Ultrasound-guided blocks in polyfractured patients: An overview and 3 case reports
2 Department of Surgery, University of Concepcion, Chile, Email: abc@gmail.com
Received: 15-Jul-2020 Accepted Date: Aug 06, 2020 ; Published: 14-Aug-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Anesthesiology has greatly developed during the previous three decades, regularly incorporating new locoregional anesthetic techniques and taking a qualitative step forward by integrating the ultrasound guide into procedures to improve the safety of the patients.
Patients: Three clinical cases of polyfractured patients operated under regional anesthesia are presented. The first case corresponds to a right upper limb polyfractured patient that is operated under axillary block of brachial plexus. The second case is a polyfractured axial skeleton patient with a left femur fracture who is operated under femoral block. The third case corresponds to a polyfractured patient that has an unstable pelvic injury and an open fracture of the left tibia that is operated under anterior sciatic block.
Results: Regional anesthetic blocks have become a fundamental tool for performing various surgical procedures, since they offer great benefits to patients, especially when it comes to polyfractured patients.
Conclusion: Ultrasound-guided locoregional blocks provide excellent anesthesia and analgesia to polyfractured patients, making it possible to perform diverse surgical techniques and facilitating the early functional rehabilitation of the cases.
Keywords
Ultrasound-guided, regional anesthesia, axillary plexus block, femoral nerve block, sciatic nerve block, polyfractures
Introduction
Polyfractured patients are cases that have fractures of more than one specific bone or skeletal segment, either of the appendicular or axial skeletons. Polyfractured patients may have potentially life-threatening volemic and/or hematological disorders, as well as neurological injuries, consolidation disorders or functional alterations of the locomotor system capable of causing permanent sequelae [1].
Multiple fractures are produced by high-energy mechanisms, usually as a cause of traffic accidents, workplace accidents, social violence, and extreme sports. Polyfractured patients present complex luxofractures, open fractures, and eventually associated neurovascular lesions, requiring urgent treatment to stabilize their diverse traumatic lesions with transient or permanent methods.
Considering the difficulty involved in the management, transfer, and care of patients with polyfractured skeletal segments, the early fixation of their injuries is peremptory, preferring the surgical simultaneity and keeping in mind that these cases are excellent candidates for the use of regional anesthetic block in their surgical interventions [2].
Orthopedic surgery has undergone enormous development over the past three decades, constantly incorporating modern devices into its surgical arsenal that allow carrying out open or closed reductions and external or internal fixations for a wide variety of fractures whether single or multiple. At the same time, anesthesiology has been benefited by the constant clinical integration of numerous drugs, devices, and equipment that are enhanced by computer development. These make it possible to offer complex cases a wide variety of procedural options for the anesthesia and analgesia of the polyfractured patient [3].
The previous decades have been marked by the ongoing development of regional anesthesia, which has undergone a qualitative leap by incorporating ultrasound imaging to improve the quality and safety of locoregional procedures, making it possible to perform various surgical interventions in the locomotor system under specific blocks according to the present fractured lesions [4].
The oldest precedent for regional anesthetic and analgesic blocks dates back to 1884 and was an inferior dental nerve block done by Halsted [5]. However, the most significant contributions to the great development of locoregional anesthesia and analgesia have been reflected in the five editions of the reference book “The management of pain” by the pioneer of algology Prof. Bonica, whose first edition dates from 1953 [6].
Hospital Traumatologico is a monographic center dedicated to the treatment of adult patients with traumatic and orthopedic conditions of the locomotor system. In this hospital, there are performed about 7.000 major surgical interventions per year. During the last five years, an average of 92% of patients have been operated under anesthesia and/ or ultrasound-guided analgesia, therefore three representative cases have been selected to be described in this study.
Three clinical cases of polyfractured patients are surgically operated under regional anesthesia. The first case is a right upper extremity polyfractured patient that is operated under axillary block of the brachial plexus. The second case is a polyfractured axial skeleton patient with a left femur fracture who is operated by blocking the femoral nerve. The third case is a polyfractured patient with an unstable pelvic injury and an open fracture of the left leg that is operated by blocking the sciatic nerve by anterior approach.
