Functional outcome in intradural extramedullary tumor patients after surgical tumour excision: Case series
2 Assistant Professor, Department of Orthopaedics, Rajshree Medical and Research Institute, Bareilly, India
3 Professor, Department of Orthopaedics, Rajshree Medical and Research Institute, Bareilly, India, Email: drvishnulalnair@gmail.com
Received: 18-Feb-2023, Manuscript No. jotsrr-22- 92818; Editor assigned: 20-Feb-2023, Pre QC No. jotsrr-22- 92818 (PQ); Accepted Date: Feb 28, 2023 ; Reviewed: 21-Feb-2023 QC No. jotsrr-22- 92818 (Q); Revised: 23-Feb-2023, Manuscript No. jotsrr-22- 92818 (R); Published: 03-Mar-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: About two-thirds of the benign intraspinal neoplasms are intradural extramedullary spinal cord tumours (IESCT). On rare occasions, they exhibit neurological involvement ranging from acute to chronic, necessitating urgent surgical intervention.
Methods: Here, we examined a group of 10 intradural extramedullary tumours treated between 2020 and 2022 by a single orthopaedic surgeon at Rajshree Medical and Research Institute, Bareilly's department of orthopaedics. Patients were followed up forat least two years. Clinical and functional outcome of these patients were evaluated by Karnofsky Performance Score [KPS], and Modified McCormick scale
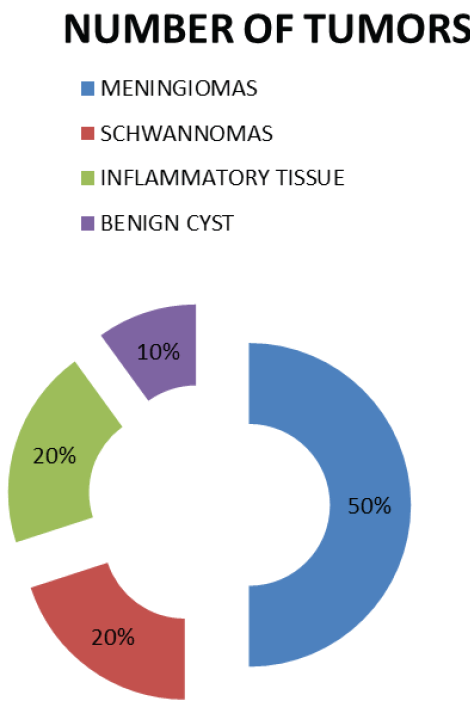
Results: Thoracic spine 07 (70%) and junctional tumours 3 (30%) were the major sites of the majority of IESCT tumour in our study. There were 5 meningiomas, 2 schwannomas, 2 inflammatory, and 1 benign cyst on histo-pathological analysis. Meningiomas were typically found dorsal spine and dorso-lumbar junction, while schwannomas were found in the middle of the dorsal region. Both KPS and the Modified McCormick scale were significantly improved after surgery.
Conclusion: MRI scan with constrast can easily identify the majority of benign intradural extramedullary tumours. It was observed that earlier diagnosis of neurological involvement were associated with good prognosis. Notably, surgical intervention is followed by positive functional outcomes.
Keywords
Clinical outcome, Intradural extramedullary tumors, Spinal tumors, Surgical excision, COVID Pandemic, Neurological evaluation
Introduction
Primary spinal cord tumours are classified as extradural, Intradural Extramedullary (IDEM: 65%), and intramedullary, making for 2%-4% of all central nervous system neoplasms. Meningiomas, schwannomas, and neurofibromas are the most frequent IDEM tumours [1]. Although these tumours are typically benign and slow-growing, sometimes they can have neurological involvement and might progress to paraparesis/ paraplegia.Intraspinal malignancies include 40% to 60% Intradural Extramedullary (IDEM) tumours. The most common primary intradural extramedullary neoplasms are meningioma (20%-30%) and schwannoma (15%-50%), which are followed by neurofibroma, lipomas, and teratomas. They can be distinguished from intramedullary tumours by their extra-axial location [2].
