Which intervention may be most effective for Muller-Weiss Disease?
2 MD, Department of Surgery, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada, Email: rocio_pasache@hotmail.com
3 Senior Physical therapist, King Fahad Specialist Hospital, Dammam, Eastern Province, Saudi Arabia, Email: mishaal.khaldi@kfsh.med.sa
4 Orthopedic consultant, Department of orthopedic surgery, King Fahad Specialist Hospital, Dammam P.O.Box 15215 Dammam 31444, Saudi Arabia, Email: alsayel002@gmail.com
Received: 25-Mar-2022, Manuscript No. jotsrr-22-58432; Editor assigned: 27-Mar-2022, Pre QC No. jotsrr-22-58432(PQ); Accepted Date: Apr 14, 2022 ; Reviewed: 11-Apr-2022 QC No. jotsrr-22-58432(Q); Revised: 13-Apr-2022, Manuscript No. jotsrr-22-58432(R); Published: 20-Apr-2022, DOI: DOI.10.37532/1897-2276.2022.17(3).71
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Muller-Weiss Disease is a rare, idiopathic, progressive condition that affects the foot, particularly the lateral aspect the navicular bone, its prevalence in males is more than females. Fortunately, the treatment can be a conservative treatment i.e. Physical therapy or a surgical intervention might be required in case physical therapy fails. In this case report we discuss a case of a female patient with Muller-Weiss Disease with the author preference of conservative and surgical technique.
https://marmarisinvestments.com
https://realestateinmarmaris.com
https://balloonsdocia.com
https://cappadociahotairballoon.org
Keywords
Muller-Weiss Disease, Navicular avascular necrosis, Talonavicular cuneiform arthrodesis, Osteoarthtis
Introduction
Muller-Weiss Disease (MWD) is a clinical foot syndrome that consists of fragmentation of lateral aspect of navicular bone, which results in a paradoxical varus flat foot [1-4]. It is more common in females (73%) between fifth and sixth decade of life, it usually occurs bilateral [5].
The disease was first described by Walther Muller, a German surgeon who found the first image of a fragmented tarsal navicular during First World War, and Konrad Weiss, an Austrian radiologist who worked with Kienbock. He thought that the disease had a similar cause of the osteonecrosis.This theory was rejected years later. MWD is managed initially with conservative treatment that usually includes activity modification, pain control and orthotics. If conservative treatment fails, surgical treatment could be considered. The options of surgical treatment were previously studied including isolated talonavicular arthrodesis, talonaviculocuneform arthrodesis and triple arthrodesis.
In this paper we will discuss a case of a female patient with MWD and the author’s preference surgical techniques for her particular case with literature review of results and outcome.
Case Report
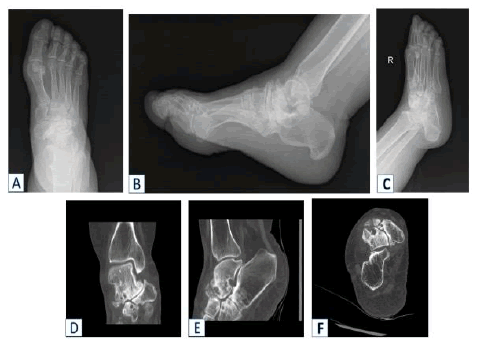
55 years old lady presented to the clinic complaining of chronic right foot pain for more than 1 year. The pain is progressive over the last months interfering with her activity of daily living. Her pain improves with over the counter analgesia. The patient denied any history of trauma. Her past medical history is positive for bronchial asthma controlled with medication and osteoporosis on anti-osteoporosis medication. Upon physical examination of the right foot, the hind foot is in valgus position, a collapsed medial longitudinal arch. Medial midfoot tenderness with restricted range of motion of midtarsal joint. Painful restricted range of motion of ankle and subtalar joint. A weight bearing lateral radiograph of the right foot showed a large dorsal protrude fragment extending over the navicular bone, degenerative change over talonavicular, naviculo-cuneiform, subtalar joint.The anteroposterior view of the right foot showed the navicular compressed in its lateral half with associated degenerative changes at the talonavicular and navicular-cuneiform joints. The first metatarsal appeared to have a relative shortening because of the fragmented navicular. SPECT scans were obtained to better outline the moderately large osseous fragment on the dorsolateral aspect of tarsal navicular bone, which looked to be articulated with both the talus and the tarsal navicular. Advanced osteoarthritic changes involving the right talonavicular joint naviculo-cuneiform, subtalar joint were also noted. Surgical option was advised to the patient after she tried all conservative treatments and she agreed to proceed with the surgery (Figure 1).