Locoregional block procedures are performed in the anesthetic induction room which has a procedural stretcher and basic monitoring tools, instruments for cardiopulmonary resuscitation, and intralipid solution to reverse systemic toxicity due to local anesthetics. It also has a TOSHIBA® Aplio 500 TUS-A500 ultrasound machine, a Stimuplex
HNS 12 nerve stimulator BRAUN®, a Stimuplex® echogenic nerve stimulating needle, Ultra 360®, 22G × 2’’, 30º, 0.7 × 50 mm BRAUN® for axillary blocks of the brachial plexus and femoral nerve and Stimuplex® echogenic nerve stimulating needle, Ultra 360®, 20G × 4”, 30º, 0.9 × 100 mm BRAUN® for anterior sciatic nerve blocks.
Bupivacaine is used as a local anesthetic, since it has an average latency and a duration ranging from 2.5 to 20 hours, depending on the area of application and the concentration used. It is assumed that the average duration of its effect varies between 3 and 6 hours. The concentration used is Bupivacaine in solution of 0.33% and the volume used is 20 ml. (75 mg of bupivacaine+physiological serum 0.9%).
Case 1. Axillary plexus brachial block in upper limb polyfractured patient
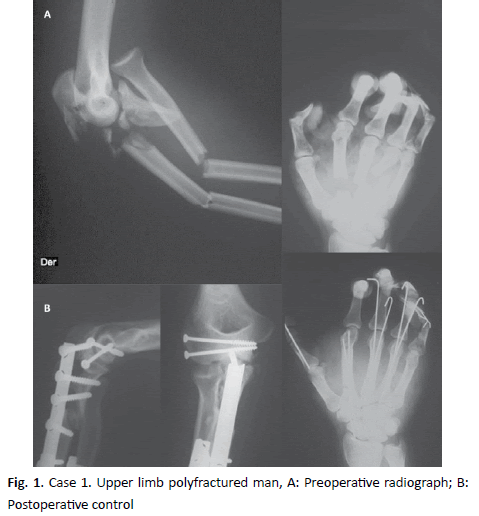
26-year-old male patient, ASA III, asthmatic with intermittent symptoms, who presents a severe crushing of his upper right limb due to a traffic accident, resulting in a complex luxofracture of the elbow, fractures of the radius and ulna of his forearm, and fractures of the metacarpals of the long fingers of the right hand (Fig. 1A).
Surgery
Open reduction and internal fixation with plate and screws in the luxofracture of the elbow and in the fractures of the right radius and ulna.
Open reduction and fixation with intramedullary Kirschner wires of right metacarpal fractures (Fig. 1B).
Anesthesia
Axillary anesthetic block of the right brachial plexus and sedation.
Anesthesiologic Technique
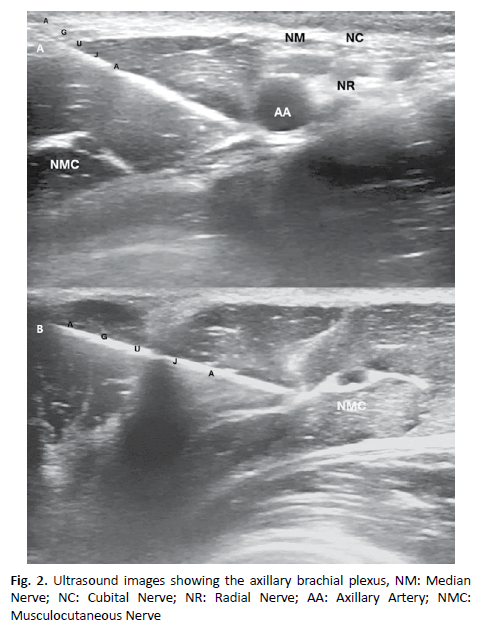
Patient in a supine position with the arm abducted at 90°, disinfection of the skin and placement of the transducer oriented with the short axis to identify the axillary artery (spherical, anechoic, throbbing, hardly compressible) which is located approximately 1 cm-3 cm. from the surface of the skin. Once the artery is identified, it is sought to locate the median, ulnar and radial nerves that are rounded or oval,
hyperechoic, or honeycomb. A prior examination should also reveal the position of the musculocutaneous nerve, on the plane between the coracobrachialis and biceps muscles or within any of the muscles. An in-plane approach is performed, inserting the needle from the top edge of the transducer from cranial to caudal, and then heading towards the backside of the axillary artery. Because nerves and vessels are positioned very close together in the vasculonervous package due to the adjacent musculature, the advance of the needle may require