Management of sports related and recreational knee injuries in children: surgical aspects
Received: 27-Jun-2021 Accepted Date: Jul 15, 2021 ; Published: 25-Jul-2021, DOI: 10.37532/1897-2276.2021.16(1).30
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Sports-related knee injuries are common in children and the management of these injuries continues to evolve. Sports injuries in children affect both growing bone and soft tissues and can result in damage of growth mechanisms with subsequent lifelong, growth disturbance. With an increasing number of paediatric and adolescent athletes presenting with knee injuries due to sports, a greater demand is put on clinicians and radiologists to assess the specific type of knee injury.
Traumatic forces applied to the immature skeleton cause a different type of injury than those seen in adults due to the differences in vulnerability of the musculoskeletal system, especially at the site of the growth cartilage. An overview of several sport-related knee injuries of young athletes is presented, based on anatomical location and their management. The training programmes should be considered an important training tool that growing athletes can adjust to the changes in their bodies and could prevent knee injuries.
Keywords
sports-related Knee Injuries in children, Knee injuries in adolescent sports players
Introduction
Physical activity is an important component of health and well‐being for people of all ages [1,2]. It has been directly linked to increased physical competency, decreased health risks, decreased body mass index, and increased social interaction 3. Physical activity also carries a risk of injury which can exact psychological, emotional, physical, social, and economic tolls [3-6]. Participation in physical activities such as sports and recreation has been identified as a strong risk factor for knee injury [4-10].
Knee is the most injured joint by adolescent athletes [7-9]. Prevention is important because a knee injury can end an athlete’s competitive career and can permanently affect physical activity capabilities among individuals of all ages. Additionally, while knee injuries can have economic effects on the injured individuals, they also pose a burden on the health care system [11]. Knee injuries are reported to account for 60% of high school sports‐related surgeries, and female athletes have been reported to be four to six times more likely to sustain a major knee injury [12].
Additionally, researchers have attributed the vulnerability of female knees to numerous factors, including anatomical, environmental, hormonal, neuromuscular, and biomechanical differences [13,14]. Increased use of indoor electronic games meant that young people spend less amount of time in sports-related physical activities. There has been an increased incidence of obesity in children [15].
The knee joint is one of the most common sites of injuries in the skeletally immature patient, with the spectrum of injuries differing from those in adults. children are not ‘little adults’ and have different physiology, anatomy, presence of growth plate (weak area), different blood supply and weak surrounding muscle strength and mechanics [16].
Sports‐related knee injury prevention efforts include a variety of approaches such as sport‐specific skills training (e.g., planting and changing direction, jumping/landing); strengthening and conditioning programs aimed to address potential deficits in the neuromuscular strength and coordination of stabilizing muscles about the knee joint; and combined programs of stretching, plyometrics, and strength training drills [17,18].
This article is focused to present a case series of knee injuries in children that happened during various sports and recreation and their management. These patients were managed in our institution with various modalities of treatment depending on the type of Knee injuries. In addition, we set out to study the associations between age, sex and types of knee injuries.
Materials and Methods
An electronic search of the PubMed, EMBASE, and Google Scholar databases for keywords related to knee sports-related injuries’ and ‘adolescent and athletes’ was performed. Each manuscript was individually reviewed. For all cases of knee injuries in children secondary to sports, presentation, treatment, and outcome were recorded. Papers were selected based on expert opinion and consensus by the authors and included if deemed to have contributed important findings to the above topics.
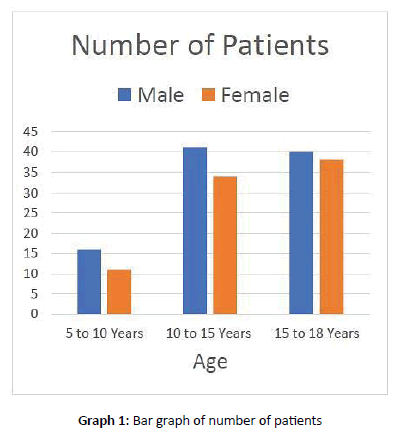
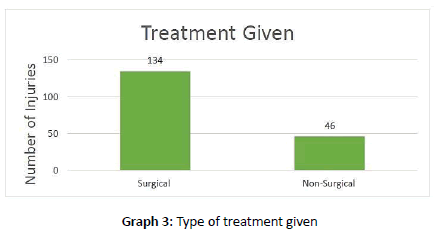
It is a retrospective descriptive study. Clinical and radiological Hospital records of knee injuries in
children, from 2000 to 2021, were randomly selected as a regional representative sample from 180 patients with sports-related and recreational knee injuries from our institution. Patient demographics as well as mechanism of injury and treatment offered were recorded. Data was segregated according to various variable like age, sex, type of injuries and treatment given. (Tables 1 and 2 and Graphs 1-3).
| Age | Male | Female | Number of Patients |
|---|---|---|---|
| 5 to 10 Years | 16 | 11 | 27 |
| 10 to 15 Years | 41 | 34 | 75 |
| 15 to 18 Years | 40 | 38 | 78 |
| Total | 97 | 83 | 180 |
Table 1. Data is collected from hospital records with epidemiological distribution among both sexes
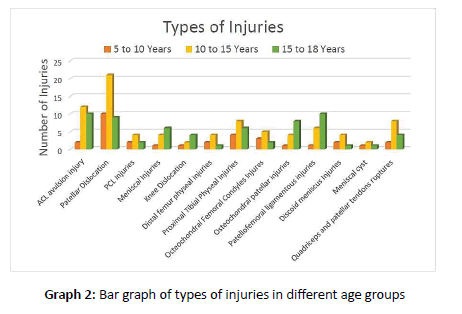
| Types of Injuries | 5 to 10 Years | 10 to 15 Years | 15 to 18 Years | Total |
|---|---|---|---|---|
| ACL avulsion injury | 2 | 12 | 10 | 24 |
| Patellar Dislocation | 10 | 21 | 9 | 40 |
| PCL Injuries | 2 | 4 | 2 | 8 |
| Meniscal Injuries | 1 | 4 | 6 | 11 |
| Knee Dislocation | 1 | 2 | 4 | 7 |
| Distal femur physeal injuries | 2 | 4 | 1 | 7 |
| Proximal Tibial Physeal Injuries | 4 | 8 | 6 | 18 |
| Osteochondral Femoral Condyle Injures | 3 | 5 | 2 | 10 |
| Osteochondral patellar injuries | 1 | 4 | 8 | 13 |
| Patellofemoral ligamentous injuries | 1 | 6 | 10 | 17 |
| Discoid meniscus Injuries | 2 | 4 | 1 | 7 |
| Meniscal cyst | 1 | 2 | 1 | 4 |
| Quadriceps and patellar tendons ruptures | 2 | 8 | 4 | 14 |
Table 2. Type of injuries for all age groups
Cases and their management
Following are the details of various sports-related knee injuries of young patients and treatment offered and algorithm.