SURGICAL TECHNIQUE
Surgical intervention was done under general anesthesia, patient was placed in supine position, prepping and draping was done under aseptic technique, tourniquet inflated. Sinus tarsi approach utilized to access the subtalar joint, debridement of sinus tarsi and arthrotomy of subtalar joint, mobilization of the joint with the chisel. Furthermore, subtalar joint cartilage was denuded and articular surface was prepared with microfracture to promote fusion. 2nd skin incision was made medial to the extensor hallucis longus tendon extending from the talonavicular joint to the first metatarsal cuneiform joint. Subperiosteal dissection was carried out over the dorsal neck of the talus, the tarsal navicular, and over the cuneiforms. Identification of large fragment of the navicular bone, consisting of approximately 40% of the volume of the navicular, was extruded dorsally and laterally. This fragment was excised, large cyst with 2 cm diameter identified in the talar head, debridement of the necrotic bone and the cystic lesion were done. The cartilage was denuded from talonavicular, navicular-cuneiform and inters cuneiform joints. Allo graft used to fill the vocal defect of navicular bone.
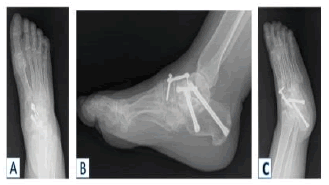
After that, two cannulated compression screws were inserted over a guide pin that had been placed under fluoroscopic control into the subtalar joint, posterior dome screw and neck screw respectively (7.5mm QWIX® Fixation Screw, Integral Life Sciences, USA ). Re-alignment of the talus, navicular, and cuneiforms, which was achieved and verified by fluoroscope control. Fusion of talonavicular, navicular-cuneiform and inter cuneiform joints and fixation with dorsal plate (Uni-CPTM compression plate, Integral Life Sciences, USA) and one two cannulated compression screws (5.5mm QWIX® Fixation Screw, Integral Life Sciences, USA ) Final c-arm fluoroscopic images were taken in the anteroposterior and lateral projections, which confirmed optimal alignment and fixation. After closure of the wound, the foot and ankle w draped with a sterile dressing. The patient was mobilized with a Aircast walker with 15 kg partial weight-bearing for 6 weeks (Figure 2).
Discussion
Muller-Weiss Disease (MWD) is a rare, idiopathic, progressive condition that affects the foot. Conservative treatment was investigated for this disease by some studies. In a retrospective comparative study that looked into the effectiveness of Conservative treatment as the first-line approach for (MWD). Both demographic and radiographic parameters were compared. MBRE sever visual analog scale (VAS) and walking disability scores were reported without change in the demographic characteristics [6]. Using custom made orthoses along with other conservative treatment methods such as magnetotherapy and bisphosphonates had positive effects. In a series case report, two patients returned to normal life after 2 to 4 months of treatment [7]. The disease has been studied in the European literature more than the American. In a study done by Maceira and Rochera at San Rafaels hospital in Barcelona, Spain, they found that 85% patients with MWD immigrate from rural regions to Barcelona in 1950 due to Spain civil war and also found a same relationship with patients from the first and second world war in Europe, establishing a malnourishment theory about this syndrome in the moment that children had to undergo ossification of their navicular, which is the last bone of the foot to ossific, around 1.5 years in girls and 2 years of age in boys [8]. Maceira conclusion is that this disease is not a necrosis of the navicular bone, in fact it is a dysplasia that develops in childhood and expresses in adulthood.
In addition, Monteagudo and Maceira described three different pathways to explain the pathogenesis of MWD:
1. “Children of war”: due to nutritional environment they did not have adequate ossification of their navicular bones making it at risk of compression stress to the articular surface.