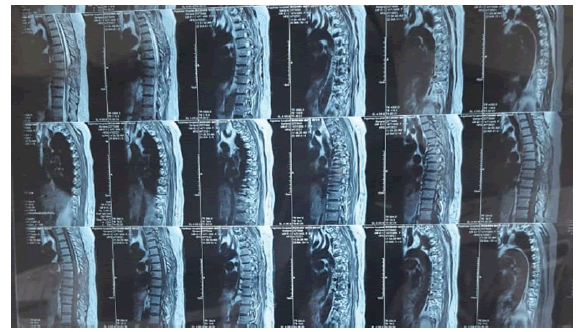
They induce a variety of neurological symptoms, including motor, sensory, sphincter, and a combination of these, in addition to pain syndromes. The diagnostic options include Computed Tomography (CT) scanning (bone windows with reconstruction), Magnetic Resonance Imaging (MRI) with contrast enhancement, and maybe CT myelograms [3].
We share our own prospective experience with 10 patients who received treatment over 2 years. Here, we examined the clinical, radiological, surgical, and histopathological aspects of ten patients with IDEM spinal cord tumours who underwent surgery with a single surgeon and assessed the surgical outcomes.
Majority of cases were diagnosed late because of the delayed seeking of medical attention possibly due to COVID-19 Pandemic.
Materials and Methods
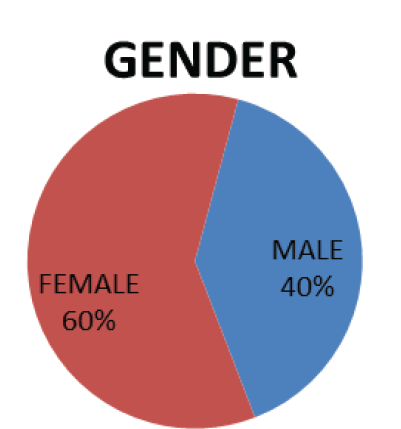
10 intradural extramedullary tumours were surgically removed between 2020 and 2022. At the Orthopaedics Department of Rajshree Medical and Research Institute, Bareilly, pre-operative, 3 months, 6 months, 1 year, and 2 year post-operative Karnofsky Performance Scores (KPSs) and Modified McCormick scale(MMS) studies were conducted. The patients, who were divided into 4 men and 6 women, had an average age of 61.7.
Inclusion Criteria
The study covered all patients who underwent surgery for primary solitary spinal IDEM tumours during the study period.
Exclusion criteria
The study eliminated patients who had multiple IDEM tumours or surgical treatments that limited their ability to function due to illness. The study did not include patients with spinal recurrent IDEM tumours.
Surgical Technique
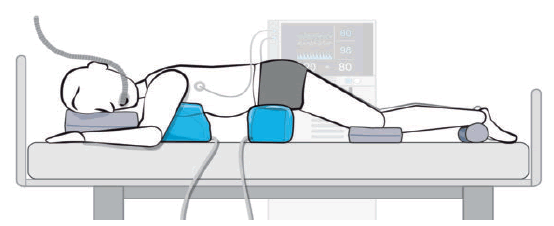
The patient was placed in the prone position under general anesthesia. The positioning was done in prone with bolsters under the chest, pelvis and under knee, with abdomen free (Fig. 1).