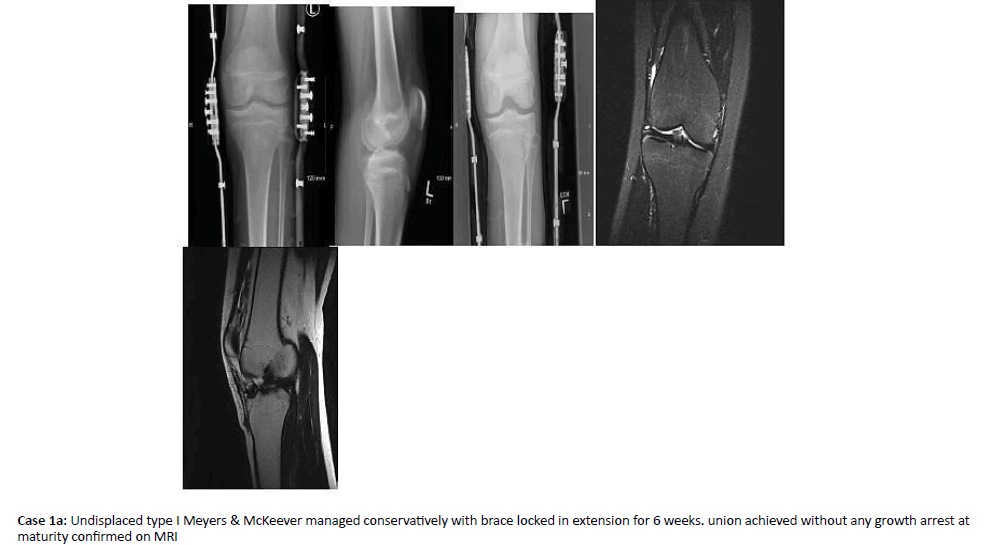
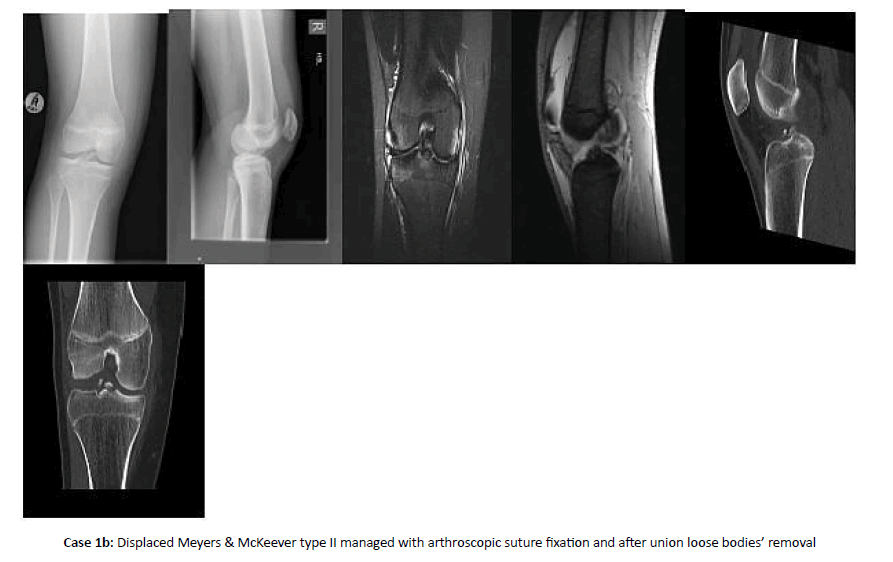
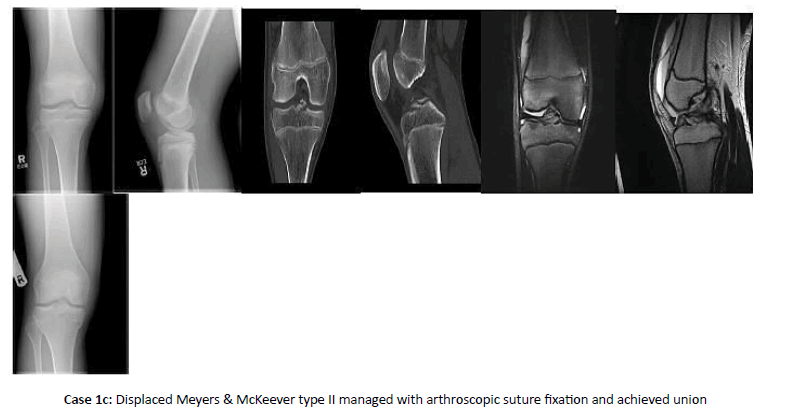
Case 1: ACL Tibial spine avulsion injury
ACL Tibial spine avulsion injury is shown in Cases 1a, 1b, and 1c
Note: We managed Modified Meyers and McKeever non-displaced type I and reducible type II fractures by immobilization in full extension.
Type III or Type II fractures that cannot be reduced were managed by Arthroscopic fixation using suture. These patients were safely and more appropriately treated with transphyseal reconstruction using small 7 mm-8 mm drill holes and Fibre wire sutures. Patients and parents were counselled that there remains a small risk of physical injury and a possibility of additional surgery for angular or growth disturbance.
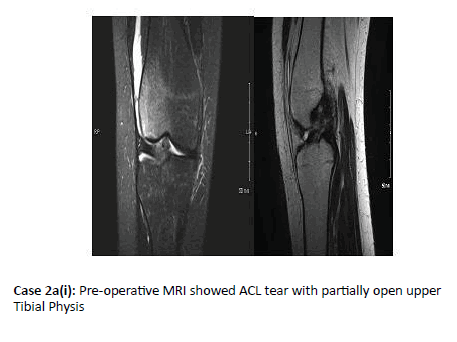
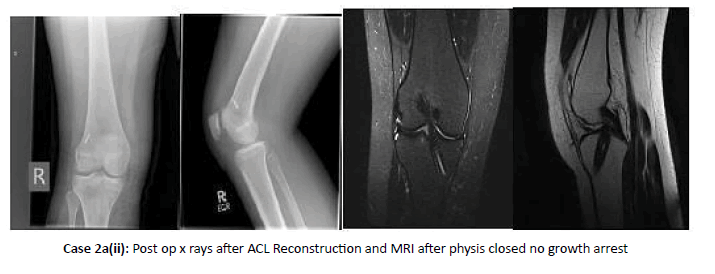
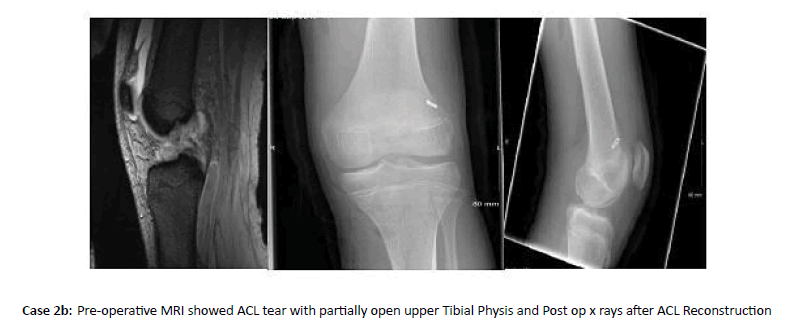
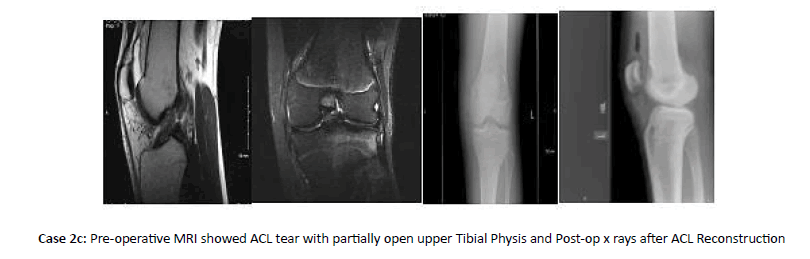
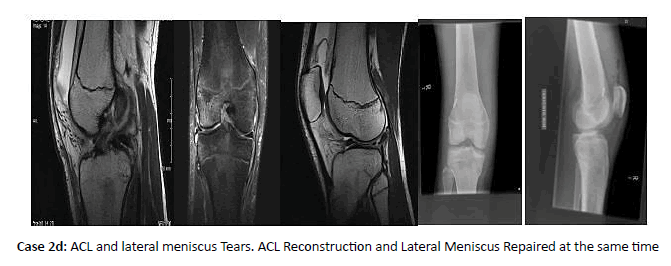
Case 2: ACL injury with open physis
ACL injury with open physis is shown in Case 2a, 2b, 2c and 2d
Note: The treatment of ACL tears in the paediatric population is challenging and controversial. Younger age Patients group (5-12) with open physis were offered the option of activity modification, functional bracing, rehabilitation, and careful follow-up. Surgery was indicated in skeletally immature patients with a torn ACL and an additional repairable meniscal injury and in patients who failed conservative care. Another option for the completely immature paediatric athlete was a more technically demanding all-epiphyseal procedure using hamstring tendon grafts.
