Total Elbow Replacement For Post-Traumatic Loss Of Elbow Movement -A Case Series
2 Hanoi Medical University, Hanoi, Vietnam
Received: 07-Jun-2021 Accepted Date: Jun 20, 2021 ; Published: 30-Jun-2021, DOI: 10.37532/1897-2276.2021.16(1).24
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This research summarized 7 clinical cases of total elbow replacement in 2 male and 5 female patients treated for posttraumatic elbow immobility. Preoperative Mayo elbow performance score was poor with 49 points. The mean age was 37.2 and the mean postoperative observation time was 9 months. After surgery, mean elbow flexion and extension arc gained 110 and 2 degrees respectively, mean elbow range of motion arc was 108 degrees, active forearm pronation and supination arc was 74 degrees and 63 degrees respectively. Mayo elbow performance score was excellent with 94 points. All 7 patients were completely satisfied with the results. Many other reports about elbow replacement treating for posttraumatic restricted elbow movement showed positive results with improvement of elbow range of motion in various degrees. In Vietnam, elbow joint replacement is still a new treatment method. Therefore, it is necessary to have a plan for pre-operative preparation and comprehensive postoperative management of the patients in order to achieve the best outcomes.
Keywords
total elbow replacement, elbow immobility, post-trauma sequelae
Introduction
In 1925, the first attempt to replace an elbow joint was conducted by Robineau, using an unconstained joint for a 20-year-old patient who had presented with distal part defect of the humerus. This type of joint was designed from metal and vulcanized rubber. In 1941, Boerema introduced a hinged prosthesis completely made of metal, which paved a way for development of later generations of artificial elbow joint [1,2].
In 1947, hemiarthroplasty of human elbow was first described by Mellen and Phalen for pseudo-joints or malunions of distal portion of the humerus [3]. In early 1970, Dee was the designer of the linked hinged elbow joint, and in 1972 he reported the results of 12 cases of elbow replacement with this joint generation [4].
In situations of post-traumatic longterm sequela disorder of the elbow, there are numerous treatment options available, including rehabilitation, open surgery, and elbow arthroscopy. However, in severe cases such as full sticking of the elbow joint resulting in stiffness or cases of elbow bone defect causing loss of elbow movement, the preceding approaches cannot help restore elbow movement optimally. For these patients, elbow replacement is the best option to increase the amplitude range of elbow joint mobility [5,6]. We present 7 clinical cases with severe sequelae after trauma causing loss of active elbow movement who received a total elbow replacement. In which, There are 4 cases used available standard hinge joints, 3 cases needed to design personalized joints. After 9 months, the average follow-up time with the outcome of elbow joint amplitude has significantly improved.
Case Presentation
This case-study review 7 post-trauma sequelae cases, including 4 cases of complete elbow stiffness and 3 cases of complete elbow instability. All of the patients were unable to move and do activities actively with their injury joint, which severely affected quality of life. All cases underwent at least 1 previous surgery to improve mobility but were unsuccessful.
Surgical history of 7 clinical cases before their elbow replacement:
Case 1: A 30-year-old female patient who was diagnosed with a left elbow injury for 30 months and a left Monteggia fracture had 4 operations before the elbow replacement surgery. The first surgery was an ulnar osteosynthesis. Following that, the patient developed pseudarthrosis on the ulnar and undergone second surgery, using combination of bone graft and screw bone. After the second surgery, the patient developed an infection of the incision, requiring a third surgery to clean the infection and place antibiotic cement. The fourth surgery was performed to remove the antibiotic cement, afterwards, the patient received no further treatment. The patient was free of infection after the fourth surgery and came to our hospital for treatment.
Case 2: A 51-year-old female patient who was diagnosed with a left elbow injury for 12 months, with сombined trauma: rib fracture, shoulder blade fracture, complex fracture of the elbow bone and humerus fracture, peeling skin from humeral to forearm. The patient underwent osteosynthesis of the left humerus, fix the left elbow joint, and patch the skin covering the left humeral and forearm at another facility before our elbow replacement surgery.