2. Non epidemic cases: this group is usually fulfilled by athletes who had intensive training during childhood affecting the correct ossification of navicular tarsal bones.
3. “Müllerweissoid feet”: in this group the patients had healthy navicular tarsal bone until adulthood, they do not show navicular fragmentation as previous groups, they have subtalar varus and short first metatarsal that stimulates pronation of the forefoot.
Consequently, they found in the first two groups a chronological sequence from lateral compression of the navicular, which led to lateral talar head subluxation,subtalar varus, dorsal extrusion of the fragmented navicular bone (“listhesis navicularis”) and plantar flexion of the talus which correlated to all the clinical findings previously mentioned.
After identifying the etiopathogenics of the disease, clinical assessment must be done. A patient presented with chronic perinavicular painflat foot with paradoxical varus hindfoot, in the anteroposterior weight bear radiographic view.
On the radiological finding, a comma or an hourglass clock shape with compression of the lateral aspect of the navicular bone could be seen In addition to an adjacent joint arthritis depending on Maceira´s stage of the disease. Furthermore, reduction of talocalcaneal divergence and cuboid sign might be observed, which a medial subluxation of the cuboid is. In the lateral view, there was a dorsal extrusion of fragmented navicular bone and the sinus tarsi see-through sign with a plantarflexion of the talus.
In addition, Welck, Kaplan and Myerson did a case series paper recommending the use of weight bearing CT that allows to calculate how much medial column length must be restored and size of calcaneal osteotomy if required [9]. In order to have a better evaluation the author recommends taking an SPECT scan to find adjacent joints arthritis and choose best surgical treatment
The surgical treatment options are:
1. Removing the dorsal fragment of the navicular bone, this might be not a good option because this procedure could make medial column unstable [10].
2. Lateral calcaneal lengthening osteotomy.
3. Talonavicular arthrodesis.
4. Talonaviculocuneiform arthrodesis.
5. Triple arthrodesis.
The most common procedures used for treatment of MWD are Talonavicular and talonaviculocuneiform arthrodesis [11]. In a retrospective cohort study done by Harnroongroj and Chuckpaiwong, 16 patients with MDW, all achieved union in a median time of two months, 2 cases developed postoperatively naviculocuneiform arthritis.
Ahmed and coworkers conducted a study of 7 adolescent patients with MWD treated with lateral calcaneal lengthening, all of them did not have osteoarthritic changes of the joints, all of the cases achieved union with an AOFAS score of 94.2, This study had satisfactory results and it was concluded that this approach will not be an obstacle if these patients develop osteoarthritis and arthrodesis is required [12].
Isolated talonavicular arthrodesis may be considered in the absence of naviculocuneiform arthritis, but it is often associated with a high risk of nonunion. Yuan and colleagues did a study in 33 feet, 91.6% underwent isolated talonavicular arthrodesis and 8.4% had talonaviculocuneiform arthrodesis with a postoperatively AOFAS score of 83.7; they concluded that talonaviculocuneiform fusion is only considered in severe arthritis of the joint.
Lu and colleagues reviewed 19 feet in 13 patients with MWD in which they performed isolated talonavicular arthrodesis [13]. Union rate was 76.9%, 61.5% had osteoarthritic changes postoperatively from which 87.5% was from calcaneocuboid joint and/or subtalar joint. Wang and coworkers reported 6 case series 5 of them were treated with isolated talonavicular arthrodesis and one of them was treated with triple arthrodesis due to subtalar and calcaneocuboid arthritis [14].