In the mid-age child (skeletal age 12 to 14 in girls and 13 to 16 in boys), physeal-sparing methods may be selected; however, many of these intermediate-maturity patients were safely and more appropriately treated with transphyseal reconstruction using small 7 mm-8 mm centrally placed drill holes and a soft tissue graft, such as the hamstring tendons. Patients and parents were counselled that there remains a small risk of physeal injury and a possibility of additional surgery for angular or growth disturbance. Last, adolescents who are approaching skeletal maturity (skeletal age older than 14 in girls and older than 16 in boys,) were undergone anatomic ACL surgery with tibial and femoral drill holes and hamstring graft with minimal risk of physeal injury.
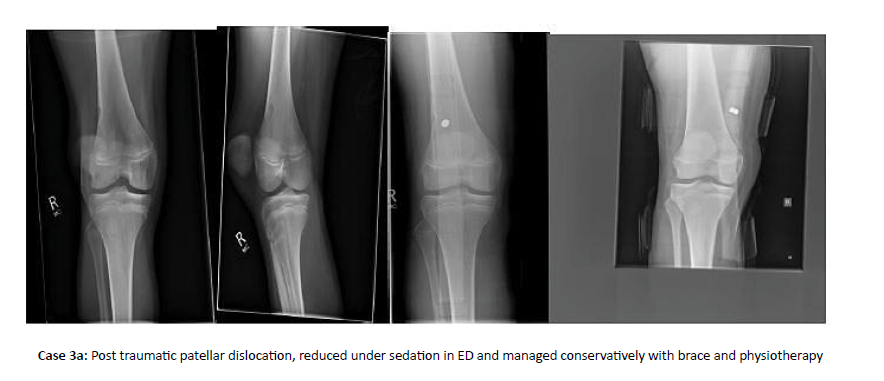
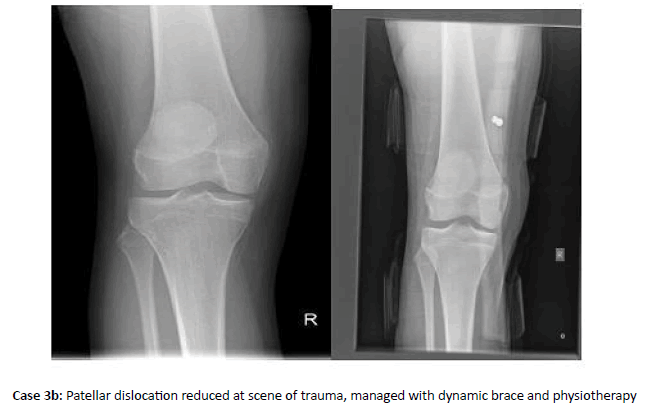
Case 3: Patellar dislocation
Patellar dislocation is shown in Case 3a and 3b
Note: All patients with patellar dislocation who had reduced at the place of injury or manually reduced in ED, were inintially managed in dynamic knee brace and physiotherapy. Most of these patients were improved with conservative treatment. Further scanning was planned who failed conservative management. MRI Knee were arranged to see rupture of medial patellofemoral ligament and ostechondral fracture. Arthroscopic removal of loose body or repair of osteochondral fracture was performed in symptomatic patients. Medial Patellofemoral liagment reconstruction were performed actutely in first time dislocation with large bony fragment and medial patellofemoral reconstruction using hamstring graft in patints having recurrent instability with ligament rupture after making sure that there is no underlying malalignment.
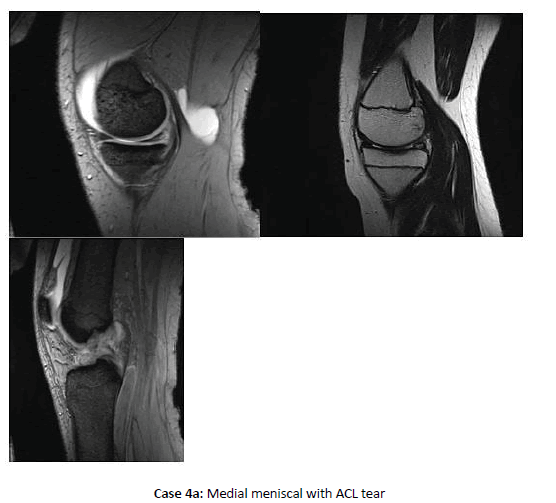
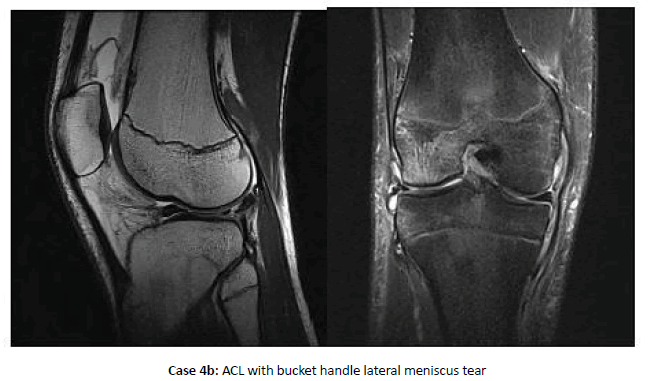
Case 4: Meniscal injuries
Meniscal injuries are shown in Case 4a and 4b.
Note: Meniscal tears in paediatric patients are often associated with other pathology such as ACL tears, tibial eminence fractures or the presence of a discoid meniscus. We repaired all meniscus tears associated with ACL at the time of reconstruction and symptomatic standalone tears in red-red and red-white zones with in-side out technique/all inside using FAST-FIX 360, arthroscopically.