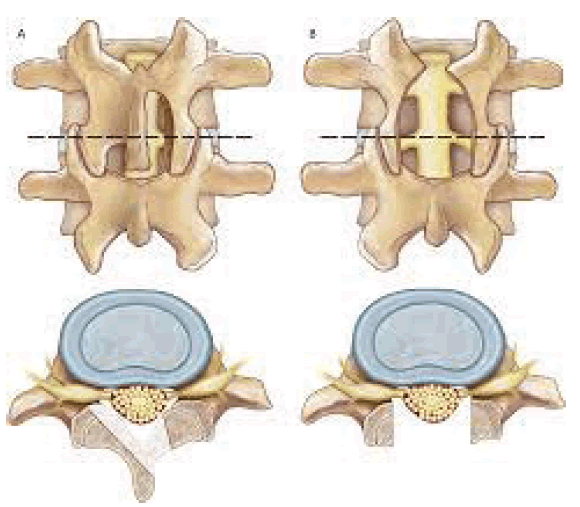
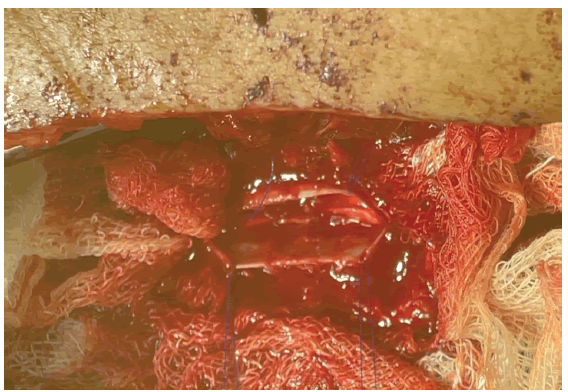
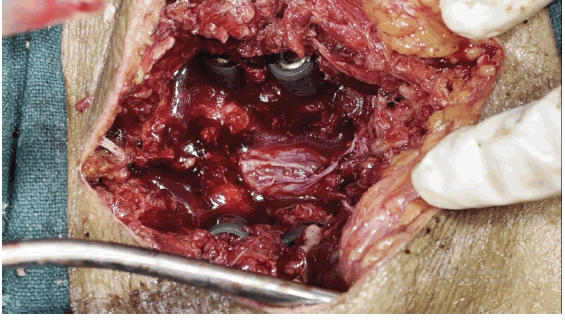
The tumour was carefully separated from the dura mater and excised. A nerve stimulator was utilised to identify whether a nerve fibre connected to a tumour was a sensory or motor nerve branch. The motor nerve branch was kept through cautious separation while the sensory nerve branch was eliminated. In cases when the tumour was so massive as to produce posterior instability, posterior interbody fusion with instrumentation was also carried out. Dura was repaired using Prolene 5-0 and spinal drain was placed in situ (Fig. 2,3).
Postoperative Evaluation
The Karnofsky Performance Scores and modified McCormick Score from before surgery and the most recent follow-up were compared as part of the postoperative examination of the neurological findings.
Result
PREOPERATIVE SYMPTOMS
Paresthesia/numbness was the most frequent preoperative complaint, which was followed by limb weakness in 70% of patients. Six patients (60%) had sphincter dysfunction, while four patients (40%) had dull aching or radicular pain. 40% of four patients experienced paraplegia (Fig. 4).
Six individuals reported symptoms that lasted longer than six months; four patients had symptoms that lasted less than six months. The typical time between symptoms was 6.4 months. The patients who reported with symptoms less than 6 months had better outcome in comparison with patients with symptoms more than 6 months in our study.
