Osteosynthesis of AO 13C distal humerus fractures using locking plates
Received: 09-Sep-2020 Accepted Date: Oct 12, 2020 ; Published: 30-Oct-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Fractures of distal humerus account for about 2%-6% of all fractures and 30% of all elbow fractures. Management of distal humerus fractures in adults is challenging. We aimed to evaluate functional and radiological outcome of surgical treatment of AO 13C distal humerus fractures in adults using locking plates.
Materials and methods: This is a prospective observational study conducted from October 2016 to September 2017 at a tertiary care center, after obtaining the institutional ethical clearance and written informed consent from patients. Around 32 adult patients (18 years to 75 years) undergoing surgical treatment for AO 13C distal humerus fractures were studied.
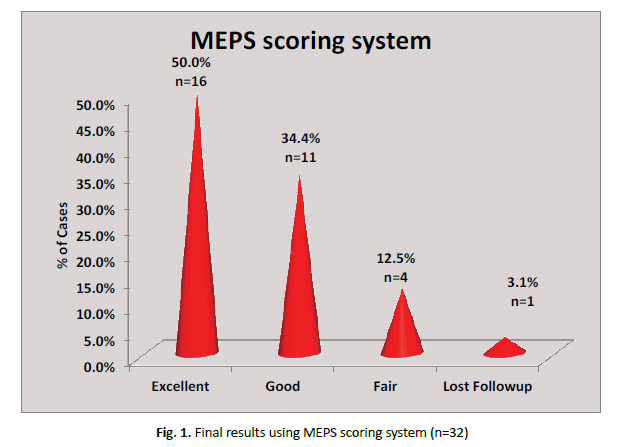
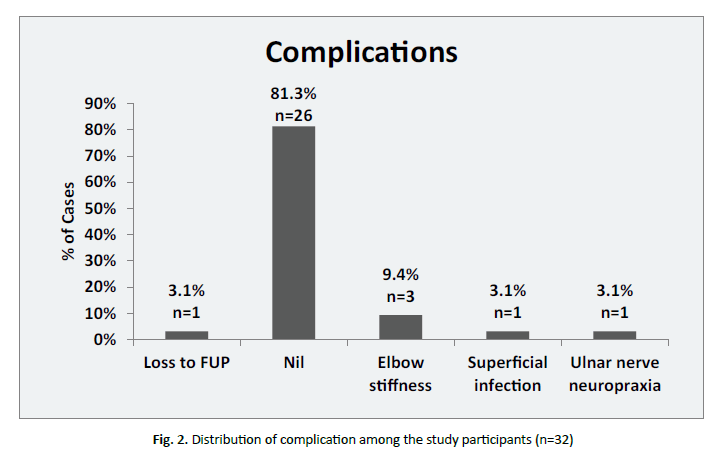
Results: The mean age was 43.75 ± 14.61 years ranging over 20-74 years. There were 15 Female and 17 Male patients in our study. There were 10 patients with type C1, 12 patients with type C2 and 10 patients with type C3 fractures in our study. Mean duration for radiological evidence for fracture union was 10.45 ± 1.43 weeks. Superficial infection in 1 patient, olecranon TBW breakage in 1 patient due to re-trauma, loss of follow up in 1 patient and elbow stiffness in 3 patients. Depending on mayo elbow performance score we had excellent results in 16 patients, good results in 11 patients, 4 patients had fair results and lost follow up of 1 patient.
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Keywords
Distal humerus, fracture, ORIF, double column plating, osteosynthesis; AO13C
Introduction
Distal humerus fractures in adults are relatively uncommon. They account for about 2%-6% of all fractures [1,2] and for about 30% of all elbow fractures [3]. There is a bimodal distribution with respect to the patient’s age and gender. The most common causes of these fractures are falls in the elderly population and sports injuries or road traffic accidents in the younger patients [4]. Up to now, the rareness of distal humerus fractures has prevented any single surgeon from gaining sufficient experience in managing the different fracture patterns, resulting in differing recommendations for treatment. Majority of the distal humerus fractures (96%) have a complex pattern involving both the columns and the articular surface (AO type C injuries) [5]. This situation has made the development of standardized treatment guidelines and implants desirable. Appropriate treatment should be based on a classification that describes the fracture pattern, is easily reproducible and allows development of treatment guidelines. Over the past two decades, the Muller AO classification [6] been the most accepted classification in the literature [7-13].