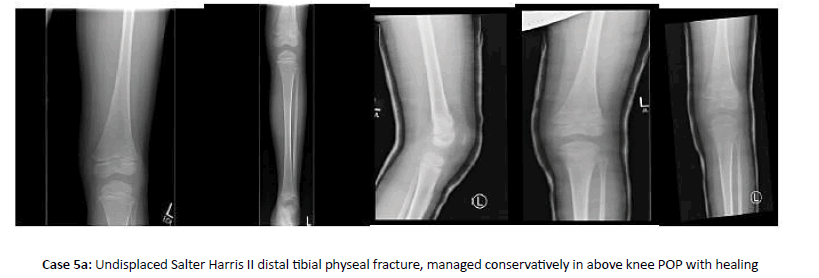
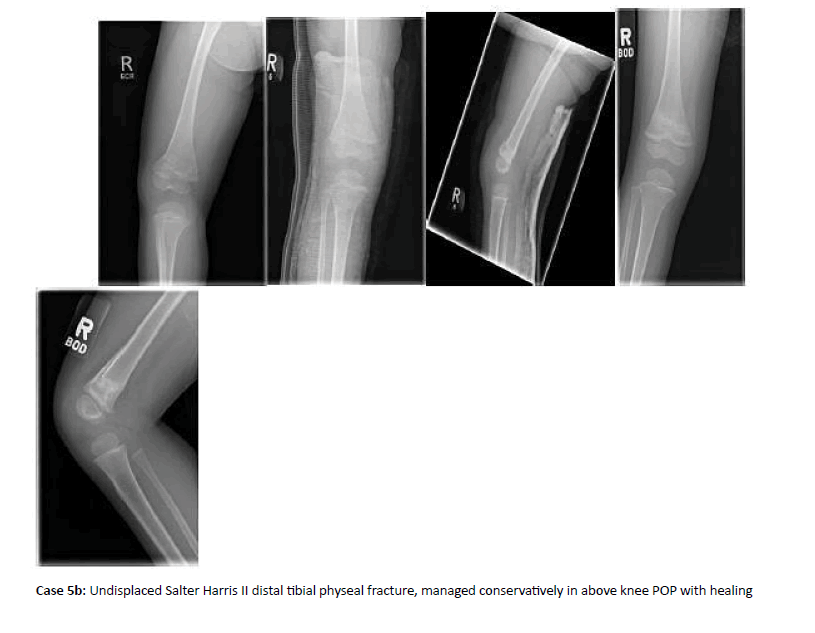
Case 5: Distal femur physeal injuries
Distal femur physeal injuries are explained in Cases 5a and 5b
Note: We managed nondisplaced fractures with long leg casting for 4-6 weeks. Closed reduction and percutaneous fixation followed by casting were applied for displaced Salter-Harris I or II and some Salter-Harris III or IV injuries if anatomic reduction were achieved. Displaced fractures successfully reduced with closed methods were still secured with fixation as fracture pattern are unstable. ORIF with Plate and screws were used for Salter-Harris III and IV with weight-bearing articular involvement.
Irreducible type II fractures were most often due to interposed periosteum on the tension side of fracture.
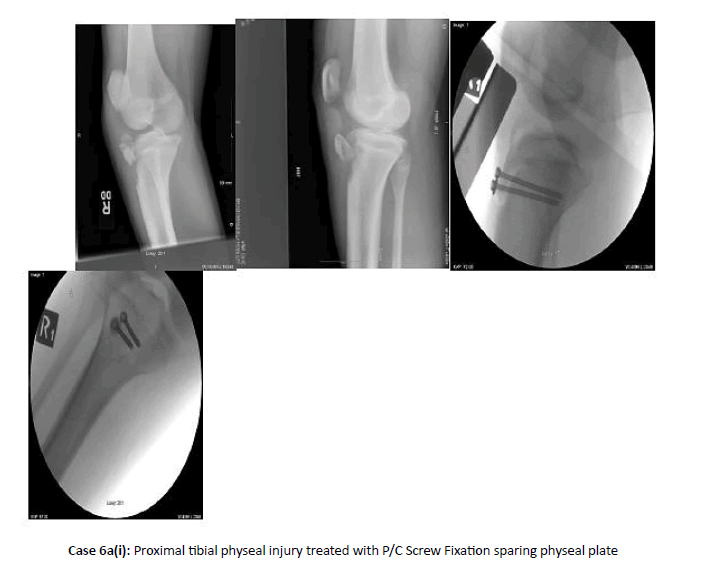
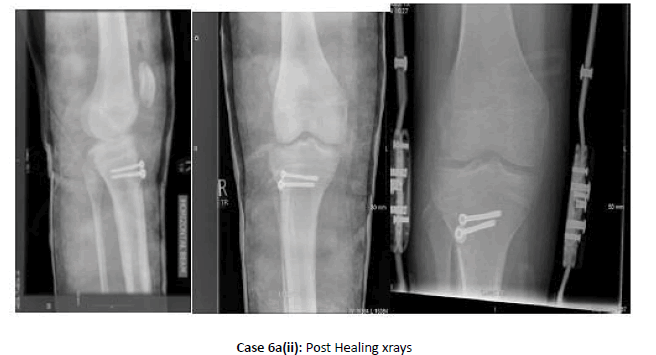
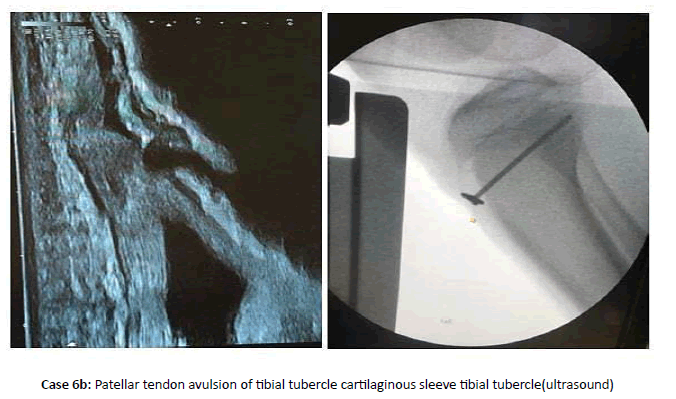
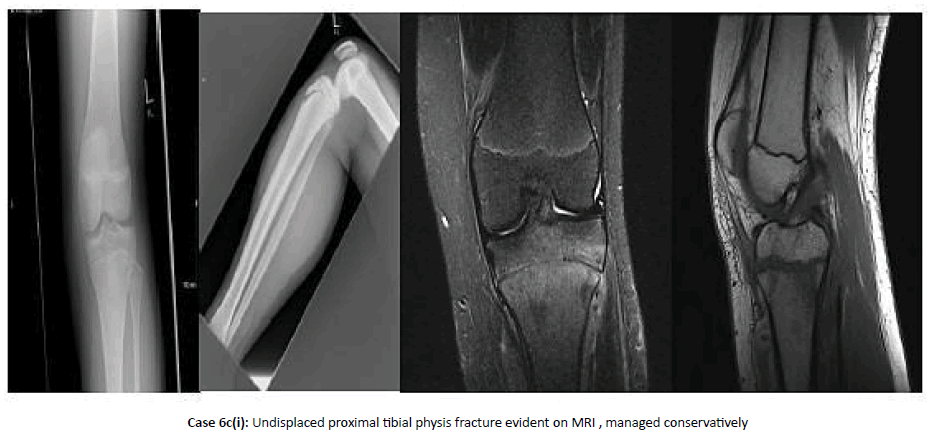
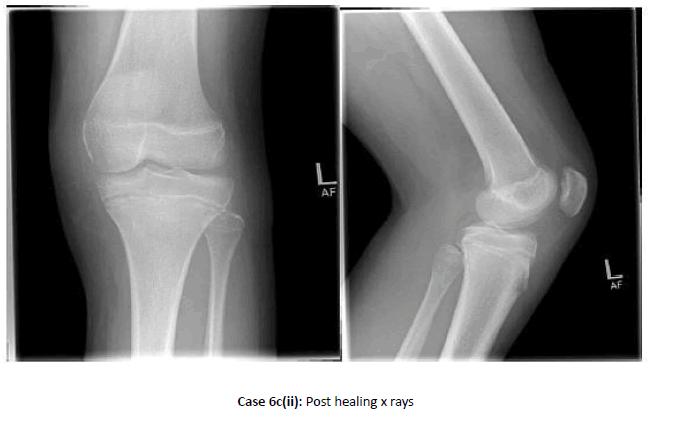
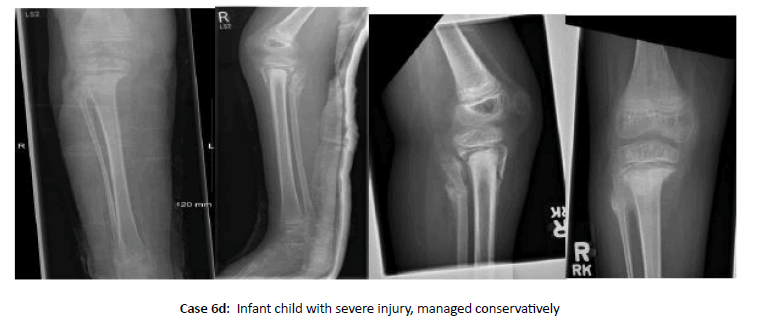
Case 6: Proximal tibial physeal injuries
Proximal tibial physeal injuries are shown in Cases 6a, 6b, 6c and 6d
Note: We had treated undisplaced fracture with long leg cast in extension for 6 weeks and open reduction internal fixation with arthrotomy +/- arthroscopy for Type II-IV fractures - according to Ogden (modification of Watson-Jones) classification.
