Submuscular locked plate for fixation of pediatric fracture femur using cluster technique
Received: 13-May-2017 Accepted Date: Jun 16, 2017 ; Published: 19-Jun-2017
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: This study evaluates submuscular locked plate in the pediatric femoral shaft fractures at the age from 6 to 12 years old. Methods: A prospective study was done on 30 patients with fracture shaft femur. 18 of them were males and 12 of them were females. Fixation of all cases was done with a submuscular locked plate using the cluster technique. Results: All fractures healed within 6 weeks. There have been no cases of non-union, malunion or infection. Conclusion: Submuscular locked plate with cluster screw placement is a reliable and a useful option for fixation of pediatric fracture shaft femur.
Keywords
Sub-muscular locked plate, Pediatric fracture femur
Introduction
Several methods are used for fixation of pediatric fracture femur. There is controversy in fixation of pediatric fracture femur in children from 6-12 years old. Elastic rods, intramedullary nail, plating and external fixators are methods for the fixation of pediatric fracture femur [1-4].
According to the current American Academy of Orthopaedic Surgeons (AAOS) Clinical Practice Guidelines concerning pediatric diaphyseal femur fractures, there is poor-quality evidence in support of any specific surgical treatment modality [5].
External fixation can be complicated by refracture, malunion, delayed union, pin tract infections, and unsightly scars [4,6-8]. Rigid intramedullary devices are used routinely in adults, but in children there is a serious risk of damaging the vascular supply to the femoral head, resulting in avascular necrosis of the femoral head when using piriformis fossa or even greater trochanter entry points [1,9,10].
Classical compression plating, with a long incision and more soft tissue damage, has a higher risk of infection and delayed healing, with a reported reoperation rate of 10% [2]. Elastic intramedullary nailing does not prevent shortening or malrotation, and it is difficult to use it for fractures with metaphyseal extensions [3,11-13].
Locked plating provides a biomechanically more stable construct than elastic intramedullary nailing [14].
The purpose of this research is to evaluate the results of submuscular locked plate with cluster technique in the treatment of pediateric femoral shaft fracture.
Patients and Methods
A prospective study was done on 30 patients with fracture shaft femur in our university hospital during 2014 and 2015. Follow up ranges from (6-24 months) average 12 months. 18 were males and 12 were females.
Inclusion criteria were all patterns of pediatric femoral shaft fractures in age range from 6 to 12 years. Exclusion criteria were open femoral shaft fractures and pathological fractures.
Ethical committee agreement was taken. Age, laterality, associated injuries and type of the fracture were documented. All the patients undergo submuscular locked plating by senior surgeon. Intraoperatively time of surgery, bl. loss and radiation exposure were documented Table 1.
| Variables | Values |
| Sex | 18 males 12 females |
| Age | 6-12 |
| Laterality | 16RT 14LT |
| Weight | 23.5 kg (14-41kg) |
| Mechanism of trauma | |
| Fall from height | 16 |
| Motor car accident | 7 |
| Heavy object trauma | 4 |
| Toktok accident | 3 |
| Fracture type according to Muller classification | |
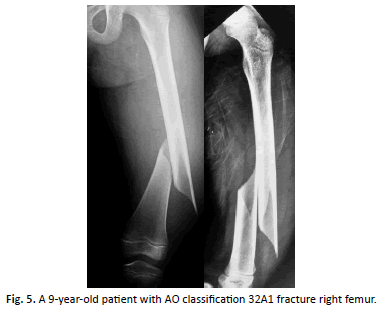
| 32A1 | 6 |
| A2 | 8 |
| A3 | 12 |
| B2 | 4 |
| Fracture level | |
| Prox | 8 |
| Middle | 16 |
| distal | 6 |
| Length unstable | 10 |
| Days from injury* | 2.5(0-8) |
| Operative time* | 57min(30-100min) |
| Fluoroscopic time* | 51 sec |
| Estimated blood loss* | 80cc(50-150cc) |
Table 1: Patient demographic, fracture and operative data.
A special technique for locked plate insertion was followed. Radiolucent operative table was used. If there was substantial comminution, both lower extremities were prepared and draped, allowing for intraoperative comparisons between the two extremities for rotation and length. The plate length was chosen intraoperatively using fluoroscopy.