The only reliable method for restoring the normal alignment and contour of the distal humerus is operative exposure and direct manipulation of fracture fragments. However, fixation of fracture fragments must be stable enough to allow motion while ensuring union. The result was often elbow stiffness and delayed healing. In this context, non-operative treatments, such as the so-called bag of bones technique (a short duration of immobilization in either a cast or a collar and cuff followed by mobilization as tolerated) were established as treatment alternatives [14]. By the 1970s, the advent of the AO group and the introduction of new instrumentation and techniques helped the surgeons to achieve accurate anatomical reduction and stable internal fixation. This allowed early mobilization of the joint and gave satisfactory results [15]. Bicondylar intraarticular fractures of the distal humerus, because of their rarity and often associated significant displacement, comminution, and osteopenia, present the orthopaedician with a difficult injury to reliably treat successfully. As with any displaced intraarticular fracture, the principles of anatomic restoration of the articular surface, stable fixation, and early motion are the optimal treatment goals [16]. For fractures of the metaphyseal area, with or without joint involvement, many studies exist that show that best results are achieved if physical therapy is initiated early [13-19]. Without doubt, the main prerequisites for early postoperative motion are stable fracture fixation and anatomical joint restoration [13,20]. However, it is also known that this goal is often difficult to obtain.
Although it is wise to be prepared to perform a total elbow arthroplasty in the event that a complex fracture is not amenable to internal-fixation, one must keep in mind the functional limitations and eventual failure associated with total elbow arthroplasty. A surgeon treating a healthy active patient with a fracture of distal humerus should make every attempt to reconstruct and preserve the distal humerus [21]. AO 13C distal humerus fractures has been subject of interest for me because of complex articular anatomy and a challenge for the surgeons to restore the articular anatomy and function of elbow joint. This study mainly deals with the outcome of intercondylar fractures of distal humerus using locking plates and its functional outcome. These fractures demand accurate reduction and stable internal fixation to avoid disability from malunion and arthrofibrosis of elbow.
We aimed to study and evaluate functional and radiological outcome of surgical treatment of AO 13C distal humerus fractures in adults using locking plates and to study the range of movement of elbow following distal humerus fracture fixation with dual plating and to assess complications associated with dual plating of distal humerus.
Methodology
This is a prospective observational study conducted at tertiary care institute, after obtaining the ethical clearance from institutional ethical committee and written informed consent from participating patients. This study was conducted in our institute from October 2016 to September 2017. All adult patients (18 years to 75 years) undergoing surgical treatment for AO 13C distal humerus fractures were studied.
The proportion of patients with good to excellent outcome found in previous studied articles ranges from 70%-95% [22]. All patients with AO 13C closed fractures of both sex between the age of 18 and 75 years willing to participate in the study, with minimum follow-up period of 6 months were included. Pregnant female patients, patients with neuro muscular disorders affecting upper limbs, patients with pathological fractures except osteopenia and osteoporosis, patients with paralyzed upper limb with distal humerus fracture, patients for revision surgery and, patients with pre-existing upper limb congenital deformity were excluded from the study.
On admission, all patients will undergo a primary survey and hemodynamic stabilization in the emergency department. Appropriate antero-posterior and lateral radiographs and CT scan (if required) were taken. The presence of other fractures, neurovascular status of the limb and systemic evaluation will be done subsequently on secondary survey. The limb was immobilized in the form of above elbow plaster slab or crammer wire splintage temporarily. The fractures were classified using the method of AO classification [6]. After obtaining a proper consent patient were enrolled in the study. Preoperative investigations and preparations (accordingly) were done in all patients. Patients were operated as early as possible once the general condition of the patients were stable and is fit for surgery after proper pre-operative preparation. All patients were treated surgically using posterior trans-olecranon approach with ulnar nerve exploration and fixation using locking plates and tension band wiring for olecranon osteotomy.