Case 3: A 18-year-old male patient who was diagnosed with a left elbow injury for 10 months, left humerus distal head fracture, had 3 previous surgeries. In which, the first surgery was osteosynthesis of the distal humerus, the second surgery treated the humeral pseudarthrosis, the third surgery performed surgical release of the elbow stiffness but showed no significant improvement.
Case 4: A 46-year-old female patient who was diagnosed with a right elbow joint injury for 6 months. First surgery was to fix the old dislocation, but no improvement. The patient came to us with a loose elbow joint, severe degeneration and complete instability.
Case 5: A 35-year-old female patient who was diagnosed with a left elbow injury for 15 years, distal left humerus fracture, had four surgery before our elbow replacement surgery. The first surgery was a distal humerus osteosynthesis. Afterwards, the patient developed elbow osteoarthritis and distal humeral pseudarthrosis. The second surgery was osteosynthesis, grafting distal humerus, surgical release of the elbow stiffness. After the operation, the elbow joint was completely fused into one block, the distal humerus was missing, the third surgery was performed to remove the screw brace and to release the elbow stiffness but no significant improvement.
Case 6: A 32-year-old female patient, who was diagnosed with a left elbow injury for 30 years and a complex fracture of the elbow and wrist, had four surgeries before our elbow replacement surgery. The first surgery was an osteosynthesis of the elbow and wrist, the second one was a bone graft surgery to treat pseudarthrosis condyle of the humerus, remove the wrist joint. The third surgery was a surgical release of the wrist stiffness and elbow stiffness, along with the removal of the screw brace. After the third surgery, the muscles of the humerus and forearm began to atrophy. The fourth surgery was a surgical release of the elbow stiffness but showed no significant improvement, afterwards, the arm and forearm suffered from severe muscle atrophy, osteoporosis and thin bone wall.
Case 7: A 43-year-old male patient who was diagnosed with a right elbow injury for 30 years, complicated fracture of the elbow, had two surgeries before the elbow replacement surgery, first surgery was an osteosynthesis. Afterwards, the patient developed elbow osteoarthritis, the second surgery was implant removal and surgical release of the elbow stiffness but no significant improvement.
The above are the surgical history of all clinical cases before their elbow replacement. The range of motion of the elbow joint before and after the operation is summarized in table 1.
| Ordinal number | Patients | Preoperative range of motion | Postoperative range of motion |
|---|---|---|---|
| 1 | Female, 35 years old, 30 months of elbow injury, proximal ulnar defect | Elbow instability, incapable of active elbow flexion and extension. | 10 month after megaprosthetic elbow replacement for proximal ulnar defect: |
| 70 degrees pronation, 50 degrees supination | Â 130 degrees flexion, 0 degrees extension | ||
| Mayo score: 55 points | Â 70 degrees pronation, 50 degrees supination | ||
| Â Mayo score: 100 points | |||
| 2 | Female, 51 years old, 12 months of elbow injury | Elbow stiffness at 30 degrees extension position | 12 months after standard elbow replacement: |
| 5 degrees pronation, incapable of supination | Â 120 degrees flexion, 10 degrees extension | ||
| Mayo score: 45 points | Â 70 degrees pronation, 70 degrees supination | ||
| Â Mayo score: 100 points | |||
| 3 | Male, 18 years old, 10 months of elbow injury | Elbow stiffness at 25 degrees extension position | 6 month after standard elbow replacement: |
| 40 degrees pronation, 10 degrees supination | Â 100 degrees flexion, 5 degrees extension | ||
| Mayo score: 45 points | Â 80 degrees pronation, 50 degrees supination | ||
| Â Mayo score: 85 points | |||