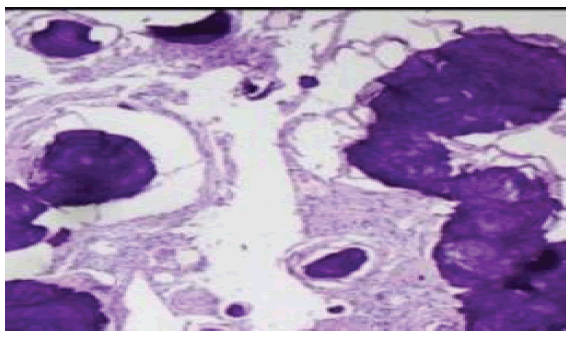
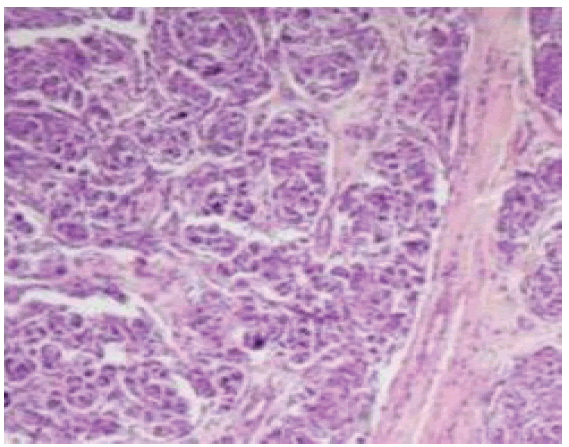
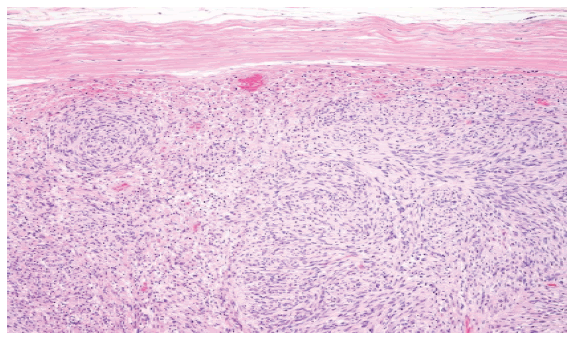
With the above mention surgical technique the tumor was completely excised and sent for histopathological (Biopsy) reporting (Fig. 5-7).
A post-operative MRI was performed to review the case and confirm the Tumour had been entirely removed (Fig. 8).
Post-operatively, steroids were started and then tapered off. 2 patients had complaints of persistent headache for which CSF leak was suspected. The re-exploration of surgical site was done and the CSF leak was repaired using Prolene 5-0.
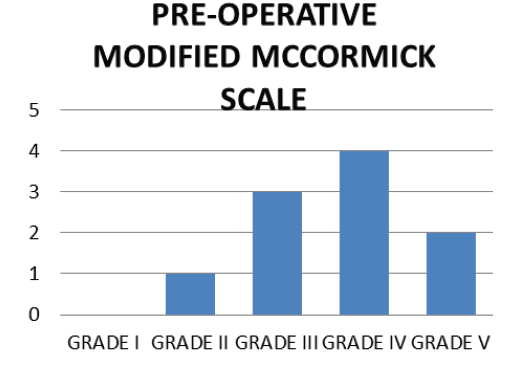
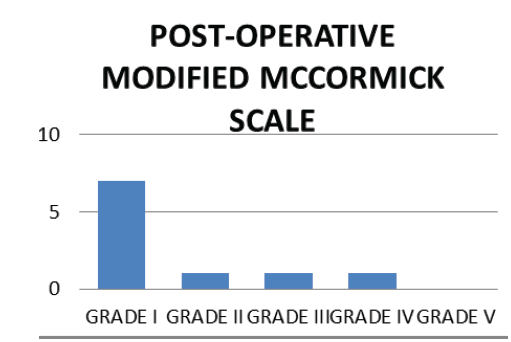
Outcomes: All patients’ symptoms and neurological signs improved post-operatively. There were 1 patient with Modified McCormick Scale grade I, 5 patient with Modified McCormick Scale grade II, 3 patients with grade III, 1 patients with grade IV pre-operatively.
Post-operatively, there were 1 patient with grade III, 3 patients with grade IV and 6 patients with Grade V (Fig. 9,10).
