Shoulder hemiarthroplasty for complex proximal humerus fracture: Vietnamese experiences
2 Saint Paul Hospital, Vietnam, Email: MANHNGUYENHUU2@aol.com
Received: 06-Feb-2020 Accepted Date: Apr 29, 2020 ; Published: 17-May-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Proximal humerus fracture accounts for 4%-5% of fractures, most of them in older people. For cases of 3-part of 4-part fractures, fracture-dislocation, or comminuted fracture, internal fixation is very difficult to achieve good results. These cases are usually indicated for shoulder joint replacement surgery. The purpose of the study evaluated the results of shoulder hemiarthroplasty surgery in patients with complex proximal humerus
fracture.
Material and Methods: This prospective study included 30 patients with complex proximal humerus fractures who were treated by shoulder hemiarthroplasty during the period from January 2015 to December 2018. The average follow-up time was 26 months. The results of the surgery were evaluated based on the postoperative range of motion, shoulder Constant score, and the postoperative radiograph.
Results: The average postoperative Constant score was 67.65. The active elevation, abduction, internal rotation and external rotation at the last follow-up were 110.2°, 98.6°, 34.5°, and 22.7°, respectively. There were 20 patients (66.67%) without pain, 8 patients (26.67%) with mild pain, and 2 patients (6.66%) with moderate pain. There were 4 patients of nonunion of the greater and lesser tuberosity. There were no complications of dislocation, infection,
and stem loosening.
Conclusion: shoulder hemiarthroplasty in patients with complex proximal humerus fracture was a safe surgery and had very good results on shoulder function, patients returned to daily activities early.
Keywords
Shoulder hemiarthroplasty, complex proximal humerus fractures, shouder replacement
Introduction
Proximal humeral fracture accounts for 4%-5% of total fractures. There are two common forms of proximal humeral fracture in clinical features: usually in older women because of injury with low energy and in young men is often with high energy injury [1-3]. Although the majority of non-displaced fractures can be treated conservatively, treatment of displaced or complex fractures is a controversial issue [4,5]. Many current types of research show that it is not possible to make an accurate conclusion among joint replacement surgery, intramedullary nail, locking compression plate, or conservative treatment in humeral fracture treatment [6,7]. With a lot of advances of technique and instruments such as locking plate, surgical treatment of proximal humeral fracture has become increasingly popular, but there are still a few reports about the high rate of complication over the open reduction and internal fixation and close reduction and internal fixation [8-13]. These complications are related to the risk of vascular injury nourishing the proximal humeral fracture [6,7]. This has caused rotator cuff injury, the high percentage of osteoporosis in the fracture area, especially the rate of necrosis the humeral head [5]. This rate is little changed even with the most modern treatment techniques and it is clear that the rate of necrosis the humeral head is increasing by the time [3,5]. Due to these complications, it is recommended to shoulder hemiarthroplasty or reverse shoulder replacement which is often applied if humeral fracture with dislocation and complex humeral head fracture [3]. The purpose of this study is to evaluate the effectiveness of hemiarthroplasty surgery in complex proximal humeral fractures.
Materials and Methods
We conduct a prospective study from January 2015 to December 2017.
Criteria SelectionPatients with proximal humeral fractures following Neer classification including complex proximal humeral fracture (3-part or 4-part) or proximal humeral fracture with shoulder dislocation based on shoulder X-rays and shoulder CT-scanner [14].
There is no accompanying with the brachial plexus injury.
All the patients who meet the above selection criteria will be performed shoulder hemiarthroplasty.
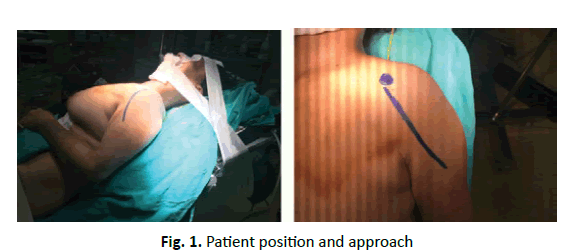
TechniquesSurgeries were performed with the patients under general anesthesia in a semi-seated position on the shoulder table.
A deltopectoral approach utilized to all the patients (Fig. 1).