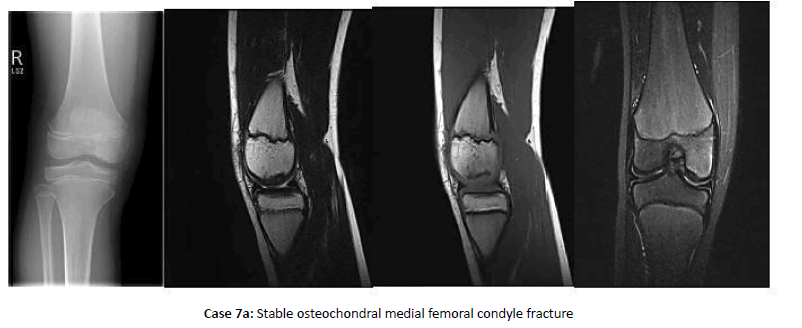
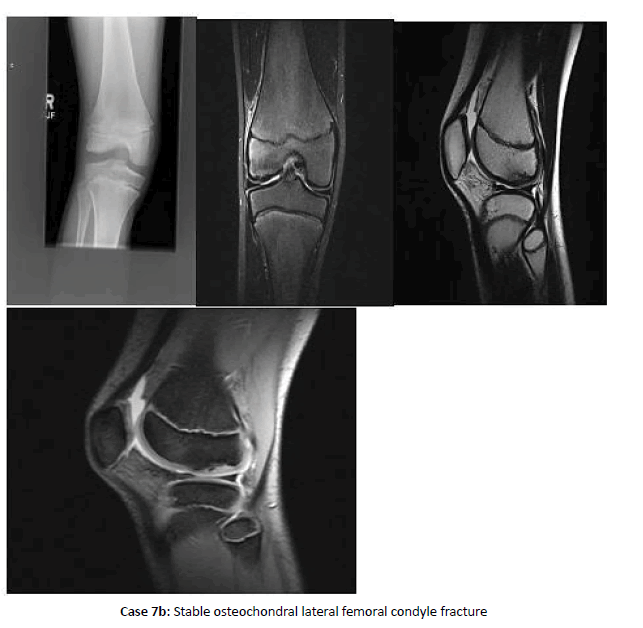
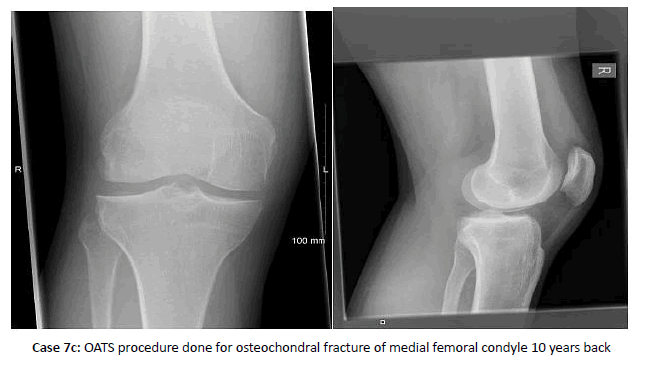
Case 7: Osteochondral femoral condyles injuries
Osteochondral femoral condyles injuries is explained in Case 7a, 7b and 7c
Note: most of undisplaced and small size injuries in younger age group (Category 1 according to Pappa’s classification) were managed conservatively with NWB/TOE touch bearing for 6 weeks and then full ROM and had healed very well due to high healing potential in this age group. Lesions in older age group (category II & III) were managed according to size of lesion and displacement and detachment pattern with arthroscopic removal of detached fragment, retrograde drilling, headless screws fixation, Chondroplasty, Mosaic plasty, OATS and ACI. Cartilage repair and restoration appeared to be fair better when compared to microfracture alone.
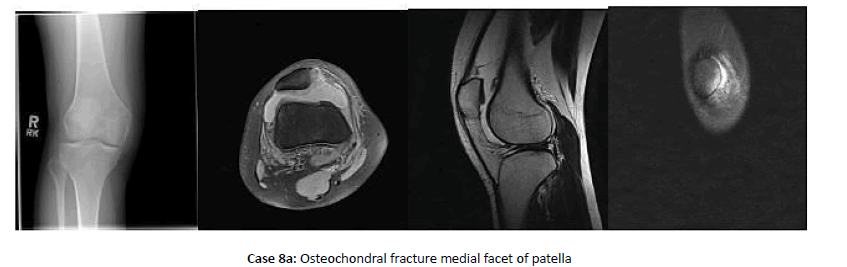
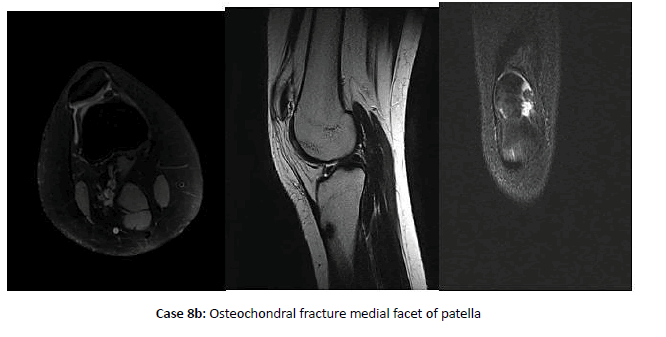
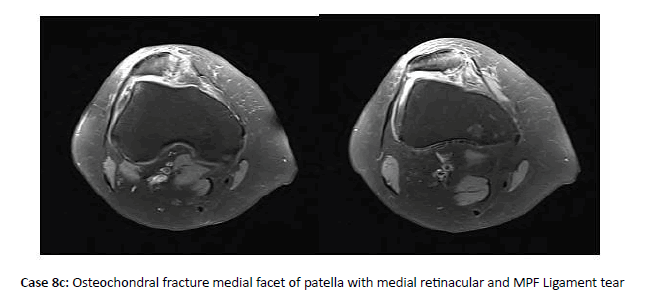
Case 8: Osteochondral patellar injuries
Osteochondral patellar injuries are shown in Case 8a, 8b and 8c
Note: Osteochondral patellar fractures were usually associated with patellar instability and patellar dislocation. Most of these patients were improved with conservative treatment. Further scanning was planned who failed conservative management . MRI Knee were arranged to see rupture of medial patellofemoral ligament and ostechondral fracture. Arthroscopic removal of loose body or repair of osteochondral fracture were performed in symptomatic patients. Medial Patellofemoral liagment reconstruction were performed actutely in first time dislocation with large bony fragment and medial patellofemoral reconstruction using hamstring graft in patints having recurrent instability with ligament rupture after making sure that there is no underlying malalignment.