| 4 | Female, 46 years old, 6 months of elbow injury | Elbow instability, incapable of active elbow flexion and extension | 11 month after standard elbow replacement: |
| 60 degrees pronation, 50 degrees supination | Â 120 degrees flexion, 0 degrees extension | ||
| Mayo score: 45 points | Â 90 degrees pronation, 80 degrees supination | ||
| Â Mayo score: 95 points | |||
| 5 | Female, 35 years old, 15 years of elbow injury, distal humeral defect | Â Elbow instability, incapable of active elbow flexion and extension | 9 months after megaprosthetic elbow replacement for distal humeral defect: |
| Â 70 degrees pronation, 60 degrees supination | Â 130 degrees flexion, 0 degrees extension | ||
| Â Mayo score: 45 points | Â 80 degrees pronation, 70 degrees supination | ||
| Â Mayo score: 95 points | |||
| 6 | Female, 32 years old, 30 years of elbow injury, total muscle atrophy from arm to forearm | Â Elbow stiffness at 10 degrees extension position | 6 months after personalized elbow replacement: |
| Â 50 degrees pronation, incapable of supination | Â 50 degrees flexion, 0 degrees extension | ||
| Â Mayo score: 55 points | Â 50 degrees pronation, 50 degrees supination | ||
| Â Mayo score: 80 points | |||
| 7 | Male, 43 years old, 30 years of elbow injury | Â Elbow stiffness at 30 degrees extension position | 8 months after standard elbow replacement: |
| Â 40 degrees pronation, incapable of supination | Â 120 degrees flexion, 0 degrees extension | ||
| Â Mayo score: 55 points | Â 80 degrees pronation, 70 degrees supination | ||
| Â Mayo score: 100 points |
Table 1. Preoperative and postoperative summary of 7 clinical cases
Before surgery, 3D CT scans of elbow joints for all patients were taken to measure the expected indexes of osteotomy, from which we would decide to use whether available or newly personalized joints for each case. The type of joint we used is hinged elbow joints with a varusvalgus motion arc of a few degrees, made of titanium alloy material, manufactured by Chunli Medical, Beijing, China.
In 4 cases of elbow stiffness, on X-ray films, the olecranon was fused into a mass with the distal portion of the humerus. 1 case had had elbow stiffness since childhood and undergone 4 previous surgeries without any improvement, arm and forearm muscles were atrophied, arm and forearm bones were severely osteoporotic, medulla cavity of the humerus was really narrow, medulla cavity of the ulna was even absent and the ulnar wall was thin as well. Hence, a special joint with a small stem part was designed to fit this patient’s bones. For the remaining 3 cases, we used available standard hinge joints.
In 3 cases of total elbow instability, standard hinged elbow joint was applied for a patient with a previous elbow dislocation. Two other cases had defects of distal part of the humerus and proximal part of the ulna respectively, we had to use personalized elbow joint with compensating parts for the defects (Megaprosthesis joint) of distal part of the humerus and proximal part of the ulna.
This report describes in detail 3 typical clinical cases out of 7 cases.
Three typical clinical cases
Clinical case 1
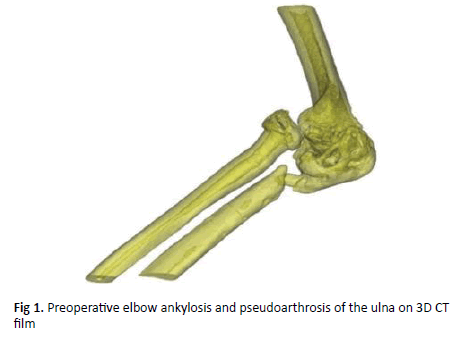
The first case is a 35-year-old female patient with past history of Monteggia left forearm fracture 30 months before hospitalization. The patient had 4 surgeries including bone fusion, bone grafting, infection clearance, antibiotic cementation and then removing the antibiotic cement. After that treatment, the patient’s arm was no longer infected, inflammatory bilan also returned to normal, however active motion of elbow joint was absent. The patient came to us in the following conditions: Total elbow instability, incapability of active flexionextension movement, 70 degrees pronation, 5 degrees supination. Mayo elbow performance score was 55 points and at a poor level, heavily affecting quality of life. There is a figure of anterior radial head dislocation, joint adhesion and proximal ulna bone defect (Figure 1).