The maximum Karnofsky rating in this study was 70, and the study’s minimum Karnofsky score was 40. Histopathological reporting and biopsy was done and images are as follows (Fig. 11-13)
Follow Up: Follow up was done on 3 months, 6 months, 1 year and 2 years and during the study and follow up, Karnofsky Performance Status Scale and Modified McCormick Scale was evaluated and the values were calculated. The Karnofsky Performance Status Scale and Modified McCormick Scale changed significantly over a period of time with improvement of status/score from pre-op to 3 months to 6 months to 1 year to 2 year.Patients were followed up for a mean duration of 25.5 months with a range of 21 months-30 months.
The mean KPS increased significantly with improvement of score from Pre-operative to 3 months to 6 months to year to 2 year according to the p-value by ANOVA test (SPSS Version27.0).
The mean MMS decreased significantly with improvement of score from Pre-operative to 3 months to 6 months to 1 year to 2 year according to the p-value by ANOVA test(SPSS Version 27.0).
Discussion
The most prevalent primary Intradural Extramedullary (IDEM) tumours are meningiomas, which develop from arachnoid cap cells, and nerve sheath tumours (Schwannomas and Neurofibromas), which arise from sheath cells of spinal nerve roots [2].
The surgical removal of a spinal cord tumour involved a total laminectomy. This facilitates access and visualisation. Seppälä MT et al observed successful outcomes after surgically removing spinal schwannoma in a group of 187 individuals [4].
We examined 10 cases of IDEM tumours, of which 10 had undergone complete resections; whereas in a study conducted by Seppala et al., 62.5% patient undergone complete resection. Our study’s mean patient age at presentation was 61.7 years. Fachrisal et al. studies had a similar mean patient age at presentation of 43.4 years and a mean illness duration of 11.56 months [5]. The majority of our study’s patients were females (60%) whereas in a related study, males made up the majority of the patient population [5].
Meningiomas are more prevalent in women who are middle-aged or older and our research favour and confirm the notion that meningiomas are more common in women [6].
In a study by Stein BM et al., schwannomas were discovered in both males and females, but in our investigation, evidence of schwannomas was primarily found in males [7]. Schwannomas are more common in adults than in youngsters.
The majority of these IDEM tumour patients have spinal cord and/ or root compression symptoms. Local pain and/or radicular pain are frequent initial symptoms. Other frequent presentations include numbness and paresthesia [8].
Additionally, the clinical manifestation of sphincter dysfunction and paralysis were included in our study.
MRI is the best imaging modality for this tumour in terms of assessing the size, shape, and anatomical relationships with adjacent structures, particularly with dura matter and spinal cord, allowing best treatment guidelines and surgical approaches [9].
On T1W1 and T2W2 MRI images, spinal IDEM meningiomas exhibit hypo- to isointense signal. Strong homogeneous enhancement and the appearance of a dural tail are provided by gadolinium contrast on the dural attachment [7].
If accessible, intraoperative neurophysiological monitoring aids in lowering postoperative morbidity [8].
Additionally, our case study data confirms that neurophysiological monitoring lowers the incidence of neurological deficiency and postoperative morbidity.
Even long-lasting preoperative neurologic deficits may be alleviated and reversed postoperatively, and surgical outcomes for IDEM tumours are favourable. Although surgical resection is still the preferred form of treatment for the majority of IDEM tumours [9].
The pre-operatively mean KPS of the study of Fachrisal Et al was 74 whereas in our study, due to late presentation because of the COVID-19 Pandemic. The mean Pre-operative KPS score was 52, which indicates that there was evidence of a serious illness, serious difficulties with everyday tasks, and moderate difficulty with self-care.
A retrospective study conducted by Fachrisal et al with a study group of 88 patients had a KPS score average of 88 on follow-up post operatively, whereas our study had average KPS score of 74 [10]. This could be due to the delayed presentation for management and greater neurological deficit. In a study by Jesse CM et. al, majority of cases had a Mccormick grade of III and IV pre-operatively and post-operatively a grade of I and II, whereas in our study, 9 patients had a Mccormick grade of more than III pre-operatively, due to delayed presentation because of COVID-19 Pandemic and 7 patients had a Mccormick grade of I post-operatively [11]. CSF leak, pseudomeningocele, and wound infection are the most frequent postoperative side effects following IDEM tumour removal [3]. Spinal instability and additional neurological impairment are less common consequences and our study, 2 patients had post-operative complications of CSF leak [12, 13].