careful hydrodissection with a small amount of local anesthetic. This technique consists of the injection of 0.5 ml to 2 ml., which indicates the plane on which the needle tip is located. The needle is carefully advanced step by step a few millimeters at a time [7,8]. The local anesthetic should be deposited first at the back of the artery, to avoid displacing deeper structures of interest and hiding nerves, which can occur if injections for the medium or ulnar nerves are first given. The radial nerve located lower and posteriorly in relation to the artery is often more clearly visualized once surrounded by local anesthesia. After administering 5 ml to 7 ml, the needle is removed almost at the level of the skin, and is redirected to the medium (upper and anterior) and ulnar (lower and anterior) nerves; additionally, 7 ml to 10 ml. more is injected into these areas to complete the spread around the nerves. Finally, the needle is partially removed and redirected to the musculoskeletal nerve, depositing 5 ml to 7 ml. of local anesthetic. Occasionally, the musculocutaneous nerve is very close to the median nerve, making a separate injection unnecessary. In the adult patient, a successful blockade is obtained using 20 ml. of local anesthetic, although it can eventually be achieved with volumes less than this [9,10] (Fig. 2).
Blockade Distribution
\The block of the axillary brachial plexus, including the musculocutaneous nerve, results in upper limb anesthesia from the middle of the arm to the hand. The name of this block refers to its approach and not to the axillary nerve, since it moves away from the posterior cord more proximally in the axilla. The musculocutaneous nerve is easily visualized with ultrasound guidance and is reliably anesthetized with a separate injection, so it may be advisable to block it first.
Case Considerations
Regional anesthesia of the brachial plexus is performed at the axillary level bearing in mind that it is the technique of choice for elbow, forearm, and hand surgery in patients with pulmonary pathology. The level at which this block is performed avoids the risk of pleural puncture, anticipating the blockade of the phrenic nerve and the consequent hemi diaphragmatic paralysis, so that the absolute respect of lung function is obtained as a result of the procedure.
Case 2. Femoral nerve block in a polyfractured patient of axial skeleton and femur
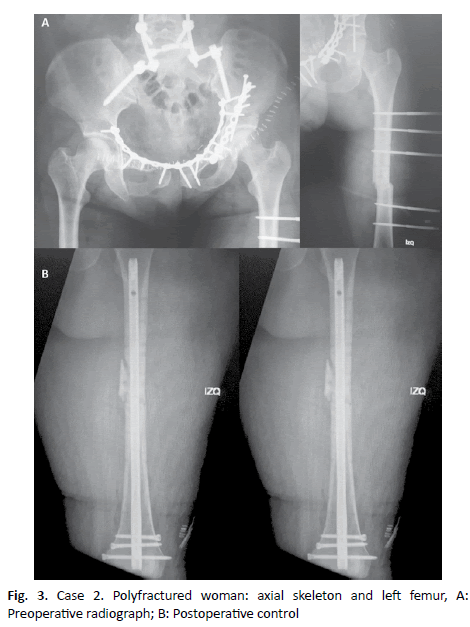
A 47-year-old woman, ASA II, BMI 36, who present an accident after falling from a high altitude, resulting in displaced lumbar spine luxofracture, unstable pelvis fracture, and left femoral diaphysis fracture. The first operation consists of performing an internal fixation of the lumbar spine and pelvis and an external fixation of the femur (Fig. 3A). A week later the patient is re-operated under locoregional anesthesia block.