Post-operatively, mobilization of the elbow and weight lifting ambulation on normal side but non weight lifting on affected side were advised as early as possible. Sutures were removed on the 12th day of surgery. X ray of the involved limb will be taken postoperatively. Patients were allowed partial weight lifting and subsequently full weight lifting depending on the fracture union and patient compliance. Further, monthly follow up was done for 2 months and then for every 2 months till 6 months. Serial x-rays were taken at 1 month, 2 months, 4 months and 6 months. Patients were advised not to lift heavy weight or exert the affected upper limb. The Post-operative follow up period ranged from 6 months to 12 months and the minimum follow up period was 6 months. Evaluation was done using Mayo Elbow performance Score at 1 month, 2 months, 4 months and 6 months. The functional assessment of the patient was done according to Mayo Elbow Performance Score (MEPS).
Results
In our study, distribution of age was between 20-74 years, the average age was 43.75 ± 14.61 years (Table 1).
| S. No. | Variable | Frequency | Percentage |
|---|---|---|---|
| 1 | Age | ||
| 20-40 | 16 | 50 | |
| 41-60 | 12 | 37.5 | |
| >60 years | 4 | 12.5 | |
| 2 | Gender | ||
| Male | 17 | 53.1 | |
| Female | 15 | 47.9 | |
| 3 | Mode of injury | ||
| Fall | 11 | 34.4 | |
| Rta | 21 | 65.6 | |
| 4 | Laterality of fracture | ||
| Left | 13 | 40.6 | |
| Right | 19 | 59.4 | |
| 5 | AO type | ||
| C1 | 10 | 31.3 | |
| C2 C3 |
12 10 |
37.5 31.3 |
|
| 6 | Associated injuries | ||
| Nil | 25 | 78.1 | |
| Abrasion | 1 | 3.1 | |
| Distal end radius | 1 | 3.1 | |
| Facial injury | 1 | 3.1 | |
| Head injury | 1 | 3.1 | |
| Pelvic injury | 1 | 3.1 | |
| Ulna fracture | 1 | 3.1 | |
| Radial nerve palsy | 1 | 3.1 | |
| 7 | Time duration between trauma and surgery | ||
| ≤10 hours | 16 | 50 | |
| 10-24 hours | 13 | 40.6 | |
| ≥24 hours | 3 | 9.4 | |
| 8 | Implants used | ||
| Titanium | 6 | 18.7 | |
| Stainless steel | 26 | 81.3 | |
| 9 | Union rates | ||
| 8-10 weeks | 15 | 46.9 | |
| 11-15 weeks | 16 | 50 |
Table 1. Distribution of demographic data among the participants (n=32)
There were 17 males and 15 females in our study. Male patients constituted 53.1% and female were 46.9%. Around 21 (65.6%) patient’s sustained fractures following Road Traffic Accidents. We had 16 patients (50.0%) operated within 10 hours of trauma and three patients (9.4%) operated after 24 hours of trauma. In 32 patients, 15 patients (46.9%) had union between 8-10 weeks and one patient (3.1%) had lost to follow up.
In our study, the mean ROM at 1 month was 79.03 ± 10.44, at 2 months was 98.71 ± 7.18, at 4 months was 109.35 ± 8.54, and at 6 months was 120.32 ± 9.83. In our study, the mean functional MEPS score at 1 month was 64.35 ± 9.46, at 2 months was 73.87 ± 9.19, at 4 months was 82.26 ± 10.48, and at 6 months was 89.52 ± 12.67. (Table 2) Out of 32 patients, final results using MEPS scoring system excellent outcome is noticed in 16 patients (50%), good results are noticed in 11 patients (34.4%), fair result is noticed in 4 patients (12.5%) and 1 patient (3.1%) is omitted as we lost follow up. So, the results were quantified for 31 patients omitting 1 patient of which the follow up was lost (Fig. 1).