Conclusion
Gross complete surgical excision is often the best treatment option for intradural extramedullary tumours, which are typically benign, easily identified on MRI images.
On the basis of the Karnofsky Performance Status Scale, all patients in the series aside from one—had functional outcomes greater than 50.On the basis of clinical grading using the Modified McCormick Scale, all instances with the exception of three patients received a grade of 1.It was observed that earlier diagnosis of neurological involvement were associated with good prognosis.
References
- Sharma GR, Jha R, Poudel P, et al.Functional outcome of intradural extramedullary spinal tumors after surgical resection. Nepal J Neurosci,2016 Dec 1;13(2):73-80.[Google Scholar]
- Nair S, Menon G, Rao RM, et al. Essential practice of Neurosurgery. Kalangu KKN, Kato Y, Dechambenoit G (eds). Spinal tumors, Access publ. Co. Ltd, Nagoya, Japan. 1967;971:2009.[Google Scholar]
- Arnautovic K, Arnautovic A. Kenan arnautovic*, Aska Arnautovic. 9(Supplement1):40–45.[Google Scholar]
- Seppälä MT, Haltia MJ, Sankila RJ ,et al. Long-term outcome after removal of spinal schwannoma: a clinicopathological study of 187 cases. Journal of neurosurgery. 1995 Oct 1;83(4):621-6.[Google Scholar]
- Stein BM, McCormick PC. Spinal intradural tumors. In, Neurosurgery; Wilkin RH, Ranfachary SS (eds)Vol ii. 2nd ed. McCraw Hill, New York. PP 1769-1781, 1996[Google Scholar]
- Schroth G, Thron A, Guhl L, et al.. Magnetic resonance imaging of spinal meningiomas and neurinomas: improvement of imaging by paramagnetic contrast enhancement. J. neurosurg. 1987 May 1;66(5):695-700.[Google Scholar][CrossRef]
- Gottfried ON, Gluf W, Quinones-Hinojosa A,et al. Spinal meningiomas: surgical management and outcome. Neurosurg. focus 2003 Jun 1;14(6):1-7.[Google Scholar][Cross Ref]
- Korn A, Halevi D, Lidar Z, et al. Intraoperative neurophysiological monitoring during resection of intradural extramedullary spinal cord tumors: experience with 100 cases. Acta neurochirurgica. 2015 May;157:819-30.[Google Scholar][Cross Ref]
- Gerszten PC, Burton SA, Ozhasoglu C, McCue KJ, Quinn AE, et al. Radiosurgery for benign intradural spinal tumors. Neurosurgery. 2008 Apr 1;62(4):887-96.[Google Scholar][Cross Ref]
- Arnautovic K, Arnautovic A. Extramedullary intradural spinal tumors: a review of modern diagnostic and treatment options and a report of a series. Bosnian journal of basic medical sciences. 2009 Oct;9(Suppl 1):S40.[Google Scholar][CrossRef]
- Setiawan E, Alhuraiby SS. Functional outcome in intradural extramedullary tumor patients: Case series. Annals of Medicine and Surgery. 2020 Jun 1;54:71-3.[Google Scholar][CrossRef]
- Kumar R, Dhal AC, Kumar A. Case report: minimal invasive approach in a case of cervical schwannoma. Romanian Neurosurgery. 2017 Mar 15:115-21.[Google Scholar][Cross Ref]
- Jesse CM, Alvarez Abut P, et al.Functional Outcome in Spinal Meningioma Surgery and Use of Intraoperative Neurophysiological Monitoring. Cancers. 2022 Aug 18;14(16):3989.[Google Scholar][Cross Ref]




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.