Management and outcome of infectious spondylodiscitis in patients with and without neurological deficit: A prospective study
2 Professor, Department of Orthopaedics, Rajshree Medical and Research Institute, Bareilly, India
3 Associate Professor, Department of Orthopaedics, Rajshree Medical and Research Institute, Bareilly, India
Received: 11-Jan-2023, Manuscript No. jotsrr-23- 86979; Editor assigned: 12-Jan-2023, Pre QC No. jotsrr-23- 86979(PQ); Accepted Date: Jan 28, 2023 ; Reviewed: 20-Jan-2023 QC No. jotsrr-23- 86979(Q); Revised: 27-Jan-2023, Manuscript No. jotsrr-23- 86979(R); Published: 04-Feb-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: The term Infectious Spondylodiscitis involves infection of the vertebra and infection of the intervertebral disc, or both. Any delay in its diagnosis or management may cause serious long-term morbidity and mortality. In this study, we report the experiences in our Institution in the management of severe and complicated cases of infectious spondylodiscitis.
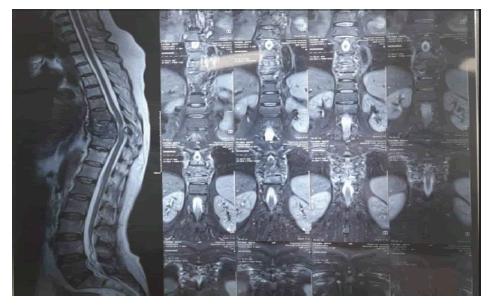
Materials and methods: Over the period of 2 years from 2020- 2022 (covid-19) 40 patients were operated in our medical college. The management was tailored according to the clinical condition based on VAS, ODI, radiological studies and lab results of each case; and patients were then prospectively followed-up for 2 years. Results: The goals of treatment for spondylodiscitis is to relieve pain, restore pain free mobilization of the patient and to eliminate infection. Magnetic Resonance Imaging (MRI) was considered the main choice of investigating tool other assessments were done by ODI, VAS, Neurologic deficits was assessed by Modified McCormick scale, sepsis, an intraspinal empyema, the failure of conservative treatment, and spinal instability are all indications for surgical treatment.
Conclusion: The quality of life of patients who have been appropriately treated for infectious spondylodiscitis has been found to be highly satisfactory in general. The risk of recurrence increases in the presence of accompanying illnesses such as diabetes mellitus, renal failure, which were managed by immediate debridement and results were good which was assessed according to above mentioned post-op ODI and VAS.
Exclusion criteria
Informed consent was obtained from all the participants. Ethical approval for the study was obtained from the Institutional Ethical Committee.
References
- Sobottke R, Seifert H, Fätkenheuer G, et al. Current diagnosis and treatment of spondylodiscitis. Dtsch Ärztebl Int. 2008; 105(10):181. [Google Scholar]
[CrossRef]
- D’agostino C, Scorzolini L, Massetti AP, et al. A seven-year prospective study on spondylodiscitis: epidemiological and microbiological features. Infection. 2010; 38(2):102-7. [Google Scholar]
[CrossRef]
- Akbar M, Lehner B, Doustdar S, et al. Pyogenic spondylodiscitis of the thoracic and lumbar spine: a new classification and guide for surgical decision-making. Der Orthopade. 2011; 40(7):614-23. [Google Scholar]
[CrossRef]
- Bettini N, Girardo M, Dema E, et al. Evaluation of conservative treatment of non specific spondylodiscitis. Eur Spine J. 2009; 18(1):143-50. [Google Scholar]
[CrossRef]
- Vos FJ, Kullberg BJ, Sturm PD, et al. Metastatic infectious disease and clinical outcome in Staphylococcus aureus and Streptococcus species bacteremia. Medicine. 2012; 91(2):86-94. [Google Scholar]
[CrossRef]
- Bettini N, Girardo M, Dema E, et al. Evaluation of conservative treatment of nonspecific spondylodiscitis. Eur Spine J. 2009; 18(1):143-50. [Google Scholar]
[CrossRef]
- Vos FJ, Kullberg BJ, Sturm PD, et al. Metastatic infectious disease and clinical outcome in Staphylococcus aureus and Streptococcus species bacteremia. Medicine. 2012; 91(2):86-94. [Google Scholar]
[CrossRef]
- Homagk L, Marmelstein D, Homagk N, et al. SponDT (Spondylodiscitis Diagnosis and Treatment): spondylodiscitis scoring system. J orthop surg res. 2019; 14(1):1-8. [Google Scholar]