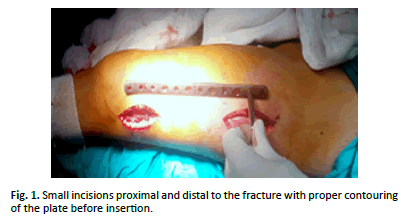
The plate was contoured proximally and or distally if needed. A small proximal incision was opened. Skin, facia lata and vastus posterolaterally was opened. The plate was slided exteraperiostially under the vastus lateralis muscle (Figure. 1).
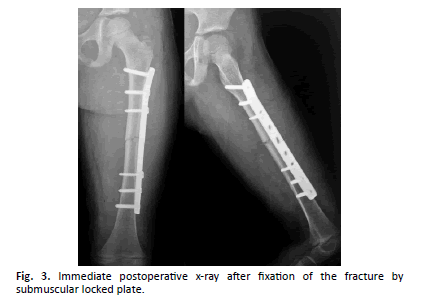
The most prox. screw was fixed. Then the 3rd screw from above. The screws were taken unlocked first to bring the plate on the bone. The distal incision was opened, then closed reduction was done, then the 3rd screw from below was taken unlocked to bring bone to the plate, so that indirect reduction of the fracture could be gained, then the most distal screw was taken locked. Sometimes, especially in simple fractures, sub-muscular digital reduction from distal or proximal incision was needed. Another 2 screws (the 2nd from above and below) should be taken. Thus, 3 screws above and 3 screws below the fracture were taken. All fractures were fixed with the same technique. Narrow locked plate was used with length from 8-14 holes. AP and Lat views were done to confirm reduction. Closed bridge plating technique has the disadvantage of not allowing for intraoperative open assessment of limb alignment. Several intraoperative clinical and radiographic examination methods that had been found to be reliable were developed to solve this problem. Some of these methods such as the cable technique, clinical knee hyperextension test, hip rotation test, and lesser trochanter shape sign were performed to ensure the proper limb alignment in the current study. Closure of the wound was done in anatomical matter.
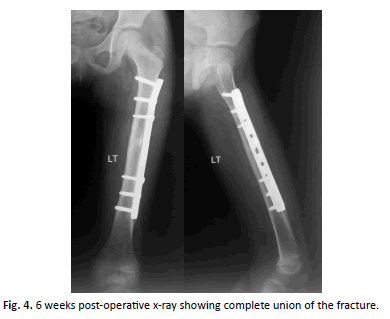
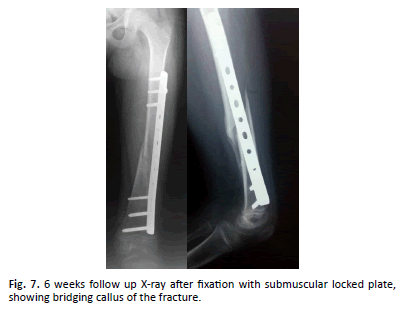
No post-operative immobilization was needed. The Patient came after 2 weeks for stitch removal. The patient came after 6 weeks to take X-ray to see if bone is healed to begin weight bearing. The patient came after 3 months for assessment of gait, alignment, rotation and knee motion.
Fracture type was classified according to the OTA/AO classification as follows: A (simple, transverse or short oblique), B (wedge-shaped middle fragment), or C (complex, with multiple fragments) [15].
There were 26 (86.6%) Type A fractures and 4 (13.3%)) Type B. Fracture instability was defined as length unstable if it was complex or spiral (the length of the fracture was twice as long as the diameter of the femur at the level of the fracture) [16,17]. (33.3%) of fractures were length-unstable fractures. Fracture level was separated into the proximal, middle, and distal 1/3 of the diaphysis. Proximal 1/3 diaphyseal fractures occurred in 8(26.6%) patients, middle 1/3 fractures in 16(53.3%), and distal 1/3 fractures in 6 (20%).
Results
30 cases of pediatric fracture femur were fixed with submuscular locked plate including 18 males and 12 females. Age was from 6 to 12 years. There were 16 right, 14 left. The average weight of the patients was 23.5kg. Mechanisms of injury included: fall from height (16), motor car accident (7), heavy object trauma (4) and motorbike accident (3).
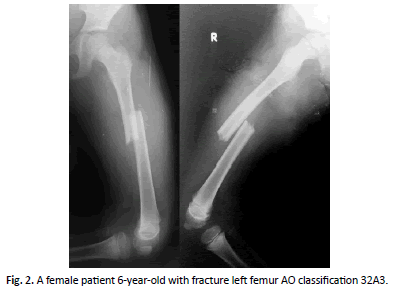
All fractures achieved union (bridging callus in AP and LAT.) in average 6 weeks (Figure. 2-7).