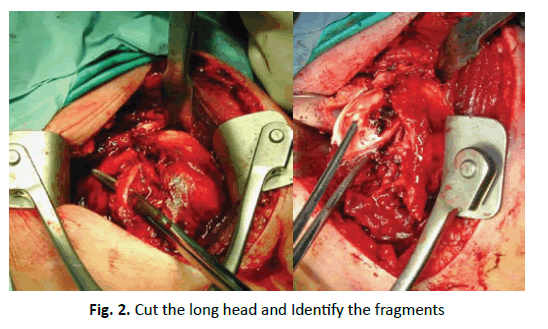
Cut the long head of biceps tendon at the footprint to glenoid, this tendon was tenodesed to at the bicipital groove.
Identify the fragments of greater and lesser tuberosities. In cases of the footprint of pectoralis major was intact, we keep it. This can be used to identify the height of the stem (Fig. 2).
Based on the diameter of the humeral head to determine the diameter of the humeral head component.
Ream the humeral shaft and choose the diameter of actual stems, 1 size smaller than the diameter of the last reaming.
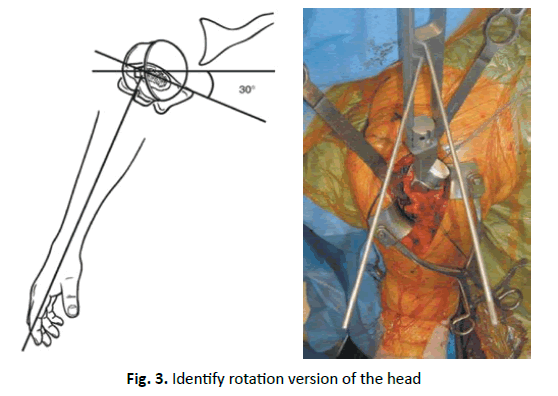
Based on the X-rays and CT scanner on the normal shoulder to determine the height and rotation version of head of artificial shoulder joint usually in the range of 20-30 degrees (Fig. 3).
Using 5 fiber wires sutures including 2 sutures to recover greater tuberculosis, 2 sutures to recover lesser tuberculosis, and 1 suture for the rotator cuff interval and attached the biceps tendon. After tying fiber wires sutures if fragments not stable, we use reinforced steel sutures.
All the patients were dressed in Dassault’s bandage for 4 weeks to immobile the shoulder joint, start passive range of motion soon after surgery, active exercise after 06 weeks, and strengthen exercise after 03 months.
The patients were evaluated after surgery based on Pain score, Constant score, range of motion after surgery, bone healing, dislocation or subluxation, stem loosening based on X-rays at different time points immediately after surgery, 1 month, 3 months, 6 months, 12 months and the last time before the end of the study.
Results
Some Characteristics of Patients
The average age of patients (at the time of surgery) was 66.7 years (range 51-84). Most were women with 26 patients accounts for 86.67%. The main mechanism of injury was fall, with 20 patients (66.67%).
Characteristics of Morphological Proximal Humeral Fracture
Most were Neer type IV including 23 patients with simple fracture occupies 76.67%, 4 patients fracture with dislocation occupies 13.33%), 3 patients with Neer type III occupies 10%.
Average Follow-Up Time after Surgery was 26 Months
The average post-op Constant score was 67,65. Most of the patients returned to normal activities.
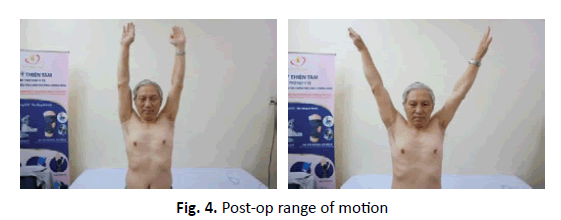
Post-Op Range of Motion
Active forward flexion was 110.2° (range 75°-170°), abduction was 98.6° (range 60°-135°), internal rotation was 34.5° (range 10°-60°), and external rotation was 22.7° (range 15°-45°) (Fig. 4).
There were 20 patients (66.67%) of painless, 8 patients (26.67) of mild pain, and 2 patients (6.66%) of moderate pain.