We decided to replace the patient’s elbow with linked, unremovable hinge megaprosthesis. Personalized 3D design was based on the patient’s CT scan with an offset part for the proximal ulnar defect and made of titanium alloy material manufactured by Chunli Medical, Beijing, China.
We incised posterior skin of the elbow joint following the old scar, dissected to expose the ulnar nerve, and pushed it to the side. Exposing the elbow joint and previous ulna fracture showed complete osteoarthritis. Proximal ulnar defect was 3 centimeters in length, the radius head was dislocated and completely deformed.
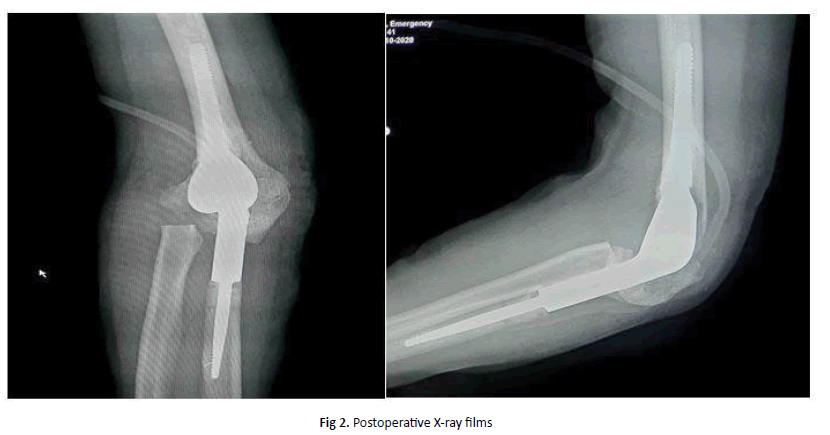
Dissect on both sides the insertion point of the triceps tendon, go to the olecranon and preserve the entire insertion point. Cut and remove radial head at the radial neck, cut the intercondylar fossa and bore the medullar cavity of the humerus. Drill and bore the medullar ulnar cavity. Drill and shape a groove at the olecranon for the artificial joint to pass through. Put antibiotic cement and the prosthesis into the medulla, then wait for the cement to harden. Intraoperative examination the elbow range of motion arc was 140 degrees of flexion, 0 degrees of extension, 70 degrees of pronation, and 70 degrees of supination. We actively moved the ulnar nerve bed forward and then sutured the incision anatomically. After surgery, the patient practiced passive flexion-extension from the second day, passive pronation-supination from the fifth day. Active exercises were conducted from the tenth day. Strength training from the fourteenth day. The patient had postoperative radiograph show that the implants are anatomically correct surficial image (Figure 2). Patients were scheduled for follow-up visits every 2 weeks. 4 weeks after surgery, elbow range of motion: active flexion and extension arc was 120 degrees and 0 degrees respectively, active pronation and supination arc was 70 degrees and 50 degrees (Figure 3). Most recent visit was 10 months after surgery, surgical scars were completely healed. Elbow range of motion: active flexion and extension arc was 130 degrees and 0 degrees respectively, active pronation and supination arc was 70 degrees and 50 degrees. Mayo elbow performance score gained excellently 100 points and the patient began to return to normal daily activities.