| S. No. | Variable | Mean (SD) | p value |
|---|---|---|---|
| 1 | Range of Motion | ||
| 1st month | 79.03 ± 10.44 | <0.001 | |
| 2nd month | 98.71 ± 7.18 | ||
| 4th month | 109.35 ± 8.54 | ||
| 6th month | 120.32 ± 9.83 | ||
| 2 | MEPS score | ||
| 1st month | 64.35 ± 9.46 | <0.001 | |
| 2nd month | 73.87 ± 9.19 | ||
| 4th month | 82.26 ± 10.48 | ||
| 6th month | 89.52 ± 12.67 |
Table 2. Postoperative characteristics of the study participants (n=31)
Range of motion at 1 month, 2 months, 4 months and 6 months is measured. There was no significant difference between ROM, and MEPS with fracture type in our study group (Table 3).
| AO classification | P Value | C1 V/S C2 | C1 V/S C3 | C2 V/S C3 | |||
|---|---|---|---|---|---|---|---|
| C1 | C2 | C3 | |||||
| Mean ± SD | Mean ± SD | Mean ± SD | |||||
| ROM | |||||||
| 1st month | 76.00 ± 9.66 | 80.83 ± 11.65 | 79.00 ± 9.94 | 0.568 | 0.539 | 0.801 | 0.913 |
| 2nd month | 96.00 ± 9.66 | 99.17 ± 2.89 | 100.00 ± 8.17 | 0.436 | 0.572 | 0.445 | 0.961 |
| 4th month | 108.89 ± 12.69 | 109.17 ± 6.69 | 110.00 ± 6.67 | 0.959 | 0.997 | 0.960 | 0.974 |
| 6th month | 120.00 ± 12.25 | 120.00 ± 8.53 | 121.00 ± 9.94 | 0.968 | 1.000 | 0.975 | 0.971 |
| MEPS | |||||||
| 1st month | 62.00 ± 11.35 | 63.33 ± 9.37 | 68.00 ± 6.33 | 0.324 | 0.940 | 0.330 | 0.476 |
| 2nd month | 73.00 ± 9.19 | 72.08 ± 10.76 | 77.00 ± 6.33 | 0.429 | 0.97 | 0.592 | 0.426 |
| 4th month | 81.11 ± 12.94 | 80.83 ± 12.03 | 85 ± 5.27 | 0.618 | 0.998 | 0.710 | 0.637 |
| 6th month | 87.78 ± 12.78 | 87.5 ± 15.45 | 93.5 ± 8.52 | 0.497 | 0.999 | 0.599 | 0.525 |
Table 3. Comparison of trend of range of motion and MEPS score in different AO classifications
Table 4 shows that out of 14 female patients, 4 (28.6%) had excellent, 8 (57.1%) had good and 2 (14.3%) had fair results. Whereas out 17 male patients 12 (70.6%) had excellent, 3 (17.6%) had good and 2 (11.8%) had fair results. On overall, 16 (51.6%) patients had excellent, 11 (35.5%) had good and 4 (12.9%) patients had fair results. We had 16 patients operated within 10 hours of trauma out of which 10 (62.5%) had excellent, 2 (12.5%) had good and 4 (25.0%) had fair results. We had 8 patients operated between 11-20 hours of trauma out of which 3 (37.5%) had excellent and 5 (62.5%) had good results and 2 patients operated after 30 hours of trauma of which both the patients had excellent results.
