Total hip arthroplasty in a case of ochronotic hip arthropathy: A case report
2 Department of Pathology, SRM Medical College Hospital and Research Centre, India, Email: abc@gmail.com
Received: 21-Oct-2020 Accepted Date: Nov 17, 2020 ; Published: 26-Nov-2020, DOI: 10.37532/1897-2276.2021.16(1).1
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Ochronosis is a rare inherited metabolic disorder caused by disturbance in tyrosine metabolism. It manifests as deposition of dark pigments in connective tissues and articular cartilage leading to arthropathy. Arthroplasty gives good functional outcome in severe ochronotic arthropathy. Case Report: A 56 years old female was admitted with advanced arthritis of left hip secondary to ochronosis. Total hip arthroplasty was performed. The results of the surgery in this patient was satisfactory. Conclusion: The functional result of total hip arthroplasty in ochronotic arthropathy is similar to primary osteoarthritis. Both cemented and uncemented hip arthroplasties have similar outcome in these hips.
Keywords
ochronosis, homogentisic oxidase, hip arthropathy, total hip arthroplasty
Introduction
Alkaptonuria, first described by Virchow in 1866, is the first designated hereditary metabolic disorder with autosomal recessive inheritance. It has a rare occurrence of 1 in 2.5 lakhs to 1 in 10 lakhs population [1]. Males and females are equally affected.
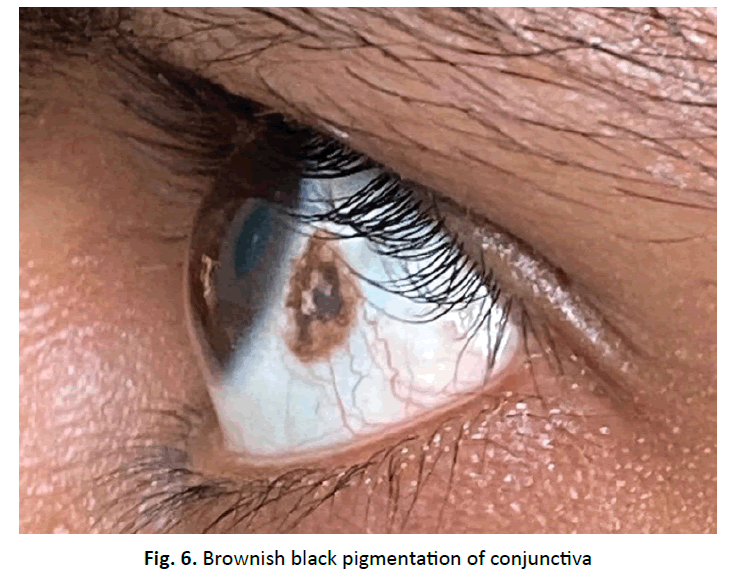
Absence of homogentisate oxidase leads to accumulation of homogentisic acid in connective tissues called as ochronosis [2]. It has high affinity to proteoglycans of hyaline cartilage and hence the deposition in pinnae, sclera, intervertebral discs, menisci, tendons and articular surfaces. HGA, present in the urine turns it black on oxygenation or alkalinization due to the formation of benzoquinone acetic acid.
The treatment is mainly symptomatic and supportive. Surgical treatment in the form of synovectomy, arthroscopic debridement and arthroplasty provides patients with painless range of motion in ochronotic arthropathy. Here, we report a case of 55-year-old female of ochronotic hip arthropathy treated with total hip replacement of the left hip.