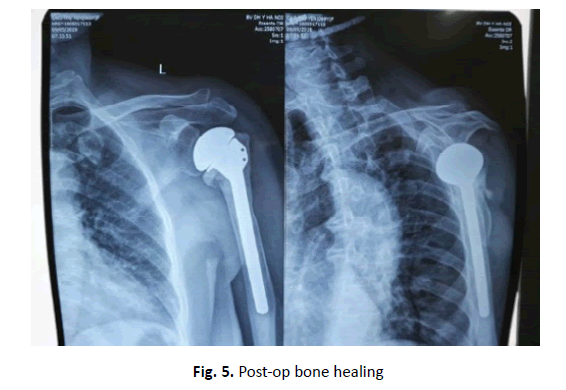
All 30 cases showed good bone healing at greater and lesser tuberosities (Fig. 5).
There was no complication of stem loosening, dislocation, and infection.
Discussion
Managements of complex proximal humerus fractures and indications of shoulder hemiarthroplasty.
Management of proximal humerus fractures includes a wide range of treatment options such as conservative treatment, Open Reduction and Internal Fixation (ORIF), and shoulder replacement. Appropriate treatment to obtain good results depend on many factures such as fracture pattern, patient’s condition, and qualification of the treatment facility.
The results of ORIF and conservative treatment for complex proximal humerus fracture are still debated [15-18]. Krappinger et al. showed that in cases of comminuted fractures in elderly patients with osteoporosis, ORIF often fails [19]. With the epidemiological characteristics of the elderly in Vietnam, the rate of osteoporosis in this group is very high.
Shoulder hemiarthroplasty is a surgery that requires rigorous techniques that usually indicated for the elderly who have complex proximal humerus fractures with the intact function of the rotator cuff. It can reduce pain, restore shoulder biomechanical function, and range of motion [20-22]. In this study, we had patients with an average age of 67.65, most of whom had a 4-part fracture, the rest were patients with fracture-dislocation or 3-part fracture in old patients with osteoporosis. These findings are similar to G. Kontakis’ systematic review, which showed that most cases of proximal humerus fracture in the elderly were 4-part fractures or fracture-dislocation [23]. These are groups of patients who are at high risk of complication of necrosis of the humeral head or nonunion after ORIF surgery, so we proactively assign a hemiarthroplasty to avoid these complications. In some review articles, it is shown that older patients with less need for shoulder function, poor bone quality, or cases of comminuted fracture, the hemiarthroplasty surgery has many advantages [5,23,24]. Krishnan et al. found that the patients’ age was one of the most important factors for choosing the treatment method for proximal humerus fracture, in which older patients were appointed to shoulder replacement [25].
Surgical Techniques and Results of Shoulder Hemiarthroplasty
Neer was the first to describe the results of hemiarthroplasty for patients with proximal humerus fractures with good and excellent outcomes accounting for 98% [26]. This method provides the early stability of the shoulder joint and pain relief after surgery [23]. In a controlled clinical trial comparing shoulder hemiarthroplasty and conservative treatment of proximal humerus fractures also showed improvement in function, quality of life, pain relief, or shoulder hemiarthroplasty surgery compared with conservative treatment [27].
During the surgery, we have always tried to recover the fragments of greater and lesser tuberosities into the anatomical position and firmly fixed to the stem. The fracture fragments were always guaranteed to be in contact with each other. In the cases of displacement due to comminuted fragments, after the recovery stage, we harvested cancellous bone from the humeral head and carried out bone grafting, which will facilitate the healing of the greater and lesser tuberosities. Chambers et al. also found that the results of partial shoulder replacement surgery would achieve the best results if the tuberosities were healed [3]. Liu and his colleagues retrospectively studied 33 patients with shoulder hemiarthroplasty that found nonunion of greater and lesser tuberosities in 18 patients, these patients had a significant difference in pain and shoulder function [28].
Determining stem version and height also are primary aspects to prevent failures [3]. During the surgery, we found that it is very difficult to determine the height of the stem, so it must be based on some anatomical landmarks such as the attachment point of the pectoralis major (if intact) or the height of the opposite humerus. With the patients with fracture-dislocation, we let the retroversion be higher than normal to prevent dislocation. A stem positioning guide was developed to ensure the correct height and version of the implant. Incorrect version of the stem reduces the healing ability of the tuberosities and increases the risk of implant instability [29,30]. Intra-operative fluoroscopic criteria, intra-medullary position guide, extra-medullary jig fixed to the elbow, and anatomic landmarks have been proposed [31-34]. Boileau reported that lengthening of the humerus increases the risk of tuberosity detachment, malunion or nonunion, which will lead to a decrease or loss of rotator cuff function; shortening will result in loss of deltoid tension, compromising its function [35].