| S. No. | Variable | Total cases | Result | p Value | ||
|---|---|---|---|---|---|---|
| 1 | Excellent (%) | Good (%) | Fair (%) | |||
| Gender | ||||||
| Female | 14 | 4 (28.6%) | 8 (57.1%) | 2 (14.3%) | 0.049 | |
| Male | 17 | 12 (70.6%) | 3 (17.6%) | 2 (11.8%) | ||
| 2 | Age | |||||
| 20-40 | 16 | 11 (68.8%) | 3 (18.8%) | 2 (12.5%) | 0.045 | |
| 41-60 | 11 | 5 (45.5%) | 4 (36.4%) | 2 (18.2%) | ||
| >60 years | 4 | 0 (0.0%) | 4 (100%) | 0 (0.0%) | ||
| 3 | Associated injury | |||||
| Nil | 24 | 13 (54.2%) | 8 (33.3%) | 3 (12.5%) | 0.373 | |
| Abrasion | 1 | 0 (0.0%) | 1 (100%) | 0 (0.0%) | ||
| Distal end radius | 1 | 0 (0.0%) | 1 (100%) | 0 (0.0%) | ||
| Facial injury | 1 | 0 (0.0%) | 1 (100%) | 0 (0.0%) | ||
| Head injury | 1 | 1 (100%) | 0 (0.0%) | 0 (0.0%) | ||
| Pelvic injury | 1 | 1 (100%) | 0 (0.0%) | 0 (0.0%) | ||
| Ulna fracture | 1 | 1 (100%) | 0 (0.0%) | 0 (0.0%) | ||
| Radial nerve palsy | 1 | 0 (0.0%) | 0 (0.0%) | 1 (100%) | ||
| 4 | Time duration between trauma and surgery | |||||
| 6-10 hours | 16 | 10 (62.5%) | 2 (12.5%) | 4 (25.0%) | 0.032 | |
| 11-20 hours | 8 | 3 (37.5%) | 5 (62.5%) | 0 (0.0%) | ||
| 21-30 hours | 5 | 1 (20.0%) | 4 (80.0%) | 0 (0.0%) | ||
| >30 hours | 2 | 2 (100%) | 0 (0.0%) | 0 (0.0%) | ||
Table 4. Association of demographic variable with the final outcome (n=31)
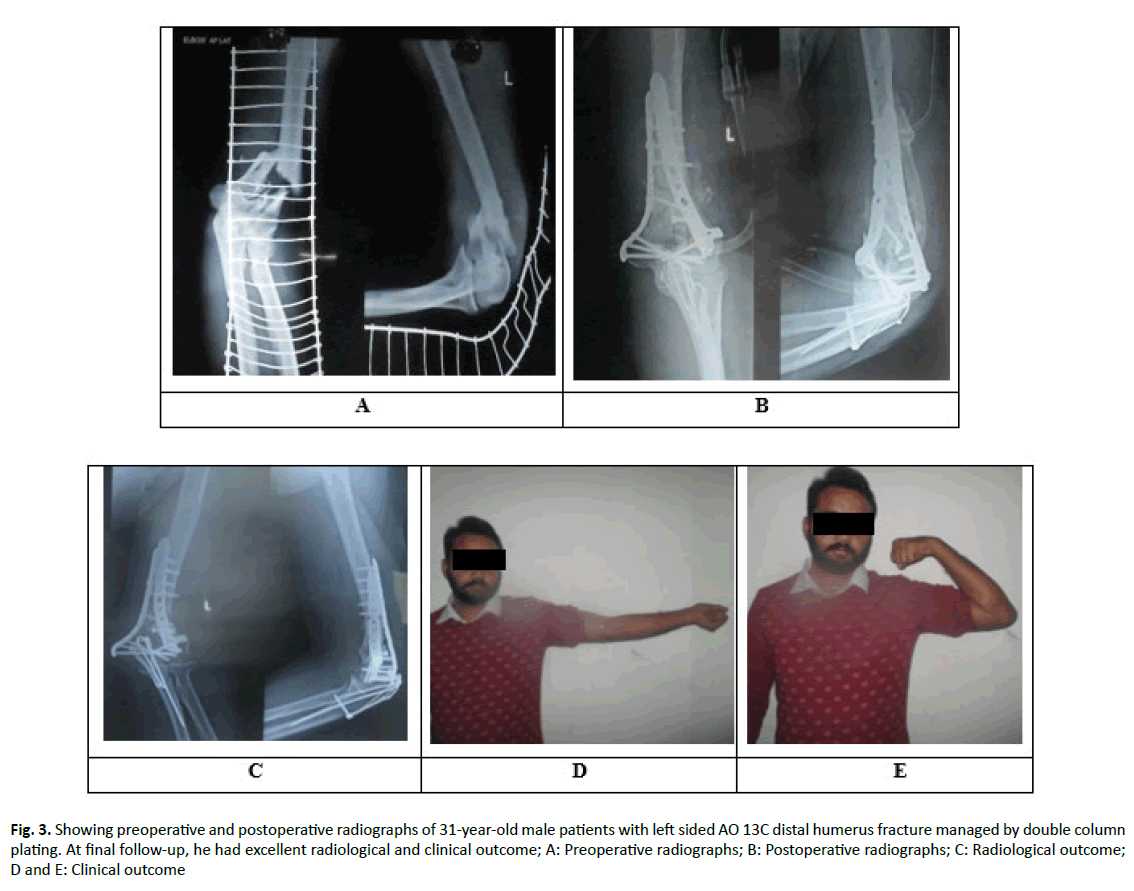
In 32 patients in our study, 1 patient (3.1%) had superficial infection, 1 patient (3.1%) had ulnar nerve neuropraxia which recovered in 3 weeks, in 1 patient (3.1%) we lost follow-up after 2 months of regular follow-up and 3 patients (9.4%) developed stiff elbow (Fig. 2 and 3).