Case Report
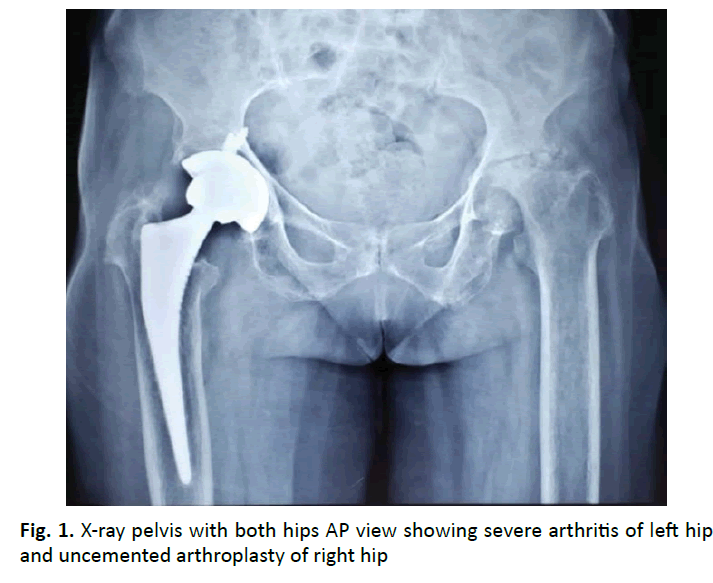
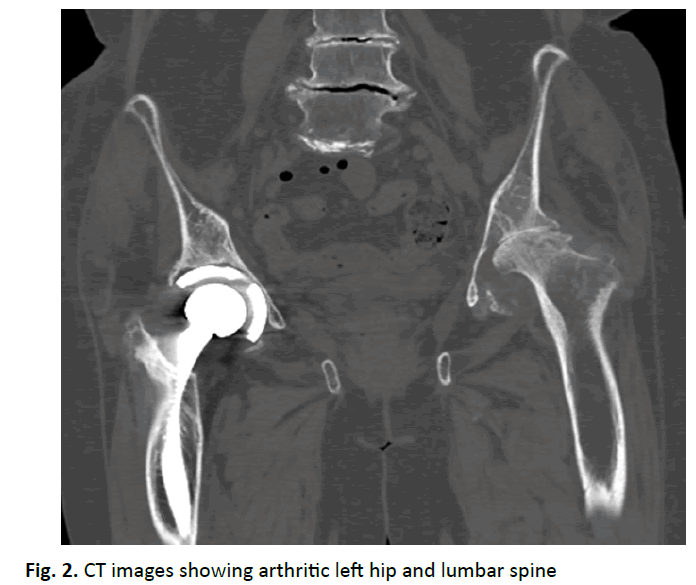
A 55-year-old female presented with complaints of left hip pain and difficulty in walking for the past 8 months. Patient had undergone total hip arthroplasty on right side for severe osteoarthritis 4 years back elsewhere. Clinically, there was 4 cm shortening and gross restriction of range of movements. Plain radiographs and CT scan of bony pelvis revealed severe osteoarthritis of left hip (Fig. 1 and 2). Patient was planned for cemented total hip arthroplasty of left hip.
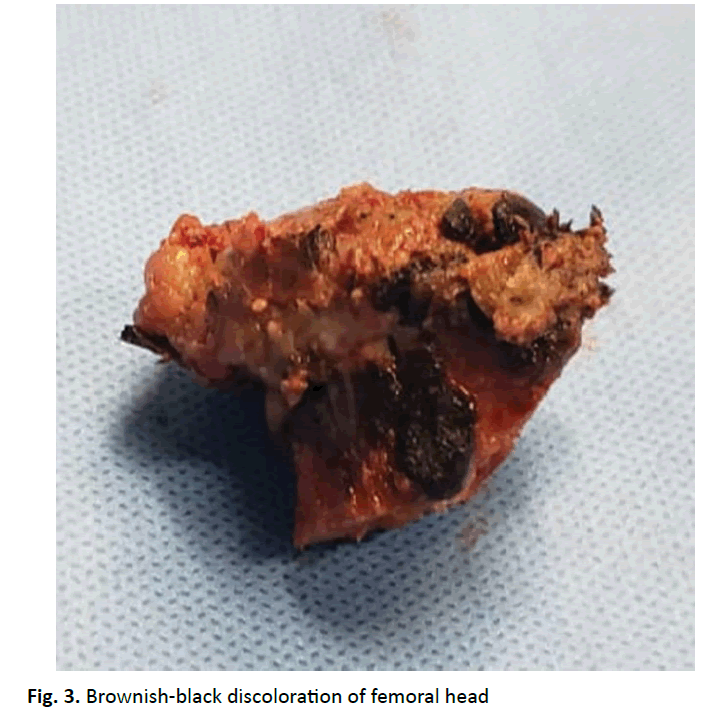
Surgery was done using posterolateral approach under spinal anesthesia with patient in right lateral decubitus position. Per operatively capsule was found to be brownish-black in colour with firm consistency. Capsule was excised completely. Femoral head was delivered with difficulty and found to be deformed with brownish-black discoloration (Fig. 3). Cemented total hip arthroplasty was done. The hip joint was reduced and found stable intraoperatively.