[CrossRef]
- Tsai TT, Yang SC, Niu CC, et al. Early surgery with antibiotics treatment had better clinical outcomes than antibiotics treatment alone in patients with pyogenic spondylodiscitis: a retrospective cohort study. BMC musculoskelet disord. 2017; 18(1):1-7. [Google Scholar]
[CrossRef]
- Stoop N, Zijlstra H, Ponds NH, et al. Long-term quality of life outcome after spondylodiscitis treatment. Spine J. 2021; 21(12):1985-92. [Google Scholar]
[CrossRef]
Conclusion
In our study of 40 patient’s outcome was assessed on the basis of ODI, VAS scores, assessment of neurological status along with sequential changes in TLC and CRP being evaluated at 3 months, 6month, 1 year,and at 2 years. The quality of life of patients who have been appropriately treated for infectious spondylodiscitis has been found to be highly satisfactory in general with p-value of VAS and ODI at the end of 2 years was 0.001(<0.005). The risk of recurrence increases in the presence of accompanying illnesses such as diabetes mellitus, which were managed by immediate re-surgery and results were good. Early surgery was advised to the patients for early mobilization and to reduce the risk of spinal cord injury.
Discussion
The 40 patients included in our study had a mean age of 52.0 years. 22.5% subjects were less than 40 years and 77.5% more than 40 years there were 40.0% males and 60.0% females. In comparison to our study, Homagk the 296 patients included in their study had a mean age of 67.3 years. 66.2% were 60 years to 80 years old and 56.7% were male. Tsai did same as our study including two groups in which group 1 were taken on antibiotic treatment only with 26 patients with mean age of 62 with 68.2% males and 30.8% females and group 2 with 35 patients undergoing surgical and antibiotic treatment with mean age of 58.4 years. with male constituting 74.3% and females 25.7%. Homagk took CRP and TLC as laboratory markers for patient evaluation post-surgery same as in our study. In Homagk study CRP at admission was 119.9 which fell to 43 at the time of discharge at 1 month where as in our study it was measured during presentation with mean CRP levels 25.7 and after 3 months it was significantly reduced with mean of 1.48 with p value of 0.015 as compared to them which was< 0.05. TLC levels in Homagk study during presentation with mean value of 10.6 with p value of<0.05 as compared to our study with mean TLC of 13.4 with p value of 0.027 (p value<0.05) [8]. They generally fell across the course of treatment for spondylodiscitis to the normal value of 9.5 on discharge in Homagk study in our study it was measured after 3 months with mean TLC value of 5.7 with p value of 0.027(p value<0.05). Tsai et al measured performance outcome of surgically treated patients with VAS and ODI same as in our study with mean value of 1.4 and 8.8 with p value of 0.034 and 0.048 respectively [9]. Stoop et al. measured VAS and ODI The mean VAS for back pain was 3.5, and the mean ODI score was 22 (p value o.81) [10]. In our study it was followed up regularly at 3 months,6 months, 12 months, and 24 months with mean of 1 and 5 with p value of 0.000 (p value<0.05).
Limitations
1. Short sample size.
2. Single centre study.
3. Short duration of follow up
Complications
Out of 40 patients, 11 patients in our study required re-exploration of surgical wound with debridement which was decided on the basis of persistent fever, continuous and copious discharge from surgical site corroborated by excessive drain output and continuous elevation of inflammatory markers visa vis CRP [9,10]. All above mentioned patients which were re-explored had multiple co-morbidities namely Diabetes Mellitus, Chronic Renal Failure, COPD, Hypertension. The post-operative ODI and VAS scores of these 11 patients had significant improvement after 2nd surgical intervention.