In addition, a prospective study done by Fornaciari and coworkers [15]. 10 cases with MWD using a tension band technique with a compression plate, postoperative AOFAS score was of 88.3, they concluded this procedure could be an effective alternative treatment to provide stability when the naviculocuneiform and subtalar joints are unaffected. Additionally, Yu and colleagues made a study performing talonavicular and naviculocuneiform arthrodesis with a tricortical iliac bone block fixed with plate and screws, they achieved 100% fusion rate and AOFAS increased by 33 points postoperatively [16]. They believe their technique makes the arthrodesis more stable and has better outcome than conventional techniques. Nelson and colleagues made a case report of a patient with MWD who underwent talonaviculocuneiform arthrodesis with a postoperatively hindfoot score of 97, their judgment is that this arthrodesis adequately corrects the deformity and eliminates medial column arthritis and discusses that triple arthrodesis does not solve the problem of pain with the navicular cuneiform joints and unnecessarily restrict subtalar joint [17]. A comparative study between triple arthrodesis and talonaviculocuneiform arthrodesis done by Zhang and colleagues, they found an improvement of AOFAS SCORE to 79 postoperatively in the first group and of 86.2 in the second group with no significant difference between both [18]. They concluded that every technique has a different complication: isolated talonavicular arthrodesis usually fails and has more risk on non-union, triple arthrodesis has better consolidation but does not solve the naviculocuneiform arthritis and talonaviculocuneiform arthrodesis can have a non-union of one of the joints and if it develops a second surgery is mandatory. Other authors preferred to avoid arthrodesis, Tosun and colleagues reported a case of a patient with MWD and because of the negative effects on gait they chose to avoid arthrodesis and they just did debridement of the navicular and used cancellous autologous bone grafting to fulfill the defect [19]. However, the deficient of this study is a one patient case and also short term follow up. In regards of the grafts being used for the arthrodesis, Tan and colleagues completely removed the navicular tarsal bone and used a remodeled femoral head allograft to fulfill the defect and then make the talonavicularcuneiform arthrodesis [20]. Cao and coworkers made a 9 patient report of a reverse V-shaped osteotomy and used tricortical autologous bone graft [21].
Moreover, Fernandez de Retana and colleagues removed the fragmented navicular bone and used a trapezoid autologous graft to occupy the defect; these studies had complete consolidation in all cases [22]. Also supported by Mayich who in his systematical review emphasized that autograft remains the gold standard for biomechanical support and comprehensive healing factors [23]. Finally, Mohiuddin et al. made a review discussing a current finding about MWD. He concluded that in advanced stages, talonaviculocuneiform arthrodesis with or without hind foot correction is the best surgical option [24]. But it was also mentioned that the information is still inconclusive about this topic and there is no a standard approach yet. In our case, we chose to do a talonaviculocuneiform, intercuneiform and subtalar arthrodesis, we made that decision based on the results of the SPECT CT scan that showed arthritis in those joints and with the help of subtalar arthrodesis, we managed to correct the subtalar varus that is always present in the MWD.
Conclusion
There is no consensus on the surgical treatment for MWD; in the present case we made a different approach in order to restore all the affected joints by the disease. The goals of the surgical treatment is to achieve a pain-free, plantigrade and well aligned foot and for that reason the assessment has to be personalized and specific for the patient treated.
REFERENCES