Figure 3: Showing preoperative and postoperative radiographs of 31-year-old male patients with left sided AO 13C distal humerus fracture managed by double column plating. At final follow-up, he had excellent radiological and clinical outcome; A: Preoperative radiographs; B: Postoperative radiographs; C: Radiological outcome; D and E: Clinical outcome
Discussion
The management of distal humerus fractures has been of particular interest to orthopaedic surgeons particularly when associated with osteoporosis or severe communition. They are often difficult to treat, and functional results are poor. Distal humerus fractures are commonly seen in young males and a severe fracture is associated with poor outcome that can affect the socioeconomic status of the patient in the long run.
Open reduction and internal fixation with double plating is the gold standard treatment for distal humerus fractures [14]. Open reduction internal fixation with dual plating helps to reduce intercondylar fragments provide much stability to allow immediate post-operative range of mobility of elbow which can improve final outcome. Fractures and fracture-dislocations involving the elbow joint usually produce extensive soft tissue injury along with the bony injury. Fractures extending into the joint in either children or adults often require open reduction and internal fixation, but treatment should be individualized. Non operative measures often fail if articular surfaces are involved.
If open reduction of fracture is delayed, the best time for surgery may be lost and can lead to soft tissue contractures, myositis ossificans and much more difficult reconstructive procedures are more likely. Regardless of the method of treatment, substantial damage to the distal humerus usually results in some limitation of motion, pain, weakness, and possibly instability. Even minor irregularities of the joint surface of the elbow usually cause some loss of function. This can usually be minimized by early, accurate open reduction with sufficiently rigid fixation by dual plating to permit immediate motion. In cases of open reduction and internal fixation several factors influence the stability of fixation like: quality of bone, type of fixation device, number and size of fracture fragments, condition of soft tissues after injury [23].
Jacobson et al. [24] compared 5 different combinations of multiple plates in the fixation of distal humerus fractures and found that the orthogonal plate configuration provided the greatest sagittal plane stiffness. Cadaveric study by Schemitsch et al. [25] showed that medial and lateral plating provided the greatest rigidity when there was the presence of a comminution gap. The use of locking screws creates a fixed angle construct. This plate-screw construct resists cantilever bending stresses, reducing the risk of angular deformity in comminuted metaphyseal fractures. In this study, the fractures were common in the 20-40 years age group, with mean age of 43.75 ± 14.61. In this study, there was a bimodal distribution of patients with 16 patients between 20-40 years and the most common mode of injury in these patients was road traffic accident. This could be due to increased mobility in urban youth. In this study, we had a male preponderance with 53.1% and 46.9% female patient, which is comparable to Henley et al. study. In his study, Jupiter et al. [1] noted about 47% male and 53% female, sex distribution and Gabel et al noted about 38% male and 62% female incidence.
In this study, 65.6% of cases were due to road traffic accident and 34.4% of cases were due fall. Henley et al. [26] accounted 61% of his cases to road traffic accident and 39% due to direct fall. Wang et al. [27], accounted 70% of the cases to road traffic accident and 30% of the cases to direct fall and accounted 42.3% of the cases to road traffic accident and 54% of the cases to direct fall. The results of Henley et al. are comparable with our study [26].