Greiner showed a correlation between tuberosities displacement and further fatty infiltration of rotator cuff muscles after shoulder hemiarthroplasty for proximal humerus fracture [36]. Since the original technique was described, some methods of tuberosities fixation and stem designs were developed to ensure a good functional result [37- 39]. The most popular complication that affects the results is the failure of fixation and nonunion, which will lead to pain, loss of function, and noncompliance with rehabilitation.
Conclusion
Through the evaluation of the results of shoulder hemiarthroplasty surgery in 30 patients with proximal humerus fractures, we found this method to be a valid and reliable technique for the treatment of complex proximal humerus fractures. After surgery patients have very good shoulder function, few complications and patients returned to daily activities early. The fixation technique of the tuberosities and the height and version of the stem are important factors determining the outcomes of this method.
REFERENCES
- Court-Brown C.M., Garg A., Mc-Queen M.M.: The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72:365-371.
- Green A., Norris T., Browner B., et al.: Proximal humerus fractures and fracture dislocations. Skeletal Trauma. 2003;3:1532-1624.
- Chambers L., Dines J.S., Lorich D.G., et al.: Hemiarthroplasty for proximal humerus fractures. Curr Rev Musculoskelet Med. 2013;6:57-62.
- Koval K.J., Gallagher M.A., Marsicano J.G., et al.: Functional outcome after minimally displaced fractures of the proximal part of the humerus. J Bone Joint Surg Am. 1997;79:203-207.
- Jordan R.W., Modi C.S.: A Review of Management Options for Proximal Humeral Fractures. Open Orthop J. 2014;8:148-156.
- Lanting B., MacDermid J., Drosdowech D., et al.: Proximal humeral fractures: a systematic review of treatment modalities. J Shoulder Elbow Surg. 2008;17:42-54.
- Solberg B.D., Moon C.N., Franco D.P., et al.: Surgical treatment of three and four part proximal humeral fractures. J Bone Joint Surg Am. 2009;91:1689-1697.
- Zhang A.L., Schairer W.W., Feeley B.T.: Hospital Readmissions After Surgical Treatment of Proximal Humerus Fractures: Is Arthroplasty Safer Than Open Reduction Internal Fixation? Clin Orthop Relat Res. 2014;472:2317-2324.
- Gregory T.M., Vandenbussche E., Augereau B.: Surgical treatment of three and four-part proximal humeral fractures. Orthop Traumatol Surg Res. 2013;99:197-207.
- Helmy N., Hintermann B.: New trends in the treatment of proximal humerus fractures. Clin Orthop Relat Res. 2006;442: 100-108.
- Hirschmann M.T., Quarz V., Audige ´ L., et al.: Internal fixation of unstable proximal humerus fractures with an anatomically preshaped interlocking plate: a clinical and radiologic evaluation. J Trauma. 2007;63:1314-1323.
- Kou Koukakis A., Apostolou C.D., Taneja T., et al.: Fixation of proximal humerus fractures using the PHILOS plate: early experience. Clin Orthop Relat Res. 2006;442:115-120.
- Moonot P., Ashwood N., Hamlet M.: Early results for treatment of three and four-part fractures of the proximal humerus using the PHILOS plate system. J Bone Joint Surg Br. 2007;89:1206-1209.
- Neer II C.S.: Displaced proximal humeral fractures: I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077-1089.
- Schliemann B., Siemoneit J., Theisen C., et al.: Complex fractures of the proximal humerus in the elderly-outcome and complications after locking plate fixation. Musculoskelet Surg. 2012;96:S3-S11.
- Helwig P., Bahrs C., Epple B., et al.: Does fixed-angle plate osteosynthesis solve the problems of a fractured proximal humerus? A prospective series of 87 patients. Acta Orthopaedica. 2009;80:92-96.
- Misra A., Kapur R., Maffulli N.: Complex proximal humeral fractures in adults-a systematic review of manage-ment. Injury. 2001;32:363-372.
- Bell J.E., Leung B.C., Spratt K.F., et al.: Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2001;93:121-131.