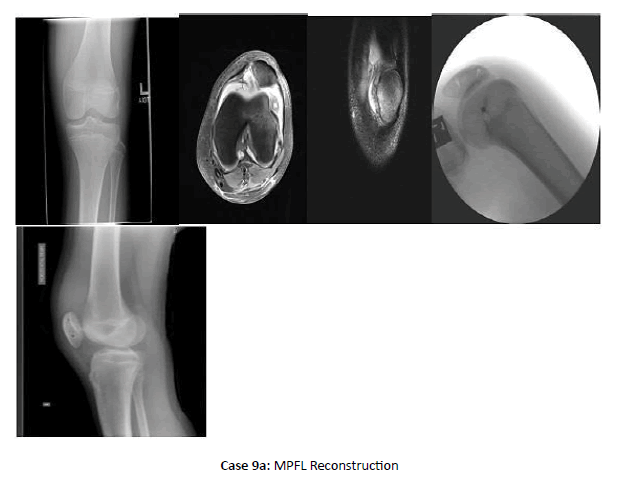
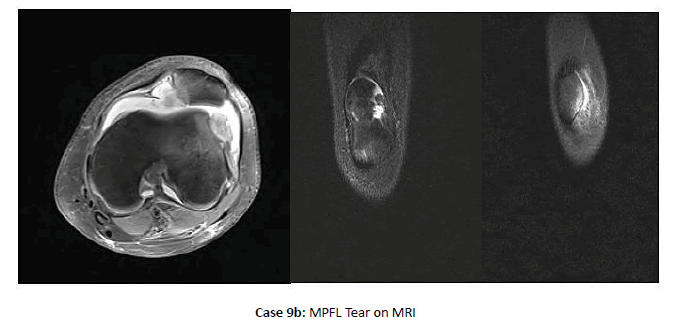
Case 9: Patellofemoral ligamentous injuries
Patellofemoral ligamentous injuries are shown in Case 9a, 9b and 9c
Note: Most of these patients were improved with conservative treatment. Further scanning was planned who failed conservative management. MRI Knee were arranged to see rupture of medial patellofemoral ligament and ostechondral fracture. Arthroscopic removal of loose body or repair of osteochondral fracture were performed in symptomatic patients. Medial Patellofemoral liagment reconstruction were performed actutely in first time dislocation with large bony fragment and medial patellofemoral reconstruction using hamstring graft in patints having recurrent instability with ligament rupture after making sure that there is no underlying malalignment
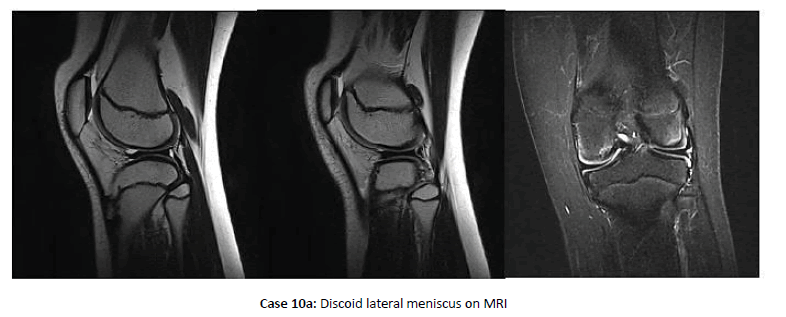
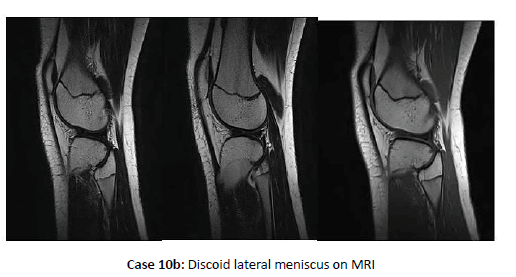
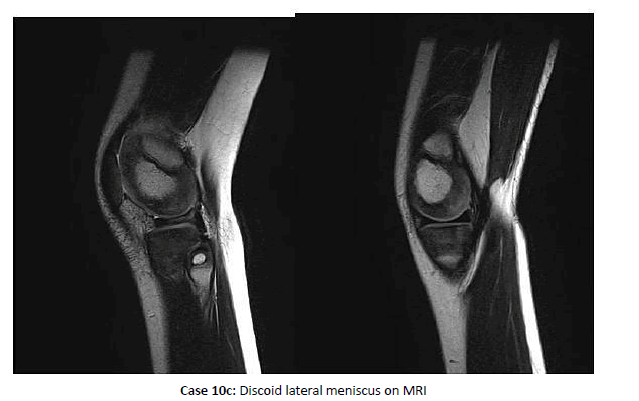
Case 10: Discoid meniscus Injuries
Discoid meniscus Injuries are shown in Case 10a, 10b and 10c.
Note: Most of the discoid Meniscus were managed conservatively who were asymptomatic or having mild symptoms. Arthroscopic saucerization of discoid meniscus or repair of discoid meniscal tear with all inside technique using Fast-Fix 360 suture, respectively.
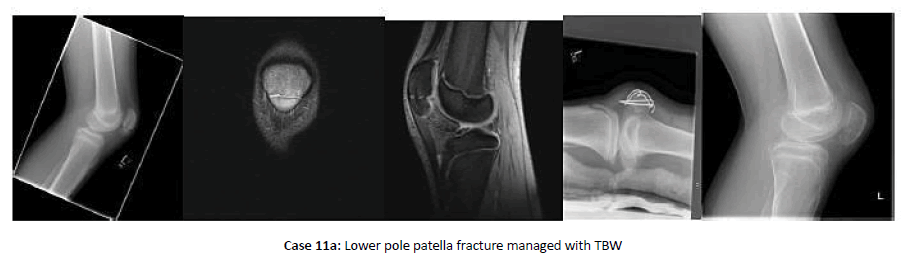
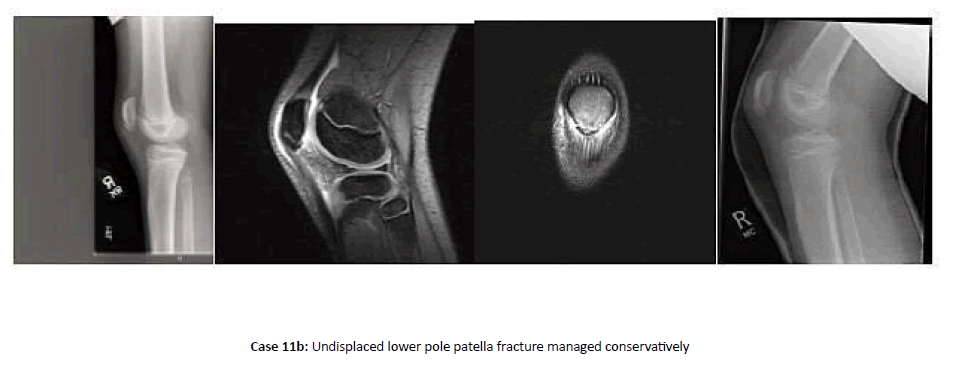
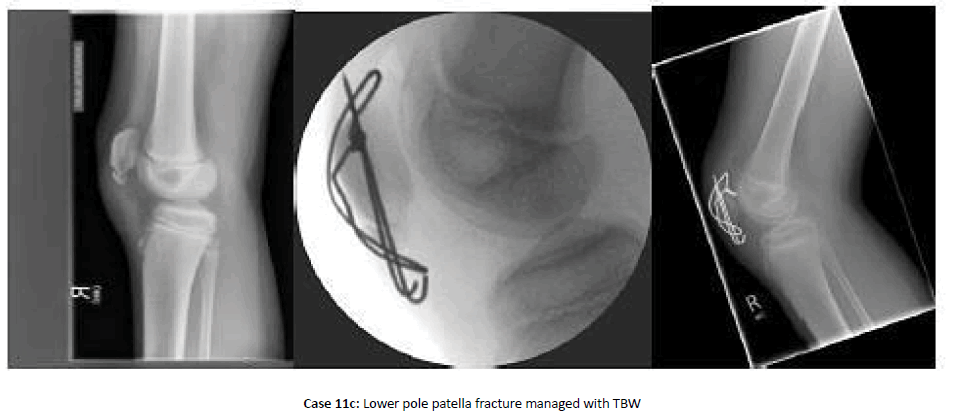
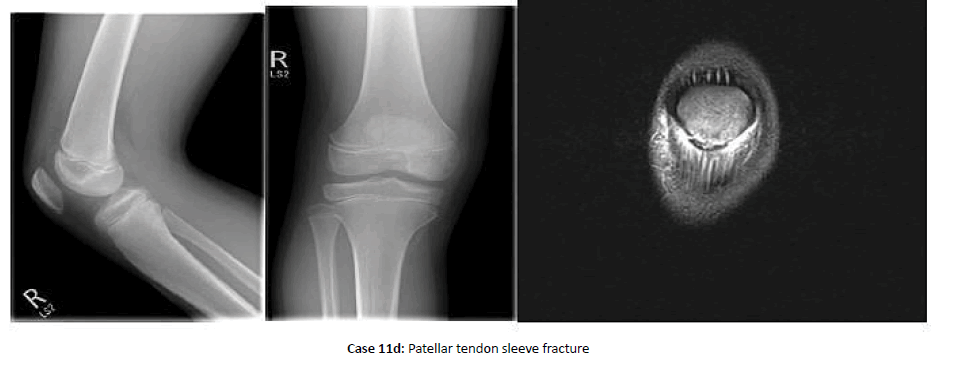
Case 11: Quadriceps and patellar tendons ruptures/Patellar fracture and Patellar sleeve avulsion injuries
Quadriceps and patellar tendons ruptures/Patellar fracture and Patellar sleeve avulsion injuries are shown in Case 11a, 11b, 11c and 11d
Note: These patients were managed with cylinder cast for 6 weeks for nondisplaced fractures with intact extensor mechanism and open reduction and internal fixation with TBW for fractures with 2 mm-3 mm displacement or 2 mm-3 mm articular step-off or disrupted extensor mechanism. We used bony anchors and fibre wire for patellar or quadriceps tendons rupture cases.
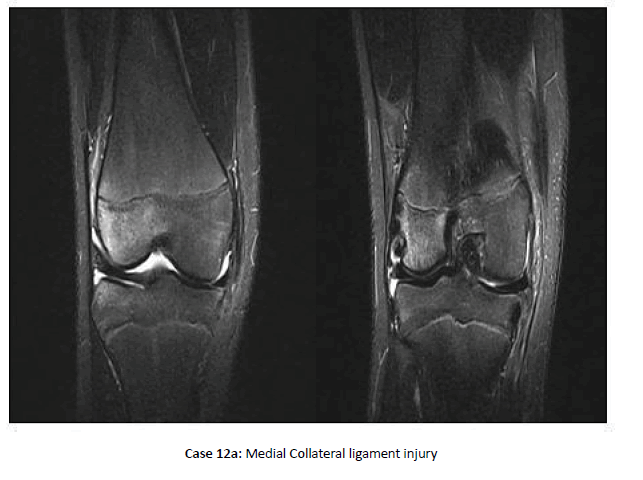
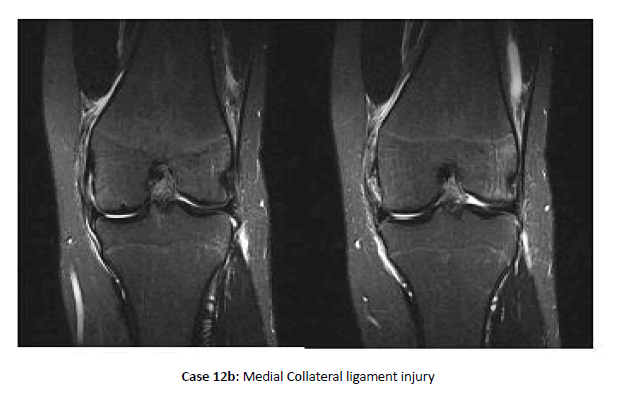
Case 12: Collateral ligaments injuries
Collateral ligaments injuries are shown in Cases 12a and 12b.
Note: Isolated collateral ligament injuries are rare in adolescent athletes. MCL injuries, one-quarter of which occurred in conjunction with patellar instability events, were 4 times more common than LCL injuries, one quarter of which have other posterolateral corner structures involved. Grade III injuries represent 20% to 25% of collateral ligament injuries and occurred most in football and soccer.
Discussion
With the high levels of physical inactivity around the world, increasing physical activity has become a key element of public health promotion [19]. Physical activity provides a great deal of benefits to health and well-being [20,21]. So great in fact that it is promoted as a medicine or a drug against life-style related diseases [22]. Nonetheless, Physical Activity as health promotion tool is not one without adverse effects. Participation in PA is the main cause of adolescent unintentional injuries in many developed countries [23]. Participating in organized sports in adolescence is a major risk factor for hospitalization throughout adolescence and on to early adulthood [24]. However, most injuries can be prevented.