Surgery
Removal of external fixator, closed reduction, and retrograde intramedullary nailing of the left femur. (Fig. 3B).
Anesthesia
Anesthetic block of femoral and left lateral femorocutaneous nerves.
Anesthesiologic Technique
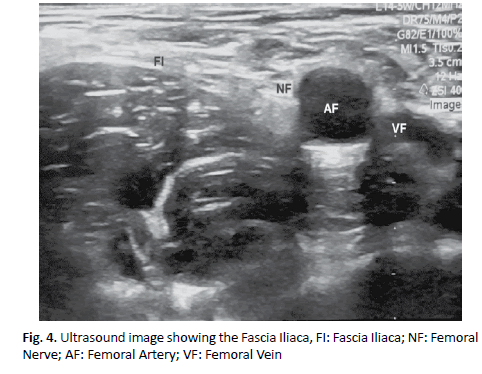
Patient in a supine position with the lower limb slightly abducted and externally rotated. The transducer is positioned to identify the femoral artery and nerve. The probe is placed in a short or transverse axis to the nerve, because it offers greater safety. If it is not possible to immediately visualize the nerve in its lateral position to the artery, the transducer can be tilted, proximally or distally, to highlight the nerve with respect to its relationship with the iliac muscle and the superficial adipose tissue. It is important to identify the iliac muscle and its fascia, as well as the fasciae latae, to avoid injection of the local anesthetic under an incorrect fascial sheath [11]. Once the femoral nerve is identified, a cutaneous injection of local anesthesia is performed 1 cm. from the side edge of the transducer, after which the needle is inserted in-plane with a lateromedial orientation, which permits to fully see the length of the needle, its tip and even its bezel. Once the end of the needle is adjacent to the femoral nerve, it is carefully aspirated, then 1 ml to 2 ml of local anesthetic are injected, whose spread confirms the proper placement of the needle. The correct injection of the local anesthetic adjacent to the femoral nerve displaces the femoral nerve from its position, confirming the correct positioning of the needle, so that the deposition of 10 ml to 15 ml of local anesthetic in an adult [12] (Fig. 4).
Blockade Distribution
Femoral nerve block produces anesthesia in the anterior and medial thigh region, including the knee, as well as in a variable skin area of the inner leg and foot region. Anesthesia and analgesia also occur in the hip, knee, and ankle joints.
Case Considerations
The choice of femoral regional anesthesia in this patient is due to the previous difficult airway management in the first surgery, obesity, with difficult airway predictors (Mallampati score, class: IV, Patil- Aldreti score-thyromentonian distance- class III: <6 cm) that increase the risk for general anesthesia; and with lumbar spine luxofracture contraindicating neuraxial anesthesia at this level [13].
Case 3. Block of the sciatic nerve by Anterior approach in a polyfractured Patient of axial skeleton and tibia
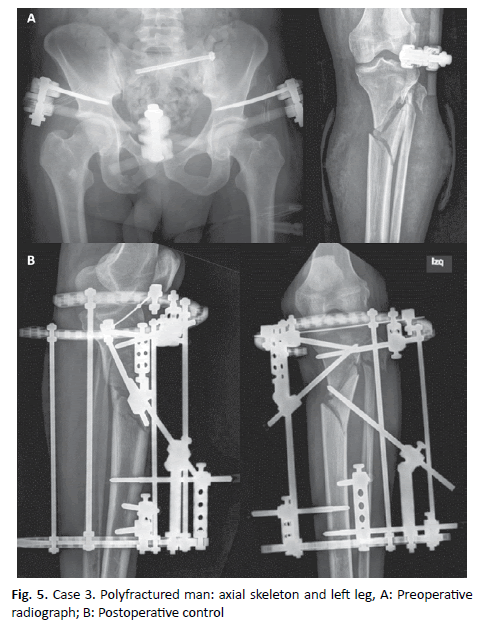
\A 55-year-old man, ASA III, with a history of smoking and Chronic Obstructive Pulmonary Disease (COPD), who presents an accident at work due to the overturning of a tractor, has an unstable fracture of his pelvis and an open fracture of his left tibia. The patient is initially operated to perform an external fixation of the pelvis and surgical debridement of the tibia fracture (Fig. 5A). A week later, he is operated again under a left sciatic nerve block by anterior approach and left femoral nerve block, to continue the treatment of his open tibial fracture.