Clinical case 2
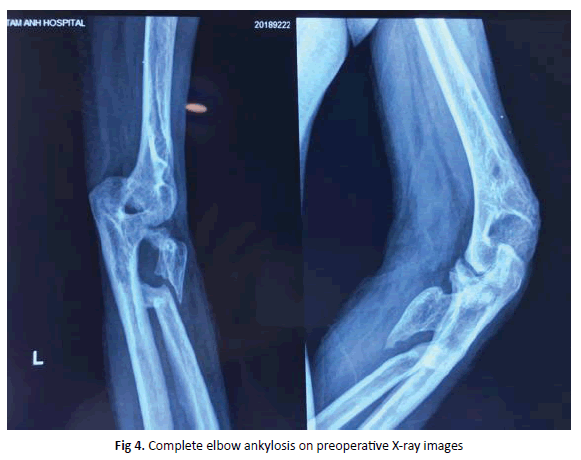
Female patient, 51 year old, suffered from a traffic accident 1 year before hospitalization and was diagnosed with multiple injuries: left rib fracture, left scapula fracture, complex fracture of left elbow area and left humerus, completely deep anterior-lateral skin tears from left arm to forearm. The patient was taken an emergency surgery for osteosynthesis of left humerus, left elbow bone fixation, combining with skin flaps covering left arm-forearm at another hospital. The patient came to us with elbow stiffness in 30 degrees loss of extension position, 5 degrees of active pronation and incapability of supination. Mayo elbow performance score was low with 45 points. Complete ankylosis of humero-ulnar joint, with a bony bridge between the proximal parts of the radius and the ulna (Figure 4).
We decided to replace the patient’s total elbow joint. The type of joint used is a standard hinged elbow joint of Chunli Medical, Beijing, China.
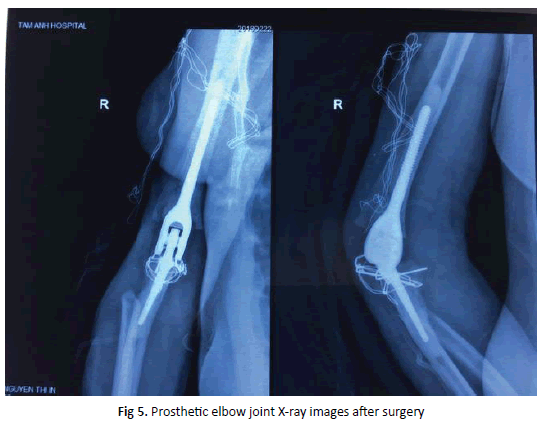
In terms of positioning and surgical technique, we still performed the same as clinical case 1, but this patient had complete ankylosis of humero-ulnar joint, so when exposing the elbow joint, we performed the technique of cutting the olecranon and keeping the insertion point of triceps tendon. After cutting the olecranon and exposing the elbow joint, we saw a proximal portion of the radius adhering to the condyle of humerus, proceeded to remove this piece of bone and the fused bony bridge was removed as well. After releasing the elbow joint and reconstructing proximal ends of the ulna and radius, we continued to drill, bore the medulla and place the prosthesis with cement. Then we proceeded to compress the olecranon with Kirschner wires and steel sutures, closed the incision anatomically. Immediate postoperative examination of elbow range of motion showed: 110 degrees passive flexion, 20 degrees extension, 70 degrees passive pronation, 60 degrees passive supination. The patient’s range of motion did not reach fully partially due to the obstruction of the stretching scars. Hence, after the incision was dry and stable, we created a skin flap to solve the stretching scars. The patient was given programmed rehabilitation exercises at home. The patient had postoperative radiograph show that the implants are anatomically correct surficial image (Figure 5).
12 months after surgery, the patient’s elbow joint range of motion improved well with: 120 degrees of active elbow flexion, 10 degrees of extension, 70 degrees of active forearm pronation, 60 degrees of active forearm supination. The Mayo elbow performance score was excellent with 100 points. The patient was completely satisfied.