- Krappinger D., Bizzotto N., Riedmann S., et al.: Predicting failure afer surgical fxation of proximal humerus fractures. Injury. 2011;42:1283-1288.
- Shukla D.R., McAnany S., Kim J., et al.: Hemiarthroplasty versus reverse shoulder arthroplasty for treat- ment of proximal humerus fractures: a meta-analysis. J Shoulder Elbow Surg. 2016;25:330-340.
- Gallinet D., Clappaz P., Garbuio P., et al.: Three or four parts complex proximal humerus fractures: hemi- arthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res. 2009;95:48-55.
- Boyle M.J., Youn S.M., Frampton C.M., et al.: Functional outcomes of reverse shoulder arthroplasty compared with hemi- arthroplasty for acute proximal humeral fractures. J Shoulder Elbow Surg. 2013;22:32-37.
- Kontakis G., Koutras C., Tosounidis T., et al.: Early management of proximal humeral fractures with hemiarthroplasty: a systematic review. J Bone Joint Surg Br. 2008;90:1407-1413.
- Hertel R., Hempfing A., Stiehler M., et al.: Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13:427-433.
- Krishnan S.G., Bennion P.W., Reineck J.R., et al. Hemiarthroplasty for proximal humeral fracture: restoration of the Gothic arch. Orthop Clin North Am. 2008;39:441-450.
- Neer C.S. II.: Displaced proximal humeral fractures. Part II. Treatment of three part and four-part displacement. J Bone Joint Surg Am. 1970;52:1090-1103.
- Olerud P., Ahrengart L., Ponzer S., et al.: Hemiarthroplasty versus nonoperative treatment of displaced 4 part proximal humeral fractures in elderly patients: a randomised controlled trial. J Shoulder Elbow Surg. 2011;20:1025-1033.
- Liu J., Li S.H., Cai Z.D., et al.: Outcomes, and factors affecting outcomes, following shoulderhemiarthroplasty for proximal humeral fracture repair. J Orthop Sci. 2011;16:565-572.
- Cadet E.R., Ahmad C.S.: Hemiarthroplasty for three- and four-part proximal humerus fractures. J Am Acad Orthop Surg. 2012;20:17-27.
- Hempfing A., Leunig M., Ballmer F.T., et al.: Surgical landmarks to determine humeral head retrotorsion for hemi- arthroplasty in fractures. J Shoulder Elbow Surg. 2001;10:460-463.
- Dines D.M., Warren R.F., Craig E.: intramedullary fracture positioning sleeve for proper placement of hemiarthroplasty in fractures of the proximal humerus. Technique Shoulder Elbow Surg. 2007;8:69-74.
- Krishnan S.G., Reineck J.R., Bennion P.D., et al.: Shoulder arthroplasty for fracture: does a fracture-specific stem make a difference? Clin Orthop Relat Res. 2011;469:3317-3323.
- Boileau P., Pennington S.D., Alami G.: Proximal humeral fractures in younger patients: fixation techniques and arthroplasty. J Shoulder Elbow Surg. 2011;20:47-60.
- Murachovsky J., Ikemoto R.Y., Nascimento L.G., et al.: Pectoralis major tendon reference (PMT): a new method for accurate restoration of humeral length with hemiarthroplasty for fracture. J Shoulder Elbow Surg. 2006:15:675-678.
- Boileau P., Krishnan S.G., Tinsi L., et al.: Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2002;11:401-412.
- Greiner S.H., Diederichs G., Kroning I., et al.: Tuberosity position correlates with fatty infiltration of the rotator cuff after hemiarthroplasty for proximal humerus fractures. J Shoulder Elbow Surg. 2009;18:431-436.
- Neer C.S.: Results of nonconstraint shoulder arthroplasty. In: Neer CS (ed) Shoulder reconstruction., W. B. Saunders Company. 1990;262-271.
- Baumgartner D., Nolan B.M., Mathys R., et al.: Review of fixation techniques for the four-part fractured proximal humerus in hemiarthroplasty. J Orthop Surg Res. 2011;6:36.
- Obert L., Saadnia R., Loisel F., et al.: Cementless anatomical prosthesis for the treatment of 3-part and 4-part proximal humerus fractures: cadaver study and prospective clinical study with minimum 2 years followup. SICOT J. 2016;2:22.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.