Surgery
Surgical debridement, closed reduction, and stabilization with circular external fixator of the open fracture of the tibia (Fig. 5B).
Anesthesia
Block of the left sciatic nerve by anterior approach and left femoral nerve.
Anesthesiologic Technique
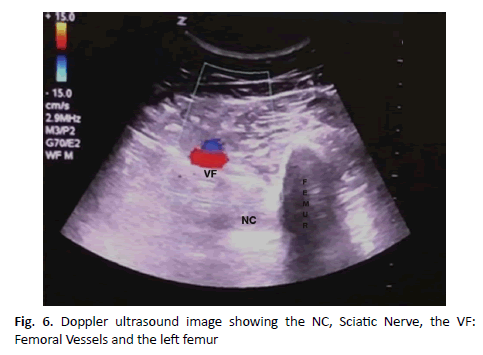
Patient in a supine position, with the hip slightly abducted and externally rotated and the knee slightly bent. The transducer is put in the axis of the limb (short axis), about 8 cm. distal to the inguinal crease, so that the sciatic nerve can be identified. If the sciatic nerve is not immediately displayed, the transducer should be slid and tilted proximally or distally until its presence is verified in the thickness of the musculature [14-16]. Subsequently, the needle is preferably inserted in-plane, from medial to lateral to avoid the presence of the femur, or outside the plane from the medial face of the thigh to the sciatic nerve if the thigh is very bulky, although in this approach the tip of the needle is hard to visualize. The contact of the end of the needle with the sciatic nerve is usually associated with a motor response in the calf or foot, plantar flexion and foot inversion for the tibial nerve, and dorsal flexion and foot eversion for the common peroneal nerve. Once it is established that the end of the needle is in the correct position, 1 ml to 2 ml. of local anesthetic are injected to confirm the proper distribution of the drug. The injection helps to delineate the sciatic nerve within its intramuscular tunnel, but the sciatic nerve can often be moved with respect to the needle. An adult patient requires an injection of 15 ml to 20 ml of local anesthetic [17] (Fig. 6).
Blockade Distribution
The block of the sciatic nerve results in anesthesia of the back of the knee, the hamstring muscles, and the entire distal lower limb to the knee,
with the exception of the skin of the medial leg and foot (saphenous nerve area, femoral nerve branch). The skin of the posterior face of the thigh is innervated by the posterior cutaneous nerve of the thigh, so this nerve is not anesthetized in the anterior sciatic block; however, the absence of anesthesia in its distribution lacks clinical consequences.
Case Considerations
The anesthetic block of the sciatic nerve is performed by anterior approach because it is a patient with chronic pulmonary pathology in which it is preferable to avoid general anesthesia, and in which the fracture of the pelvis makes it difficult to perform a technique of neuraxial anesthesia. It is complemented with an ipsilateral femoral anesthetic block to provide anesthesia on the medial face of the leg.
Discussion
Regional anesthetic blocks can be performed in different conditions of the locomotor system and can provide correct anesthesia and analgesia to certain areas and body segments, selectively interrupting the sensitive nerve conduction, a process that is established in a specific controlled, and reversible way. Therefore, one of the biggest beneficiaries of this technique have been polyfractured patients, whether these procedures are performed as exclusive anesthesia, as a regional block associated with general anesthesia or as a complementary procedure to provide adequate postoperative analgesia in cases with very complex injuries [1,2].
Locoregional blocks are a valuable alternative to general anesthesia for many surgical interventions of the locomotor system, since they offer the patient optimal operating conditions and extended postoperative analgesia that allows the early onset of the functional rehabilitation. The most relevant advantage of this technique applied to the locomotor system is the preservation of consciousness and spontaneous breathing, since it practically does not affect vegetative function. However, the use of sedative drugs is often involved, in order to offer greater comfort to the patient, especially when it is a polyfractured one [3,4].