Clinical case 3
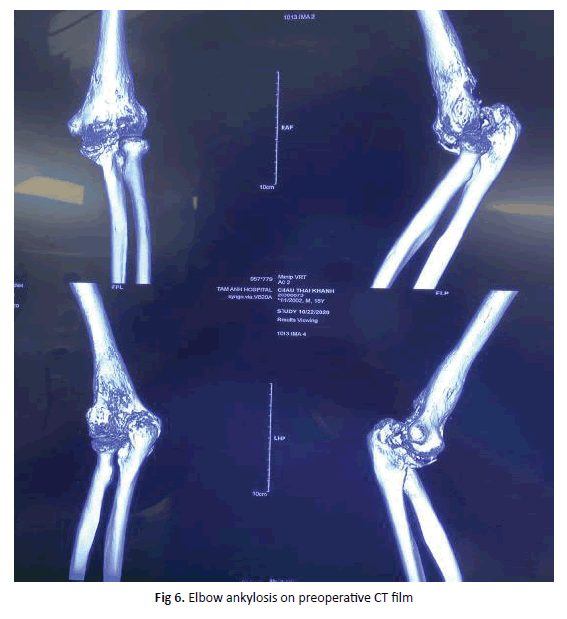
Male patient, 18 years old, had traffic collision 10 months before hospitalization. The patient was diagnosed with left distal humerus fracture, operated 3 times in which 2 times were osteosynthesis and the other was operative release of elbow ankylosis. The patient presented with stiffness of left elbow joint, 25 degrees extension, 40 degrees active pronation, 10 degrees active supination. Left elbow joint was totally degenerated and deformed, elbow ankylosis on preoperative CT film (Figure 6). Mayo elbow performance score gained 45 points.
The patient was indicated to have total left elbow replacement, using standard hinge joint by Chunli Medical, Beijing, China.
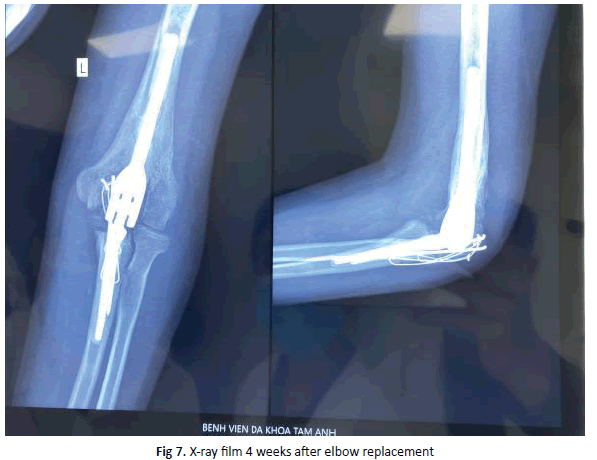
Surgery technique was performed similarly to clinical case 2; the olecranon was removed. Going into the joint, elbow joint was in total ankylosis. After removing the olecranon, we proceeded to chisel, reform the articular surfaces and other phases until joint implant. Passive examination during the surgery: 110 degrees flexion, 0 degrees extension, 80 degrees pronation, 70 degrees supination. Finally, we closed the olecranon by Kirschner wires and steel sutures; closed the incision anatomically. The patient had postoperative radiograph show that the implants are anatomically correct surficial image (figure 7).
After discharge, the patient was instructed to practice at home and get re-examinations 2 week after to control elbow joint range of motion.
At present, 6 months after surgery, elbow joint range of motion is progressing in good condition: 100 degrees active flexion, 5 degrees active extension, 80 degrees pronation, 50 degrees supination. Mayo elbow performance score gains 85 points. The patient satisfies with the result.
Discussion
Worldwide authors presumed that, for treatment of serious traumatic sequalae of elbow, such as severe osteoarthritis, total elbow stiffness, elbow ankylosis, distal humeral pseudo-joint or bone defects of elbow area, elbow replacement has been proved to be the best method to recover elbow range of motion. These authors have also had clinical reports with excellent outcomes of elbow replacement for traumatic sequalae [5,6]. Our 7 clinical cases were all severe traumatic sequala, causing incapability of active elbow movement, for example elbow instability or complete elbow stiffness. The patients underwent at least 1 surgery by various methods without any improvement. Therefore, we assumed elbow replacement was the only solution to enhance elbow function of these clinical cases.
There have been a few reports that total elbow replacement, treated for restricted elbow movement or elbow stiffness caused by traumas and others, has been positive overall, considering the improvement of elbow range of motion. According to Peden and Morrey, from 1982 to 2004, 13 patients with spontaneous elbow ankylosis were treated by semiconstrained total elbow replacement. Average operation age of the patients is 54 (24 to 80 ), mean observation time was 12 years and was estimated clinically using Mayo elbow performance score as well as X-ray images. 10 of which had posttraumatic elbow stiffness, 1 patient had juvenile idiopathic arthritis and 2 patients had rheumatoid arthritis.