Results
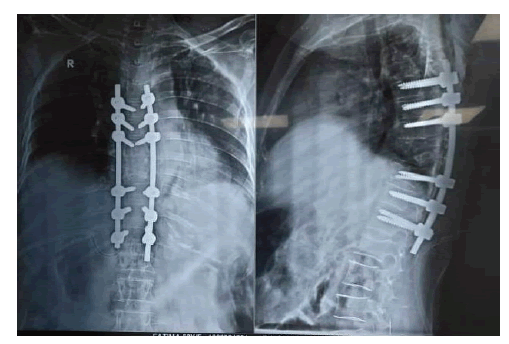
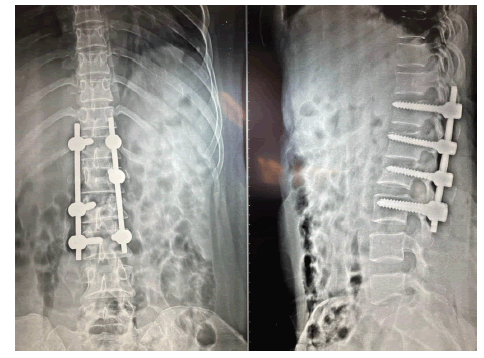
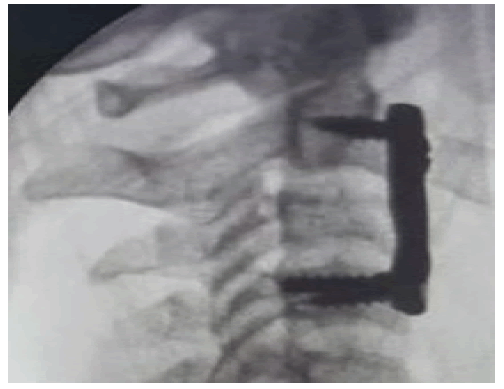
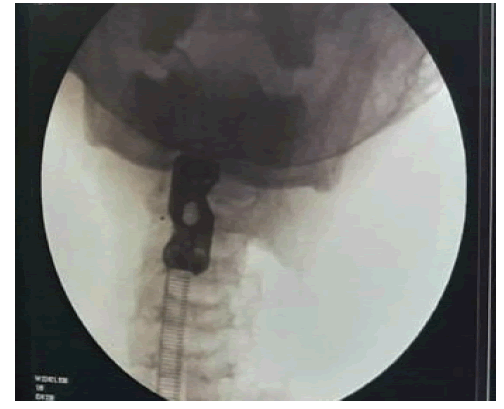
In this study we took 40 patients in which 24 female patients, 16 male patients. The study population accounted to 40 patients, of which 9 patients were 17 years-40 years and 31 patients were greater than 40 years. 22.5% were 17 years-40 years, 77.5% was more than 40 years (Table 1). The mean of total leucocyte count was 13440.0. And after 3 months of treatment, it had decreased significantly (Table 2). The mean of CRP was 25.53 which was also significant decreased (Table 3). We used different scoring systems to know outcome. The mean ODI was compared using the repeated measures ANOVA test using the post-hoc Bonferroni test. The mean ODI decreased significantly from during presentation to 3 months to 6 months and 12 months to 24 months respectively. The mean ODI during presentation was 45.98 with standard deviation of 2.03. Mean ODI at 3 months, 6 months, 12 months, 24 months was 5.0, 4.0, 4.0, 3.0 respectively with p value<0.001 (Table 4). the mean VAS score was compared using the repeated measures ANOVA test using the post-hoc Bonferroni test. The mean VAS score decreased significantly from during presentation to 3 months, 6 months, 12 months and 24 months respectively. The mean vas during presentation was 8.29 with S.D of .61. The mean VAS at 3 months, 6 months, 12 months, 24 months was 1 with p value<0.001 (Table 5). Out of 40 patients 5% cervical spine cases were managed surgically by anterior cervical approach in one of our cervical patients there was C2 instability with extensive retropharyngeal abscess extending from clivus to D2 vertebrae which was managed by anterior cervical plate. Other patient had C3 instability which was a known case of ankylosing spondylitis with Anderson’s lesion extending from posterior to anterior column of C3, with L4-L5 spondylodiscitis (Table 6 and 7). 27.5% dorsal spine were operated by posterior fixation and decompression. Out of which 54.5% were double level, 18.18% single level, 18% with thoracic epidural abscess and multiple levels were involved in one of our patient with potts spine (C7-L1) which was operated in our institution with posterior fixation and decompression extending at 13 vertebrae levels. 7.5% cases were of D-L junction with multiple levels which were managed by posterior fixation and decompression. 60% cases were of lumbar spine. 62.5% cases involving single level 33% cases involving double level and 4% cases involving multiple levels which were managed by posterior pedical screw fixation with posterior decompression. Results of patients operated by our surgeon are promising 95% of cases operated in our institution had improvement in their post op check-up.