Regional blocks are also useful in preventing phantom limb pain experienced by patients who have been amputated from an upper or lower limb, either traumatic in accidents with no chance of replantation, surgical secondary amputation in case of severe intractable fracture complications or due to peripheral vascular pathology in the lowerlimb. The prevalence of painful phantom limb can range from 30 % to 80% in lower limb amputee patients. In these cases, the preferred indication is the continuous regional block procedure by putting, by different tracts, catheters that are installed next to the target nerve of the anesthetic-analgesic block [18,19].
It should be noted that another important group of patients who benefits greatly from ultrasound-guided anesthetic and analgesic procedures are obese people, who are a continuously growing population group in our society. People with elevated BMI undergoing surgery pose specific challenges for anesthetic management, as they usually are hard to intubate. Besides, they often have latent cardiovascular disease, high blood pressure, and an increased risk of pulmonary atelectasis during surgery and postoperative intervention. They also frequently suffer from obstructive sleep apnea, which predisposes them to desaturation and hypoxemia [20].
Patients with chronic pulmonary pathology who undergo surgery are more likely to have intra and/or postoperative pulmonary complications. General anesthesia, both by the handling of the airway and by the different modalities of mechanical ventilation, has a direct impact on respiratory function, possibly producing laryngospasm, bronchospasm, aspiration pneumonitis, barotrauma, and postoperative atelectasis, among others. All of this increases morbidity rates, as well as a hospital stay.
Locoregional anesthesia interferes less with respiratory function, with the exception of supraclavicular and infraclavicular interscalene limb nerve blocks, in which there is a risk of pleural puncture that can lead to a pneumothorax, or a risk of compromising the phrenic nerve that may result in ipsilateral hemi-diaphragmatic paralysis, reducing the lung function around 25% (in the case of interscalene blocks, it can reach the 100% of the cases). That is why in the first case presented here it was decided to perform a block of the brachial plexus at the axillary level, a procedure that does not involve any of the risks described above. In addition, locoregional anesthesia provides better control of postoperative pain, and therefore facilitates respiratory function in both ASA I patients and cases with associated lung pathology. Regional anesthesia, although not exempt from risks, has benefits with respect to general anesthesia in these patients [8-21].
It should be noted that neurostimulation has been primarily responsible for the fast development of regional anesthetic blocks, using devices that send electrical impulses after puncturing a specific location with a needle-electrode. However, neurostimulation continues to be a conceptually “blind” technique, since it is performed following external anatomical references that may experience variations according to each particular patient [22].
Therefore, the inclusion of ultrasound in the performance of regional block procedures has meant a qualitative step forward in the safety of patients. The pioneers in the introduction of this technique were La Grange, Ting, and Kapral, who published the first experiences describing the successful use of ultrasonography in the performance of the regional block of the brachial plexus at supraclavicular, infraclavicular and axillary level [23-25].
Among classical regional techniques, spinal anesthesia has been used as the “gold standard” to control postoperative pain in lower limb injuries. However, peripheral nerve blocks have become increasingly relevant as they reduce the incidence of adverse effects, providing comparable benefits in the control of postoperative pain. Probably one of the biggest novelties when using an ultrasound-guided regional block, with respect to spinal anesthesia, is the fact that during the procedure it is possible to observe in real-time the diffusion of the injected anesthetic at the site selected for the block [26].
The main advantage associated with regional anesthesia methods under ultrasound control is the high rate of successful procedures, with very low levels of conversion to alternative methods of anesthesia. Other advantages are the direct visualization of the neural and vascular anatomical structures, as well as the ultrasound verification of the correct placement of the needles and the spread of the anesthetic. In addition, individual blocks are less expensive than other regional
anesthesia techniques. In fact, the amortization of standard ultrasound equipment is possible after 2500-3000 peripheral blocks, which is added to the reduction of the volume of local anesthetics used that result in lower drug expenditure. The disadvantages associated with regional anesthesia methods with ultrasound are the high upfront costs of equipment and the need for anesthesiologists to do specific training, in order to perform peripheral block techniques safely [4].