- Harnroongroj T., Chuckpaiwong B.: Müller-Weiss Disease: Three- to Eight-Year Follow-Up Outcomes of Isolated Talonavicular Arthrodesis. J Foot Ankle Surg. 2018; 57: 1014-1019 [Google scholar] [Crossref]
- Maceira E., Rochera R.: Müller-Weiss disease: clinicaland biomechanical features. Foot Ankle Clin. 2004; 9:105-125. [Google scholar][Crossref]
- Monteagudo M., Maceira E.: Management of Müller-Weiss disease. Foot Ankle Clin. 2019; 24:89–105. [Google scholar][Crossref]
- Mohiuddin T., Jennison T., Damany D.: Müller-Weiss Disease: Review of current knowledge. Foot Ankle Surg. 2014; 20:79-84 [Google scholar] [Crossref]
- Chiavegatti R., Canales P., Saldias E., et al.: Earliest Probable Case of Mueller-Weiss Disease From Ancient Egypt.J. Foot Ankle Surg. 2018; 57:1034-1036 [Google scholar][Crossref]
- Harnroongroj T., Tharmviboonsri T., Chuckpaiwong B.: Müller-Weiss Disease: The Descriptive Factors of Failure Conservative Treatment. Foot Ankle Int. 2021; 24:1022-1030. [Google scholar][Crossref[
- Volpe A., Monestier L., Malara T., et al.: Müller-Weiss disease: Four case reports. World J. Orthop. 2020; 11:507-515. [Google scholar][Crossref]
- Couturier S., Gold G.: Imaging Features of Avascular Necrosis of the Foot and Ankle. Foot Ankle Clin. 2018; 24:17-33. [Google scholar][Crossref]
- Welck M., Kaplan J., Myerson M.: Müller-Weiss Syndrome Radiological Features and the Role of Weightbearing Computed Tomography Scan.Foot Ankle Spec. 2016; 9:245-251. [Google scholar][Crossref]
- Nuñez S.M., Maceira S.E., Fernández R.P.: Müller-Weiss disease. Foot ankle j. 2007; 12:46-55 [Google scholar] [Crossref]
- Yuan C., Wang C., Zhang C.: Derotation of the Talus and Arthrodesis Treatment of Stages II-V Müller-Weiss Disease: Midterm Results of 36 Cases.Foot Ankle Int. 2019; 40:1-9. [Google scholar][Crossref]
- Ahmed A., Kandil M., Tabl E.: Preliminary Outcomes of Calcaneal Lengthening in Adolescent Flatfoot in Müller-Weiss Disease. Foot Ankle Int. 2019; 40: 1-5. [Google scholar] [Crossref]
- Lu C., Fu Y., Cheng Y., et al.: Isolated talonavicular arthrodesis for Müller-Weiss disease.Kaohsiung J. Med. Sci. 2014; 30:471-476 [Google scholar][Crossref]
- Wang X., Ma X., Zhang C., et al.: Flatfoot in Müller-Weiss syndrome: a case series.J. Med. Case Rep. 2012; 6:228 [Google scholar] [Crossref]
- Fornaciari P., Gilgen A., Zwicky L., et al.: Isolated Talonavicular Fusion With TensionBand for Müller-Weiss Syndrome. Foot Ankle Int. 2014; 35:1316-1322 [Google scholar] [Crossref]
- Yu G., Zhao Y., Zhou J., et al.: Fusion of Talonavicular and Naviculocuneiform Joints for the Treatment of Müller-Weiss Disease. J. Foot Ankle Surg. 2012; 51:415–419. [Google scholar] [Crossref]
- Nelson E., Rivello G.: Muller-Weiss Disease of the Tarsal Navicular: An Idiopathic Case.J. Foot Ankle Surg. 2012; 51:636–641 [Google scholar][Crossref]
- Zhang H., Li J., Qiao Y., et al.: Open triple fusion versus TNC arthrodesis in the treatment of Mueller-Weiss disease.J. Orthop. Surg. Res. 2017; 12 [Google scholar][Crossref]
- Tosun B., Al F., Tosun A.: Spontaneous Osteonecrosis of the Tarsal Navicular in an Adult: Mueller-Weiss Syndrome.J. Foot Ankle Surg.2011; 50:221-224 [Google scholar] [Crossref]
- Tan A., Smulders Y.C., Zöphel O.T.: Use of remodeled femoral head allograft for tarsal reconstruction in the treatment of Müller-Weiss disease. J Foot Ankle Surg. 2011; 50:721-726. [Google scholar] [Crossref]
- Cao H.H., Lu W.Z., Tang K.L.: Isolated talonavicular arthrodesis and talonavicularcuneiform arthrodesis for the Müller-Weiss disease. J Orthop Surg Res. 2017; 12:83. [Google scholar][Crossref[
- Fernandez R.P., Maceira E., Fernandez J.A., et al.: Arthrodesis of the talonavicular-cuneiform joints in Müller-Weiss. Foot Ankle Clin. 2004; 9:65–72. [Google scholar][Crossref]
- Mayich J.: The Treatment of Mueller-Weiss Disease: A Systematic Approach. Tech Foot & Ankle. 2016; 15:59-73 [Google scholar][Crossref]
- Mohiuddin T., Jennison T., Damany D.: Müller-WeissDisease: Review of current knowledge.Foot ankle surg. 2014; 20:79-84 [Google scholar][Crossref]



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.