Several studies have already been published describing sports related knee injuries in children. There are few epidemiological studies are present in literature on knee related sports injuries but none of these had addressed the evidence-based management plan. Some focus on professional athletes, others focus on college students or high school students and others on adult athletes [11,25]. Some studies focus only on a specific region of the knee or a specific diagnosis, such as ACL injuries, about more incidence of ACL injuries in female [12], osteochondral (OCD) or Patellar instability [26], and many compare injuries rates between sexes [26,27]. High-level, descriptive outcomes research on a variety of paediatric sports related knee injuries is lacking and this review may help inform topics for future study.
There are only two comprehensive studies as case series of sportsrelated knee injuries in children on PubMed search [25,27]. But both studies detail about epidemiology of these injuries with very limited knowledge of accurate diagnosis and management. This is the first case series study of paediatric knee injuries presented with pictures of sample cases treated and provided some unique information about such fractures’ characteristics and their management.
Brett E. Gage and colleagues [27] had presented an epidemiology of paediatric knee injuries seen in ED and had provided the data about distribution of knee injuries in various seasons, gender, and type of knee injuries. This study has not provided any information about type of management given.
A recent study by Richmond et al. [28] demonstrated that a schoolbased neuromuscular training intervention reduces the risk of PA related injuries while simultaneously improving health markers. Furthermore, several studies have shown that it is possible to prevent adolescent injuries in organized sports by neuromuscular training [17,18,29].
One established risk factor for sports-related injury is a previous sportsrelated injury [30-32]. Therefore, one of the most efficient ways to reduce injury rates is to prevent the first injuries. Injuries can have short- and long-term consequences on adolescent health. In short term, an injury can led to unfavourable weight gain and negative changes on obesity markers [15,33]. In long term, the risk of osteoarthrosis later in life is increased [34,35]. The fear of further injury can limit participation and lead to dropping out of PA. Because of reduced activity, individuals will eventually lose the health benefits produced by PA and this will have negative effects on public health. To achieve best possible results, all PA promotion efforts should include injury prevention into their agenda [36].
Injury prevention programs target movement patterns by incorporating strength, plyometrics and sports-specific agility training [35-37]. Coach and athlete education on cutting/landing techniques (e.g.,wide foot position when cutting, flexed knee when landing) that avoid high-risk knee positions are also fundamental. Injury prevention programs are straightforward to implement because they require little to no equipment and are performed as part of regular team training or physical education 2-3 times per week [38,39].