In 2015, the Cochrane systematic review assessing the use of ultrasound to guide peripheral nerve block in upper and lower limbs was published in 32 randomized controlled trials, with 2,844 adult participants, of which 26 studies rated upper limb blocks and 6 lower limb blocks. The authors concluded that peripheral nerve block performed exclusively by ultrasound guidance, or combined with neurostimulation, results in higher success rates of sensory and motor block, decreases the administration of supplement or conversion to general anesthesia, and reduces mild complications such as accidental vascular punctures or paresthesia [27].
A pediatric population is a group of growing interest as beneficiaries of ultrasound-guided regional anesthesia. For the same reason, a systematic Cochrane review was published recently in 2016 assessing the use of ultrasound guidance for perioperative neuraxial and peripheral nerve block in children, including 20 studies, with 1,241 participants, concluding that the use of ultrasound to guide the performance of neural block procedures is advantageous, particularly when used in young children, as it improves the success rate and increases the duration of the motor and sensitive block [28].
Ultrasound-guided peripheral nerve block in polyfractured patients confers excellent site-specific anesthesia and analgesia, reduces opioid requirement, and is a safe procedure. The main disadvantages are technical complexity and training to achieve and maintain proficiency in regional anesthesia procedures. As an invasive technique, peripheral
nerve block poses risks of nerve injury, vascular injury, pleural puncture, infection, and local anesthetic toxicity. It is prudent to choose general anesthesia over regional anesthesia when multiple blocks and catheters are needed. Anesthesiologists performing regional anesthesia must have a thorough knowledge of local anesthetics pharmacology and of pathophysiology changes in polyfractured patients, detecting especially potential compartment syndrome and coagulation abnormalities [29].
Conclusion
Ultrasound-guided locoregional blocks provide excellent anesthesia and analgesia to polyfractured patients, making it possible to perform diverse surgical techniques and facilitating the early functional rehabilitation of the cases. Ultrasound-guided regional anesthesia requires a skilled anesthesiologist, as well as a compliant patient, a compliant surgeon, a quiet environment, and enough time.
Level Of Evidence
Level 4
Funding
No
Conflict Of Interest
None
Ethical Responsibilities
The authors state that the procedures were followed according to the World Medical Association’s Declaration of Helsinki.
The authors state that they have followed their center protocols on publishing patient data, right to privacy and informed consent.
REFERENCES
- Banerjee M., Bouillon B., Shafizadeh S., et al.: Epidemiology of extremity injuries in multiple trauma patients. Injury. 2013;44:1015-1021.
- Clark L., Robinson M., Varbanova M.: Role of regional anesthesia in orthopedic trauma. Anesthesiol Clin. 2014;32:789-808.
- Gadsden J., Warlick A.: Regional anesthesia for the trauma patient: improving patient outcomes. Local Reg Anesth. 2015;8:45-55.
- Slade I.R., Samet R.E.: Regional anesthesia and analgesia for acute trauma patients. Anesthesiol Clin. 2018;36:431-454.
- Olch P.D.: William S. Halsted and local anesthesia: contributions and complications. Anesthesiology. 1975;42:479-486.
- Bonica J.J.: The management of pain: with special emphasis on the use of analgesic block in diagnosis, prognosis and therapy. 1st Edition 1953. Ed. Lea and Febiger. Philadelphia. USA.
- Casati A., Danelli G., Baciarello M., et al.: A prospective, randomized comparison between ultrasound and nerve stimulation guidance for multiple injection axillary brachial plexus block. Anesthesiology. 2007;106:992-996.
- Chan V., Perlas A., McCartney C., et al.: Ultrasound guidance improves success rate of axillary brachial plexus block. Can J Anaesth. 2007;54:176-182.
- Bloc S., Mercadal L., Garnier T., et al.: Comfort of the patient during axillary blocks placement: A randomized comparison of the neurostimulation and the ultrasound guidance techniques. Eur J Anaesthesiol. 2010;27:628-633.