Postoperative observation showed that mean elbow extension arc was 37 degrees and flexion arc was 118 degrees. The result was good or excellent in 7 patients. However, half of the patients had to be reoperated due to infection, periprosthetic fracture and elbow re-ankylosis complications. Preventive measures for abnormal calcification did not succeed [8]. These outcomes were different from ours which all 7 cases did not have any infection or prosthetic loosening complications. Our patients’ mean elbow range of motion: 2 degrees extension and 110 degrees flexion. Our patients were completely pleased.
In many elbow ankylosis situations, the original boundary between the humerus and the olecranon was challenging to identify; this was a difficulty for reconstruction of the joint and sometimes surgeons might cut at wrong positions or even cause bone fracture in the operations. Intraoperative bone fracture complications were brought up by plentiful authors [8-12]. Our patients were measured all expected indexes of osteotomy based on preoperative 3D CT scan so as to limit bone fractures complication during surgery. Our 7 cases did not present any intraoperative bone fractures.
Numerous authors reported that infection rate after elbow replacement gained more than other major joints such as hip and knee joints [7,9,13- 15]. They believed since soft tissues of the elbow area were more fragile than of hip, knee or shoulder areas, thus the cover and nourishment were poor. Our cases had gone through at least 1 operation before, a case had even been operated 4 times and soft tissues had been seriously weak. Consequently during our surgeries we aimed to keep soft tissues as much as possible so as to not only increase cover area, decrease infection rate but also disperse pressure on prothesis components to reduce loosening prosthesis rate.
From 1973 to 1985, Morrey and partners carried on 53 elbow replacement surgeries for posttraumatic osteoarthritis; those cases were observed averagely 6.3 years and primary surgery result achieved 64% satisfaction. Mean preoperative elbow range of motion: 41 degrees extension, 111 degrees flexion. Postoperative range of motion was enhanced distinctly: 34 degrees extension, 128 degrees flexion. Pronation-supination was respectively 58 and 64 degrees before and progressed to 68 and 76 degrees after surgery. 11 cases of which had prosthetic loosening complication and were required to reoperate joint replacement. Generally, the results were positive with high satisfaction; however, Morey used the first-generation hinges, which allowed only simple flexion and extension and no varus-valgus motion, therefore prosthetic loosening rate was significant [16]. Our results differed slightly with 2 degrees extension and mean 110 degrees flexion. Aseptic loosening prostheses complication was common and stated by many authors, yet usually happened after long observation time [9,12,13]. Complication rate was reported more in first- generation prostheses since those were highly constrained and no varus-valgus motion, hence more pressure was put on joint components, causing loosening prosthesis [8,12,16]. Our generation had a varus-valgus arc of 5 to 7 degrees, accordingly less pressure was put on joint components during flexion-extension motion, and it decreased loosening prosthesis rate. In our opinion, second-generation or third-generation (able to transfer from linked to unliked joint and vice versa) prosthesis should be ultilized.
In 7 cases, we encountered 1 early complication which is radial nerve injury after megaprosthesis replacement for distal humeral defect: 2 days postoperation the patient presented with incapability of wrist and fingers extension; elbow flexion and extension were not affected. 2 months posoperation, symptoms of radial nerve injury disappeared; the patient was capable of wrist flexion – extension and fingers movement were completely normal. This complication occurred for the reason that the radial nerve was outstretched postoperatively since the soft tissues had been contracted for a long time before. Even so, the injury was absent after 2 months. Radial nerve injury after an elbow replacement is really uncommon, worldwide authors has also rarely encountered this complication. T.Waitzenegger and P.Mansat indicated that most frequent position of radial nerve injury was from medial epicondyle up to the arm about 15.5 cm or 14 cm from olecranon fossa. As well from the report of these 2 authors and their partners, there were 2 causes of radial nerve injury: one was that the leak of the cement through bone resulted in heat or stimulus to radial nerve; the other was stretch or contraction of soft tissues [17].