Conclusion
Knee injuries present one of the highest clinical and public health injuries-related burdens, given the high incidence of knee injuries across the age continuum and the frequent need for surgical repair and long-term rehabilitation. Although a certain endemic level of knee injury in children will always be associated with physical activity, and efforts to increase physical activity levels among the children must continue to be supported, an increased commitment should be made to reduce the number and severity of knee injuries in the children.
High-quality injury prevention programs are the first-line defence against the potential negative short- and long-term consequences of knee injuries. However, if injury prevention efforts fail, timely and accurate diagnosis is important since diagnosis is the starting point for effective management planning and shared decision-making.
REFERENCES
- Prasad D.S.,Das B.C.:Physical inactivity: a cardiovascular risk factor. Indian J Med Sci.2009;63:33-42.
- Pate R.R., Pratt M.,Blair S.N., et al.: Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA.1995;273:402-7
- Dietz W.H.: Health consequences of obesity in youth: childhood predictors of adult disease.Pediatrics.1998;101:518-25.
- Louw Q.A., Manilall J., Grimmer K.A.: Epidemiology of knee injuries among adolescents: a systematic review. Br J Sports Med.2008;42:2-10.
- Moustaki M., Pitsos N., Dalamaga M., Dessypris N., Petridou E.: Home and leisure activities and childhood knee injuries. Injury.2005;36:644-50.
- Smith A.M., Scott S.G.,Wiese D.M.: The psychological effects of sports injuries. Coping Sports Med.1990;9:352-69.
- Simon T.D., Bublitz C., Hambidge S.J.: Emergency department visits among pediatric patients for sports‐related injury: basic epidemiology and impact of race/ethnicity and insurance status. Pediatr Emerg Care.2006;22:309-15.
- Yang J.,Marshall S.W., Bowling J.M., et al.: Use of discretionary protective equipment and rate of lower extremity injury in high school athletes. Am J Epidemiol.2005;161: 511-9.
- Caine D., Caine C., Maffulli N. Incidence and distribution of pediatric sport‐related injuries. Clin J Sport Med.2006;16:500-13.
- Parkkari J., Pasanen K., Mattila V.M., et al.: The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population‐based cohort study of 46 500 people with a 9 year follow‐up. Br J Sports Med.2008;42:422-6.
- Holzach P., Bruesch M., Matter P.: Epidemiology of internal knee injuries in Alpine skiing] (German). Helv Chir Acta.1994;60:531-7.
- Ingram J.G., Fields S.K., Yard E.E., Comstock R.D.: Epidemiology of knee injuries among boys and girls in US high school athletics. Am J Sports Med.2008;36:1116-22.
- Giugliano D.N., Solomon J.L.: ACL tears in female athletes. Phys Med Rehabil Clin N Am.2007;18:417-38.
- Gehring D., Melnyk M., Gollhofer A.: Gender and fatigue have influence on knee joint control strategies during landing. Clin Biomech (Bristol, Avon).2009;24:82-7.
- Baranowski T., Adamo K.B., Hingle M., et al.: Gaming, Adiposity, and Obesogenic Behaviours Among Children. Games Health J.2013;2:119-26.
- Tagesson S., Witvrouw E., Joanna Kvist.: Differences in knee joint stabilization between children and adults and between the sexes. Am J Sports Med.2013;41:678-83.
- Hägglund M., Atroshi I., Wagner P., et al.: Superior compliance with a neuromuscular training programme is associated with fewer ACL injuries and fewer acute knee injuries in female adolescent football players: secondary analysis of an RCT. Br J Sports Med.2013;47:974-9.
- Rössler R., Donath L., Verhagen E.A., et al.: Exercise-based injury prevention in child and adolescent sport: a systematic review and meta-analysis. Sport Med.2014;44:1733-48.
- Lee I.M., Shiroma E.J., Lobelo F, et al.: Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet.2012;380:219-29.
- Biddle S.J.H., Asare M.: Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med.2011;45:886-95.
- Hallal P.C., Victora C.G.,Azevedo M.R., et al.: Adolescent physical activity and health: a systematic review. Sport Med.2006;36:1019-30.
- Janssen I., LeBlanc A.G.: Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act.2010;7:40.
- Verhagen E., Bolling C., Finch C.F.: Caution this drug may cause serious harm! Why we must report adverse effects of physical activity promotion. Br J Sports Med.2014:2014-6.
- Finch C.F., Mitchell R., Boufous S.: Trends in hospitalised sport/leisure injuries in new South Wales, Australia - implications for the targetting of population-focussed preventive sports medicine efforts. J Sci Med Sport.2011;14:15-21.
- Kraus T., Svehlík M., Singer G., et al.: The epidemiology of knee injuries in children and adolescents. Arch Orthop Trauma Surg.2012;132:773-9.
- Cruz AI Jr, Richmond CG, Tompkins MA, Heyer A, Shea KG, Beck JJ. What's New in Pediatric Sports Conditions of the Knee? J Pediatr Orthop.2018;38:66-72.
- Gage B.E., Natalie McIlvain N.M., Collins C.L., et al.: Epidemiology of 6.6 million Knee Injuries Presenting to United States Emergency Departments From 1999 Through 2008 ACAD EMERG MED. 2012;19:378-85.
- Richmond S.A., Kang J., Doyle-Baker P.K., et al.: A school-based injury prevention program to reduce sport injury risk and improve health outcomes in youth: a pilot cluster-randomized controlled trial. Clin J SportMed.2016;26:291-8.
- Soligard T., Myklebust G., Steffen K., et al.: Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. Br Med J.2008;337:a2469.
- Jespersen E., Rexen C.T., Franz C., et al.:Musculoskeletal extremity injuries in a cohort of schoolchildren aged 6-12: a 2.5-year prospective study. Scand J Med Sci Sport. 2015;25:251-8.
- Räisänen A.M., Parkkari J.,Karhola L., et al. Adolescent physical activity-related injuries in sports club, school sports and other leisure time physical activities. Cogent Med.2016; 3:1260-786.
- Kucera K.L., Marshall S.W., Kirkendall D.T., et al.: Injury history as a risk factor for incident injury in youth soccer. Br J Sports Med.2005;39:462-6.
- Myer GD, Faigenbaum AD, Foss KB, et al. Injury initiates unfavourable weight gain and obesity markers in youth. Br J Sports Med.2014; 48:1477-81.
- Whittaker J.L., Woodhouse L.J., Nettel-Aguirre A., et al.: Outcomes associated with early post-traumatic osteoarthritis and other negative health consequences 3-10 years following knee joint injury in youth sport. Osteoarthr Cartil.2015;23:1122-9.
- Lohmander L.S., Englund P.M., Dahl L.L., et al.: The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J SportsMed.2007;35:1756-69.
- Bloemers F., Collard D.C.M., Paw M.C.A., et al.: Physical inactivity is a risk factor for physical activity-related injuries in children. Br J Sports Med.2012;46:669-74.
- Rossler R., Donath L., Bizzini M., Faude.: A new injury prevention programme for children’s football-FIFA 11+ Kids-can improve motor performance: a cluster-randomised controlled trial. J Sports Sci.2016;34:549-56.
- Thorborg K., Krommes K.K., Esteve E., et al.: Effect of specific exercise-based football injury prevention programmes on the overall injury rate in football: a systematic review and meta-analysis of the FIFA 11 and 11+ programmes. Br J Sports Med.2017;51:562-71.
- Attwood M.J.,Roberts S.P., Trewartha G., wt al.: Efficacy of a movement control injury prevention programme in adult men’s community rugby union: a cluster randomised controlled trial. Br J Sports Med. 2018;52:368-374.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.