In this study, 59.4% of patients suffered injury to right side and 40.6% of patients suffered on left side. Jupiter et al. [1] reported about 38% incidence of fractures in right distal end of humerus. Henley et al. [26] reported about 45% incidence of fractures in right side distal end of humerus. Wang et al. [27], study reported about 70% incidence in right side and 30% in left side. Right-sided predominance is probably due to direct fall injury on to the predominant side that is right in our study. The delay in surgery time was due to physician clearance due to any other medical or surgical co-morbidities especially in elderly patients or due to late presentation to our center. Patients without any co morbidities were taken up within 24 hours of trauma.
Dual-plate fixation has been described by several authors and seems to provide the most secure fixation. Helfet and Hotchkiss [23] studied the rigidity and fatigue performance of several methods including the dual-plate fixation. Although there are many fixation constructs, the biomechanical behavior of the osteosynthesis depends more on plate configuration than plate type in this study, all patients were operated by orthogonal plating. Olecranon osteotomy for exposure and fixation of the distal humeral fracture was initially popularized by Cassebaum [28]. Olecranon osteotomy is the most frequently used surgical route to expose the distal humerus for AO type C fractures [29]. The K-wire/ tension band fixation of the olecranon site allows early range- ofmotion exercise of the elbow joint, thereby promoting bone healing the choice of approach was based on operating surgeon’s preference and orientation [30].
We had better results in patients aged less than 39 years compared to patients more than 40 years’ age. We had better results in male patients as compared to female patients which could be because of poor pain tolerance in females.
This could be due to the good physiotherapy protocol followed correctly by young and male patients. There were differences in functional outcome between AO type C1, C2 and C3 fractures with respect to flexion ROM arc and MEPS score at 6 months but these differences were not statistically significant. However, the significant improvement in outcome and arc of motion of elbow in each fracture type from 2 months to 6 months is attributed to the physiotherapy [28,29].
Conclusion
Open reduction and internal fixation of AO TYPE 13C fractures is challenge to orthopaedic surgeon, preoperative planning and mastering the technique over a period of time gives good to excellent functional outcomes. Radiological union in all fractures was with an average of 10.45 ± 1.43 weeks. Adequate analgesia during post operative care allowed patients to undergo good physiotheraphy and regain good range of motion of elbow. Finally, we conclude that internal fixation of intra-articular distal humerus (AO type C) fractures using double column locking plates is an effective procedure ensuring stability of fixation and thereby permitting early range of motion resulting in good to excellent functional outcomes in most patient age groups. Key to successful surgical treatment in such cases, is a well planned and designed surgical scheme ‘‘tailored’’ on the specific fracture type and soft tissue condition, combined with a high level of surgical skill and experience. Early range of motion physiotherapy should be advised to obtain good functional and clinical results. We strongly recommend timely intervention, intra operative expertise with meticulous soft tissue handling to achieve favourable results.
REFERENCES
- Jupiter J.B., Morrey B.F.: Fractures of the distal humerus in the adult. In: Morrey BF, ed. The Elbow and its Disorders. 2nd ed. Philadelphia Pa: WB Saunders. 1993:328-336.
- Robinson C.M., Hill R.M., Jacobs N., et al.: Adult distal humeral metaphyseal fractures: epidemiology and results of treatment. J Orthop Trauma. 2003;17:38-47.
- Rose S.H., Melton III L.J., Morrey B.F., et al.: Epidemiologic features of humeral fractures. Clin Orthop. 1982;168:24-30.
- Lill H., Korner J., Josten C.: Fractures of the distal humerus. In: Josten C, Lill H, eds. Elbow Injuries, Biomechanics, Diagnostics, Therapy. Darmstatt: Steinkopff. 2001:163-182.
- McCarty L.P., Ring D., Jupiter J.B.: Management of distal humerus fractures. Am J Orthop. 2005;34:430-438.
- Muller M.E.: The comprehensive classification of fractures of long bones. In: Müller M.E., Allgöwer M., Schneider R., et al., eds. Manual of internal fixation. 3rd ed. Berlin. 1991:118-150.