Conclusion
Total elbow replacement is an effective choice for posttraumatic stiffness, inconsistency or ankylosis of the elbow joint causing its immobility, with the aim to recover structure and function of the elbow joint. However, range of motion evaluation of elbow joint and adjacent joints and thorough preoperative preparation are essential to achieve best outcomes.
Conflict of Interest
No Conflict of Interest
REFERENCES
- Mayo Elbow Performance Score. J Ortho Trauma. 2006;20:S127.
- Prkić A., van Bergen C.J., The B., Eygendaal D.: Total elbow arthroplasty is moving forward: review on past, present and future. World J Orthop. 2016;7:44.
- Mellen R.H, Phalen G.S.: Arthroplasty of the elbow by replacement of the distal portion of the humerus with an acrylic prosthesis. J Bone Joint Surg. 1947;29:348.
- Dee R.: Total replacement arthroplasty of the elbow for rheumatoid arthritis. J Bone Joint Surg Br. 1972;54:88-95.
- D’Ambrosi R., Formiconi F., Ursino N. et al (2019). Treatment of complete ankylosed elbow with total arthroplasty. BMJ Case Reports. 2019;12:e231123.
- Barthel P.Y., Mansat P., Sirveaux F. et al.: Is total elbow arthroplasty indicated in the treatment of traumatic sequelae? 19 cases of Coonrad-Morrey® reviewed at a mean follow-up of 5.2 years. Orthop Traumatol: Surgery & Research. 2014;100:113-118.
- Toulemonde J., Ancelin D., Azoulay V., et al.: Complications and revisions after semi-constrained total elbow arthroplasty: a mono-centre analysis of one hundred cases. Int Orthop. 2016;40:73-80.
- Peden J.P., Morrey B.F.: Total elbow replacement for the management of the ankylosed or fused elbow. J Bone Joint Surg. 2008;90:1198-1204.
- Voloshin I., Schippert D.W., Kakar S. et al.: Complications of total elbow replacement: a systematic review. J Shoulder Elbow Surg. 2011;20:158-168.
- Figgie M.P., Inglis A.E., Mow C.S.: Total elbow arthroplasty for complete ankylosis of the elbow. J Bone Joint Surg. 1989;71:513-520
- Kraay M.J., Figgie M.P., Inglis A.E., et al.: Primary semiconstrained total elbow arthroplasty. Survival analysis of 113 consecutive cases. J Bone Joint Surg. 1994;76:636-640.
- Mansat P., Morrey B.F.: Semiconstrained total elbow arthroplasty for ankylosed and stiff elbows. J Bone Joint Surg. 2000;82:1260.
- Kodde I.F., van Riet R.P., Eygendaal D.: Semiconstrained total elbow arthroplasty for posttraumatic arthritis or deformities of the elbow: a prospective study. J Hand Surg. 2013;38:1377-1382.
- Little C.P., Graham A.J., Karatzas G., et al.; Outcomes of total elbow arthroplasty for rheumatoid arthritis: comparative study of three implants. J Boint Joint Surg. 2005;87:2439-2448.
- Sanchez-Sotelo J., Baghdadi Y.M., Morrey B.F.: Primary linked semiconstrained total elbow arthroplasty for rheumatoid arthritis: a single-institution experience with 461 elbows over three decades. J Bone Joint Surg. 2016;98:1741.
- Morrey B.F., Adams R.A., Bryan R.S.: Total replacement for post-traumatic arthritis of the elbow. J Bone Joint Surg. 1991;73:607-612.
- Waitzenegger T., Mansat P., Guillon P., et al.: Radial nerve palsy in surgical revision of total elbow arthroplasties: A study of 4 cases and anatomical study, possible aetiologies and prevention. Orthop Traumatol: Surgery & Research. 2015;101:903-907.




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.