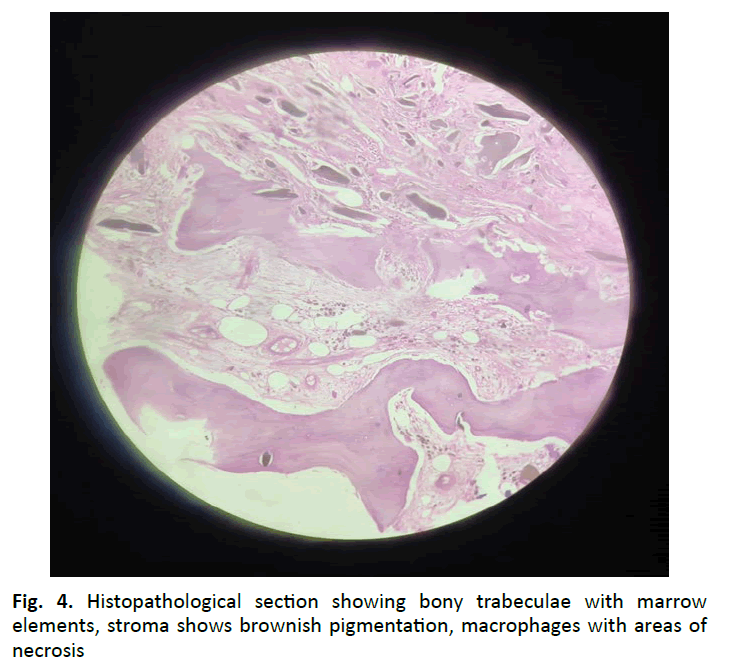
Histopathological examination of the femoral head showed bony trabeculae enclosing fibrocollagenous stroma, marrow elements and adipocytes exhibiting numerous crystalline structures (Fig. 4). These structures were brown to black in colour, irregularly shaped with sharp edges. The surrounding stroma showed numerous pigmented macrophages along with mild inflammation confirming the diagnosis of ochronosis.
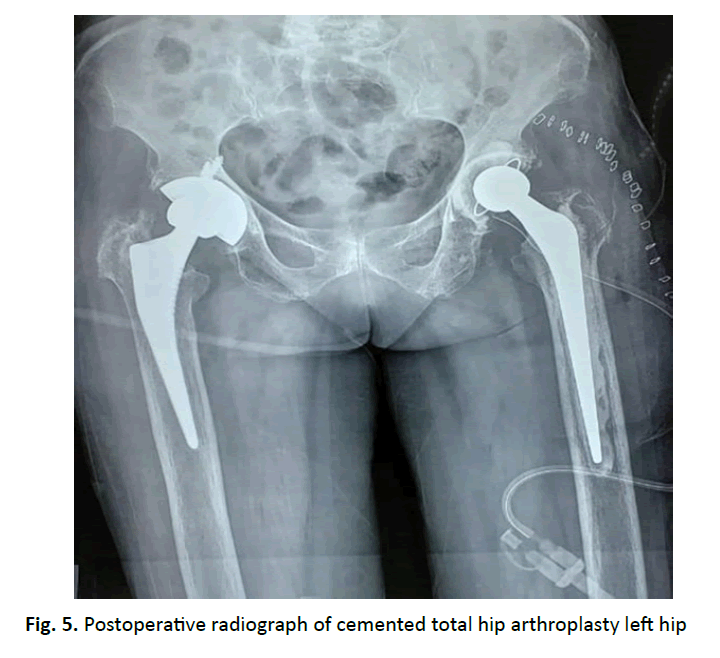
Postoperative radiograph showed prosthesis in satisfactory position (Fig. 5). Active SLR and abduction exercises started. Ophthalmology opinion postoperatively stated about the blackish patches over the conjunctiva (Fig. 6). At 2 years follow up Harris hip score was 75 and patient was able to carry out her daily activities without much pain.