Mean duration of surgery was 57 min., mean blood loss was 80 cc. and mean number of Fluoroscopic time was 51sec. None of our patients had clinically important malrotation or shortening noticed by parents or treating surgeons. None of the patients with an LLD required a shoe lift or had any functional deficit at latest follow-up. Weight and age of the child don’t affect healing time, alignment and length Also, there were no differences in the above parameters among different fracture locations (proximal/middle/distal), and no major complications occurred in proximal or distal fractures. There were no cases of infection. Implant removal was done for 20 cases after 8-12 months of fixation from the same incisions without complications. It is our strategy to remove the plate after 8-12 months but some patients are delayed because of socioeconomic aspects.
Discussion
Pediatric femoral shaft fracture is a common injury. Casting, external fixation, elastic intramedullary nail, intramedullary nails, compression plating and submuscular plate have all been used as a treatment option. The current AAOS Clinical Practice Guidelines suggest there is poor-quality evidence in support of any specific surgical treatment modality for diaphyseal femur fractures in children [5].
In a prospective, randomized trial comparing spica casting to external fixation, Wright et al. reported a 45% malunion rate in children treated with spica casts, although there was not a statistically significant difference in functional outcome or parent/ child satisfaction [18].
Skeletally immature patients are at increased risk for osteonecrosis of the femoral head when piriformis or near piriformis fossa entry nails are used. The rate of this potentially devastating complication is at least 4%. Every effort should be made to decrease the risk of osteonecrosis [1]. There is a risk for growth arrest of the greater trochanter apophysis resulting in coxa valga and heterotopic bone formation when violating the trochanteric physis [9]. External fixation is complicated by high refracture rate, pin tract problems, and unsightly scars [4]. Traditional compression plating has hardware failures and a non-union rate as much as 10% [2,19].
Elastic intramedullary nailing does not prevent shortening or malrotation, and it is difficult to use it for fractures with metaphyseal extension [3,11-13].
In the current study, Proximal 1/3 diaphyseal fractures occurred in 8(26.6%) patients, and distal 1/3 fractures in 6 (20%). All were fixed well with submuscular locked plate with good stability and all healed without malalignment or LLD.
Caglar et al. compared 21 patients treated with minimally invasive plating with 17 patients treated by titanium elastic nail system (TENS) in the age group 6-12 years and did not find any difference in healing time but found fewer complications with plate [20].
Sink et al. compared femur fracture types and analyzed complications of titanium elastic nails. After the efficacy of elastic nails had been identified by other authors, this study group treated nearly all midshaft femur fractures with TENs. They reviewed 39 consecutive children with midshaft femur fractures, identifying a 62% complication rate and eight patients (21%) who underwent unplanned surgeries prior to complete union. Though not statistically significant, the overall complication rate for lengthunstable fractures compared with length-stable fractures was 80 as opposed to 50%. Length-unstable fractures were defined as comminuted or long oblique fractures; for the latter, the length of the obliquity was twice as long as the femoral diameter at the fracture level. Major complications, requiring operative revision, were significantly higher in the length-unstable group (66 compared with 12.5%). A decreased incidence of complications was reported when at least 80% of the canal diameter was filled by the combined diameter of the nails [21].
In the current study (33.3%) of fractures were length-unstable fractures all healed after 6 weeks without malalignment or LLD.
In addition to length-unstable fracture patterns, older age and increased body weight have been associated with an increased incidence of complications after stabilization with TENs. Flynn led another multi-centre TEN study from six centers, with 234 femur fractures in 229 patients. Ninety percent of patients had excellent or satisfactory results, with excellent or essentially perfect results in 64%. There were 23 cases classified as poor for a 10% significant complication rate – many of these were classified as poor based on radiographic malalignment that was not always clinically relevant. The outcome was better for central third fractures, and a significantly higher complication rate was noted in older (>11 years) and heavier (>108 lbs) patients [22]. One level IV study demonstrated a five times higher risk of poor outcomes for flexible nailing in patients weighing ≥ 49 kg (≥ 108 lb) [23].
A number of studies report SBPs are associated with high rates of healing, reasonable alignment, and low reoperations rates, their findings require confirmation and proof of reproducibility [24-27].