- Bernucci F., Gonzalez A.P., Finlayson R.J. et al.: A prospective, randomized comparison between perivascular and perineural ultrasound guided axillary brachial plexus block. Reg Anesth Pain Med. 2012;37:473-477.
- Casati A., Baciarello M., Di Cianni S., et al.: Effects of ultrasound guidance on the minimum effective anaesthetic volume required to block the femoral nerve. Br J Anaesth. 2007;98:823-827.
- Ishiguro S., Yokochi A., Yoshioka K., et al.: Technical communication: anatomy and clinical implications of ultrasound-guided selective femoral nerve block. Anesth Analg. 2012;115:1467-1470.
- Chantzi C., Saranteas T., Zogogiannis J., et al.: Ultrasound examination of the sciatic nerve at the anterior thigh in obese patients. Acta Anaesthesiol Scand. 2007;51:132-.
- Chelly J.E., Delaunay L.: A new anterior approach to the sciatic nerve block. Anesthesiology. 1999;91:1655-1660.
- Ota J.U., Sakura S., Hara K., et al.: Ultrasound-guided anterior approach to sciatic nerve block: A comparison with the posterior approach. Anesth Analg. 2009;108:660-665.
- Yoshida T., Nakamoto T., Hashimoto C., et al.: An ultrasound-guided lateral approach for proximal sciatic nerve block: A randomized comparison with the anterior approach and a cadaveric evaluation. Reg Anesth Pain Med. 2018;43:712-719.
- Vloka J.D., Hadzic A., April E., et al.: Anterior approach to the sciatic nerve block: the effects of leg rotation. Anesth Analg. 2001;92:460-462.
- Karanikolas M., Aretha D., Tsolakis I., et al.: Optimized perioperative analgesia reduces chronic phantom limb pain intensity, prevalence, and frequency: A prospective, randomized, clinical trial. Anesthesiology. 2011;114:1144-1154.
- Aladin H., Jennings A., Hodges M., et al.: Major lower limb amputation audit-introduction and implementation of a multimodal perioperative pain management guideline. Br J Pain. 2018;12:230-237.
- Nielsen K.C., Guller U., Steele S.M., et al.: Influence of obesity on surgical regional anesthesia in the ambulatory setting: an analysis of 9038 blocks. Anesthesiology. 2005;102:181-187.
- Hausman M.S., Jewell E.S., Engoren M.: Regional versus general anesthesia in surgical patients with chronic obstructive pulmonary disease: does avoiding general anesthesia reduce the risk of postoperative complications? Anesth Analg. 2015;120:1405-1412.
- Hadzic A., Vloka J.: Peripheral nerve stimulator for unassisted nerve blockade. Anesthesiology. 1996;84:1528-1529.
- La Grange P., Foster P.A., Pretorius L.K.: Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus block. Br J Anaesth. 1978;50:965-967.
- Ting P.L., Sivagnanaratnam V.: Ultrasonographic study of the spread of local anaesthetic during axillary plexus block. Br J Anaesth. 1989;63:326-329.
- Kapral S., Krafft P., Eibenberger K., et al.: Ultrasound-guided supraclavicular approach for regional anesthesia of the braquial plexus. Anesth Analg. 1994;78:507-513.
- Berninger M.T., Friederichs J., Leidinger W., et al.: Effect of local infiltration analgesia, peripheral nerve blocks, general and spinal anesthesia on early functional recovery and pain control in unicompartmental knee arthroplasty. Musculoskelet Disord. 2018;19:249-253.
- Lewis S.R., Price A., Walker K.J., et al.: Ultrasound guidance for upper and lower limb blocks. Cochrane Database Syst Rev. 2015.
- Guay J., Surehsh S., Kopp S.: The use of ultrasound guidance for perioperative neuraxial and peripheral nerve blocks in children. Cochrane Database Syst Rev. 2019.
- Prasad G.V., Khanna S., Sharma V.: Peripheral nerve blocks in trauma patients: Recent updates and improving patient outcomes: A narrative review. Indian J Pain. 2020;34:8-14.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.