Discussion
40% of patients with alkaptonuria are asymptomatic. The clinical features usually occur in 3rd-4th decade of life. The skeletal manifestations commonly seen are secondary osteoarthritis of large weight bearing joints, spondylosis, kyphoscoliosis, rupture of tendons, osteopenia and fractures. The characteristic radiographic features are calcification of intervertebral disc, menisci, pubic symphysis, nasal cartilages, pinnae, cardiac valves and great vessels.
One third of patients develop secondary osteoarthritis of larger joints like hip, knee and shoulder after 3rd decade of life. Men are severely affected than women. The biochemical quality of the articular cartilage changes and becomes brittle, leading to this arthropathy. Concentric narrowing of joint space is seen similar to primary osteoarthritis. The clinical features of pain and limping are more marked than the radiological manifestations.
Ochronotic arthropathy is usually managed conservatively. 50% of patients undergo joint surgeries in their lifetime. Ochronotic arthropathy is diagnosed frequently intraoperatively during a joint replacement surgery due to the presence of dark synovium and cartilage surfaces. In this case too while performing arthroplasty over the left hip, ochronosis was suspected after looking at the dark discoloration of the joint capsule and femoral head, which was later confirmed by the histopathological examination. In the current case, joint capsule was completely excised after suspecting ochronosis intraoperatively.
The literature regarding total hip arthroplasty for Ochronotic Arthropathy is limited. Spencer et al from their experience of 11 various arthroplasties done in 3 ochronotic patients with a follow-up of 12 years concluded that the survival rate of prosthesis is comparable to that of arthroplasty done for other indications [3]. Harun did a cemented knee replacement and uncemented hip replacement in a patient with ochronosis and concluded that arthroplasty gives excellent outcome in patients with degenerative arthritis due to ochronosis [4]. Makela et al. performed a bilateral hip arthroplasty at an interval of 8 months for a severe arthritis and presented with a painless mobile hip in follow ups [5].
Cebesoy suggested removal of the contracted anterior capsule to prevent dislocation per operatively [6]. Fernando recommended complete removal of capsule to prevent recurrence of the disease process after a hip arthroplasty [7]. Pachore et al. published their results of arthroplasty in 12 ochronotic hips with a long-term follow-up of 3 to 24 years [8]. They noticed increased blood loss in these patients and advised to avoid total synovectomy. They advocated preservation of capsule for complete closure later. We advocate capsular removal as a contracted pathological capsule will limit hip mobility.