In 2006, Sink et al. described their technique for sub-muscular bridge plating. This study included 27 patients over a 2-year span at 2 level-I pediatric trauma centers. A single distal incision followed by several small incisions allowed for percutaneous placement of screws. There were no intraoperative complications and all patients healed by 12 weeks. The plates were removed electively around 6 to 8 months through the same percutaneous incisions without difficulty. There were no cases of refracture after plate remova [27].
Our technique involves 2 incisions on the lateral aspect of the thigh. The length of the incisions allows screw placement to be made under direct visualization. In this study, percutaneous screw placement wasn’t needed.
Pre-contouring the plate to the patient’s femur allows for reduction of the varus or valgus angulation. Recommendation of plate removal typically occurs after 6 months. We have found implant removal to be simplified because, under direct visualization, the screws are removed through the same proximal and distal incisions. This also reduces radiation exposure and decreases fluoroscopy time. No complication or difficulty encountered in plate removal.
None of our patients had clinically important malrotation or shortening noticed by parents or treating surgeons. None of the patients with an LLD required a shoe lift or had any functional deficit at latest follow-up.
A lot of studies support the use of sub-muscular locked plate in length-unstable fractures, proximal and distal pediatric femoral fractures and in heavy children (>40 kg) and older children [26-29].
In the current study sub-muscular locked plate used in all fracture patterns in the age from 6-12 years old with excellent results.
The technique of femoral shaft plating has evolved with a better understanding plate mechanics. Rozbruch et al evaluated results of femoral fracture plating over 30 years, emphasizing the evolution of plating techniques, including the use of longer plates, indirect reduction techniques, fewer plate screws, and fewer lag screws. The best predictor of success was the length of the plate. In the comminuted and long oblique fractures treated in this study, the longer plate results in less strain on the plate and screws as the working length of the plate increases. With the soft tissues intact around the fracture, the more rapid callus formation results in earlier load sharing of the bone. This limits the period of the load carried by the plate and the potential for failure. The longer plate also requires fewer screws needed for optimal plate fixation. It was found that if the fracture was of significant length, allowing room for 2 to 3 screws proximal and distal, there was still enough mechanical stability with a long plate to successfully stabilize the fracture [30].
It combines the best characteristics of closed treatment methods (preservation of the biology of the fracture site) with the best characteristics of surgical treatment (stability and preservation of the correct alignment, early mobility and ease of care).
Cluster technique simplifies application of the screws through the small incisions. From this study cluster technique gives good stability for healing of pediatric fracture shaft femur.
Our study has several limitations as small sample size, short follow up and absence of comparison group. Subsequent studies analyzing long-term follow-up are needed to support these findings.
Conclusion
Submuscular locked plate with cluster technique is a good fixation tool for pediatric fracture shaft femur and can be used in all fracture patterns with the least complications.
Compliance with Ethical Standards
Conflict of interest
All of the authors declare that they have no conflict of interest.
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all guardians or parents of children included in the study.
REFERENCES
- Buford D., Christensen K., Weatherall P.: Intramedullary nailing of femoral fractures in adolescents. Clin OrthopRelat Res. 1998; 350: 85-89.
- Caird M.S., Mueller K.A., Puryear A., et al.: Compression plating of pediatric femoral shaft fractures. J Pediatr Orthop. 2003; 23: 448-452.
- Flynn J.M., Luedtke L., Ganley T.J., et al.: Titanium elastic nails for pediatric femur fractures: Lessons from the learning curve. Am J Orthop. 2002; 31: 71-74.
- Miner T., Carroll K.L.: Outcomes of external fixation of pediatric femoral shaft fractures. J Pediatr Orthop. 2000; 20: 405-410.
- Kocher M.S., Sink E.L., Blasier R.D., et al.: Treatment of pediatric diaphyseal femur fractures. J Am Acad Orth. 2009; 17: 718-725.
- Anglen J.O., Choi L.: Pediatric femoral shaft fractures. J Orthop Trauma. 2005; 19: 724-733.
- Poolman R.W., Kocher M.S., Bhandari M.: Pediatric femoral fractures: a systematic review of 2422 cases. J Orthop Trauma. 2006; 20: 648-654.
- Skaggs D.L., Leet A.I., Money M.D.: Secondary fractures associated with external fixation in pediatric femur fractures. J Pediatr Orthop. 1999; 19: 582-586.