- Gambirasio R., Riand N., Stern R., et al.: Total elbow replacement for complex fractures of the distal humerus. An option for the elderly patient. J Bone Joint Surg Br. 2001;83:974-978.
- Haas N., Hauke C., Schutz M., et al.: Treatment of diaphyseal fractures of the forearm using the point contact fixator (PC-Fix): results of 387 fractures of a prospective multicentric study (PC-Fix II). Injury. 2001;32(suppl 2):51-62.
- Henley M.B., Bone L.B., Parker B.: Operative management of intra-articular fractures of the distal humerus. J Orthop Trauma. 1987;1:24-35.
- John H., Rosso R., Neff U., et al.: Operative treatment of distal humeral fractures in the elderly. J Bone Joint Surg Br. 1994;76:793-796.
- Kinzl L., Fleischmann W.: The treatment of distal upper arm fractures. Unfallchirurg. 1991;94:455-460.
- Rommens P.M.: Fractures of the distal third of the humerus. In: Flatow E.C., ed. Muskuloskeletal Trauma Series; Humerus. Oxford, England: Butterworth Heinemann. 1996:156-183.
- Sanders R.A., Raney E.M., Pipkin S.: Operative treatment of bicondylar intraarticular fractures of the distal humerus. Orthopaedics. 1992;15:159-163.
- Jupiter J.B., Neff U., Holzach P., et al.: Intercondylar fractures of the humerus. An operative approach. J Bone Joint Surg Am. 1985;67:226-239.
- Muller M.E., Allgower M., Schneider R., et al.: Manual of internal fixation techniques recommended by the AO group, 2nd ed. New York. 1979.
- Helfet D.L., Schmeling G.J.: Bicondylar intraarticular fractures of the distal humerus. Clin Orthop Relat Res. 1993;292:26-36.
- Bauer G.J., Hoellen I.P.: The distal intraarticular humerus fracture: diagnostics, surgical technique, results. Akt Traumat. 1997;27:125-131.
- Gupta R.: Intercondylar fractures of the distal humerus in adults. Injury. 1996;27:569-572.
- Korner J., Lill H., Verheyden P., et al.: Complex fractures of the elbow joint. Management and Results. Akt Traumat. 1998;11:205-215.
- Ring D., Jupiter J.B.: Fractures of the distal humerus. Orthop Clin North Am. 2000;31:103-113.
- Holdsworth B.J., Mossad M.M.: Fractures of the adult distal humerus: Elbow function after internal fixation. J Bone Joint Surg Br. 1990;72:362-365.
- Greiner S., Haas N.P., Bail H.J.: Outcome after open reduction and angular stable internal fixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP distal humerus system. Arch Orthop Trauma Surg. 2008;128:723-729.
- Helfet D.L., Hotchkiss R.N.: Internal fixation of the distal humerus: A biomechanical comparison of methods. J Orthop Trauma. 1990;4:260-264.
- Jacobson S.R., Glisson R.R., Urbaniak J.R.: Comparison of distal humerus fracture fixation: a biomechanical study. J South Orthop Assoc. 1997;6:241-249.
- Schemitsch E.H., Tencer A.F., Henley M.B.: Biomechanical evaluation of methods of internal fixation of the distal humerus. J Orthop Trauma. 1994;8:468-475.
- Henley B.M.: Intra-articular distal humeral fractures in adults. Orthop Clin North Am. 1987;18:11-23.
- Wang K.C., Shih H.N., Hsu K.Y., et al.: Intercondylar fractures of the distal humerus: routine anterior subcutaneous transposition of the ulnar nerve in a posterior operative approach. J Trauma. 1994;36:770-773.
- Cassebaum W.H.: Open reduction of T and Y fractures of the lower end of the humerus. J Trauma. 1969;9:915-925.
- Coles C.P., Barei D.P., Nork S.E., et al.: The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. J Orthop Trauma. 2006;20:164-171.
- McKee M.D., Wilson T.L., Winston L., et al.: Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. J Bone Joint Surg Am. 2000;82-A:1701-1707.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.