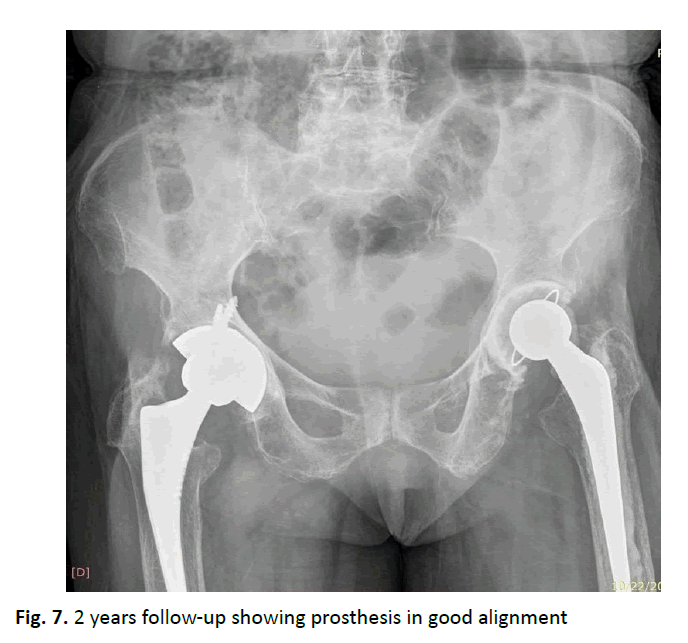
In a systematic review on total knee arthroplasty in ochronotic patients, Lee suggested using a cemented prosthesis due to the possible inflammatory nature of arthritis. In the hip, comparison between results of cemented and cementless hip arthroplasty is limited [9]. Couto in their case of hip arthroplasty diagnosed postoperatively due to alkaptonuria proceeded with cementless component as the bone seemed reasonable macroscopically [10]. Cebesoy [6] found both femoral and acetabular sides of the hip joint to be of poorquality during reaming [4]. In their case series, Pachore in view of the sclerosis of the acetabular rim, recommended usage of screws with the cup [8]. Superior pain relief with functional restoration was obtained with no radiological evidence of loosening, instability or subsidence after uncemented hip arthroplasty. However, they advised on usage of cemented hip replacement in patients with poor bone stock. They concluded that both cemented and cementless hip replacements have good survivorship in long-term. In our case both the cemented and uncemented had same functional outcome in the 2nd year and 4th year follow-up period (Fig. 7).
Conclusion
To conclude, total hip arthroplasty in ochronotic arthropathy has good outcome similar to a primary osteoarthritis. Complete capsular excision is advisable. Both cemented and uncemented hip arthroplasties have similar outcome in these hips.
Acknowledgements
No funding has been received for this study. Informed patient consent was obtained.
Conflict of Interest
The authors have no affiliations with any organization or entity with any financial interest in the subject matter discussed in this manuscript.
Author Contributions
All authors have contributed to the case report. They have read and approved the final manuscript.
REFERENCES
- Acar M.A., Erkocak O.F., Aydin B.K., et al.: Patients with black hip and black knee due to ochronotic arthropathy: case report and review of literature. Oman Med J. 2013;28:448.
- Dom K., Pittevils T.: Ochronotic arthropathy: the black hip. Case report and review of the literature. Acta Orthop Belg. 1997;63:122-125.
- Spencer J., Gibbons C.M., Sharp R., et al.: Arthroplasty for ochronotic arthritis no failure of 11 replacements in 3 patients followed 6-12 years. Acta Orthop Scand. 2004;75:355-358.
- Harun M., Hayrettin Y., Serhat M., et al.: A rare cause of arthropathy: an ochronotic patient with black joints. Int J Surg Case Rep. 2014;5:554-557.
- Makela A., Korkala O.: Hip arthroplasty for alkaptonuric ochronosis: a case report. Acta Orthop Scand. 1986;57:171-172.
- Cebesoy O., Isik M., Subasi M., et al.: Total hip replacement for an ochronotic patient: a technical trick. Am J Case Rep. 2014;15:27.
- Fernando O.S., Supreeth N., David G.D., et al.: An unusual case of bilateral ochronotic arthropathy of the hip successfully managed by a staged bilateral total hip replacement-an insight with a surgical note. JOCR. 2018;8:11.
- Pachore J.A., Shah V.I., Upadhyay S., et al.: Primary hip arthroplasty for the treatment of alkaptonuric hip arthritis: 3-to 24-year follow-ups. Arthroplasty. 2019;1:8.
- Lee W.C., Tan T.L., Chan Y.H.: Total knee arthroplasty in ochronosis arthropathy: a case report and systematic review. Case Rep Orthop. 2019;9:2019.
- Couto A., Sa Rodrigues A., Oliveira P., et al.: Ochronotic arthropathy-a rare clinical case. OMCR. 2018:omy069.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.