- Hosalkar H.S., Pandya N.K., Cho R.H., et al. Intramedullary nailing of pediatric femoral shaft. J Am Acad Orthop Surg. 2011; 19: 472-481.
- MacNeil J.A., Francis A., El-Hawary R.: A systematic review of rigid, locked, intramedullary nail insertion sites and avascular necrosis of the femoral head in the skeletally immature. J Pediatr Orthop. 2011; 31: 377-380.
- Flynn J.M., Hresko T., Reynolds R.A., et al.: Titanium elastic nails for pediatric femur fractures: A multicenter study of early results with analysis of complications. J Pediatr Orthop. 2001; 21: 4-8.
- Heinrich S.D., Drvaric D.M., Darr K., et al.: The operative stabilization of pediatric diaphyseal femur fractures with flexible intramedullary nails: A prospective analysis. J Pediatr Orthop. 1994; 14: 501-507.
- Luhmann S.J., Schootman M., Schoenecker P.L., et al.: Complications of titanium elastic nails for pediatric femoral shaft fractures. J Pediatr Orthop. 2003; 23: 443-447.
- Porter S.E., Booker G.R., Parsell D.E., et al.: Biomechanicalanalysis comparing titanium elastic nails with locked plating in two simulated pediatric femur fracture models. J Pediatr Orthop. 2012; 32: 587-593.
- Müller M.E., Nazarian S., Koch P., et al.: The Comprehensive Classification of Fractures of Long Bones Springer-Verlag: New York; 1990.
- Garner M.R., Bhat S.B., Khujanazarov I., et al. Fixation of length-stable femoral shaft fractures in heavier children: flexible nails vs rigid locked nails. J Pediatr Orthop. 2011; 31: 11-16.
- Winquist R.A., Hansen S.T., Clawson D.K.: Closed intramedullary nailing of femoral fractures: a report of five hundred and twenty cases. J Bone Joint Surg Am. 1984; 66: 529-539.
- Wright J., Wang E., Owen J., et al.: Treatments for paediatric femoral fractures: a randomized trial. Lancet. 2005; 365: 1153-1158.
- Fyodorov I., Sturm P.F., Robertson W.W.: Compression-plate fixation of femoral shaft fractures in children aged 8 to 12 years. J Pediatr Orthop. 1999; 19: 578-581.
- Caglar O., Aksoy M.C., Yazici M.: Comparison of compression plate and flexible intramedullary nail fixation in pediatric femoral shaft fractures. J Pediatr Orthop B. 2006; 15: 210-214.
- Sink E., Gralla J., Repine M.: Complications of pediatric femur fractures treated with titanium elastic nails. J Pediatr Orthop. 2005; 25: 577-580.
- Flynn J., Moroz L., Launay F.: An international, multicenter analysis of complications of elastic stable intramedullary nailing of pediatric femur fractures. In POSNA Annual Meeting; 2004; St Louis, MO. p. 27.
- Moroz L.A., Launay F., Kocher M.S., et al.: Titanium elastic nailing of fractures of the femur in children: Predictors of complications and poor outcome. J Bone Joint Surg Br. 2006; 88: 1361-1366.
- Hedequist D BJHT. Locking plate fixation for pediatric femur fractures. J Pediatr Orthop. 2008; 28: 6-9.
- Hedequist D.J., Sink E.: Technical aspects of bridge plating for pediatric femur fractures. J Orthop Trauma. 2005; 19: 276-279.
- Kanlic E.M., Anglen J.O., Smith D.G., et al.: Advantages of submuscular bridge plating for complex pediatric femur fractures. Clin Orthop Relat Res. 2004; 426: 244-251.
- Sink E.L., Hedequist D., Morgan S.J., et al. Results and technique of unstable pediatric femoral fractures treated with submuscular bridge plating. J Pediatr Orthop. 2006; 26: 177-181.
- Samora W.P., Guerriero M., Willis L., et al.: Submuscular Bridge Plating for Length-Unstable, Pediatric Femur Fractures. J Pediatr Orthop. 2013; 33: 797-802.
- Abdelgawad AA., Sieg R.N., Laughlin M.D., et al.: Submuscular Bridge Plating for Complex Pediatric Femur. Clin Orthop Relat Res. 2013; 471: 2797-2807.
- Rozbruch S.R., Muller U., Gautier E., et al.: The evolution of femoral shaft plating technique. Clin Orthop. 1998; 354: 195-208.




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.