Table 1. Distribution of study population according to age in years
| Age in years | Frequency | Percent |
|---|---|---|
| 17years - 40 years | 9 | 22.50% |
| > 40 years | 31 | 77.50% |
Table 2. Distribution of study population according to TLC
| TLC (cells/ cumm) | Mean | Std. Deviation | Minimum | Maximum | p-value |
|---|---|---|---|---|---|
| Baseline | 13440 | 4197.91 | 10200 | 30000 | 0.027* |
| At 3 months | 5675 | 972.37 | 4500 | 8500 |
Table 3. Distribution of study population according to CRP
| CRP | Mean | Std. Deviation | Minimum | Maximum | p-value |
|---|---|---|---|---|---|
| Baseline | 25.53 | 7.11 | 12 | 45 | 0.015* |
| At 3 months | 1.48 | 0.92 | 0.3 | 4 |
Table 4. Distribution of study population according to ODI
| ODI | Mean | Std. Deviation | p-value | post-hoc comparisons |
|---|---|---|---|---|
| During presentation | 45.98 | 2.03 | 0.001 | During presentation > 3 months > 6 and 12 months > 24 months |
| 3 months | 5 | 0.55 | ||
| 6 months | 4 | 0 | ||
| 12 months | 4 | 0 | ||
| 24 months | 3 | 0 |
Table 5. Distribution of study population according to VAS.
| VAS score | Mean | Std. Deviation | p-value | post-hoc comparisons |
|---|---|---|---|---|
| During presentation | 8.29 | 0.61 | 0.001 | During presentation > 3, 6, 12 & 24 months |
| 3 months | 1 | 0 | ||
| 6 months | 1 | 0 | ||
| 12 months | 1 | 0 | ||
| 24 months | 1 | 0 |
Table 6. Distribution of study population according to sex
| Frequency | Percent | |
|---|---|---|
| Female | 24 | 60.00% |
| Male | 16 | 40.00% |
Table 7. Modified McCormick grade improved significantly postoperatively
| Modified McCormik scale | Pre-operative | Post-operative | ||
|---|---|---|---|---|
| N | % | N | % | |
| Grade I | 0 | 0.00% | 36 | 97.3% |
| Grade II | 0 | 0.00% | 1 | 2.70% |
| Grade III | 6 | 16.20% | 0 | 0.00% |
| Grade IV | 26 | 70.30% | 0 | 0.00% |
| Grade V | 5 | 13.50% | 0 | 0.00% |
| p-value | 0.001* | |||
22.5% subjects were less than 40 years and 77.5% more than 40 years.
The mean TLC (cells/cumm) decreased significantly from baseline to 3 months.
The mean CRP decreased significantly from baseline to 3 months.
The mean ODI was compared using the repeated measures ANOVA test using the post-hoc Bonferroni test. The mean ODI decreased significantly from during presentation to 3 months to 6 months and 12 months to 24 months with p-value 0.000 (p-value<0.05).
The mean VAS score was compared using the repeated measures ANOVA test using the post-hoc bonferroni test. The mean VAS score decreased significantly from During presentation to 3 months to 6 months and 12 months to 24 months with p-value 0.000 (p-value<0.05) [7-8].
There were 40.0% males and 60.0% females
Postoperative Evaluation
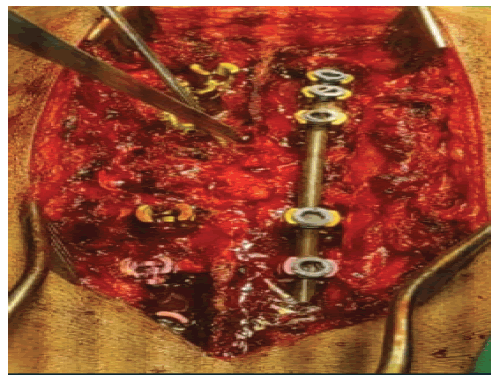
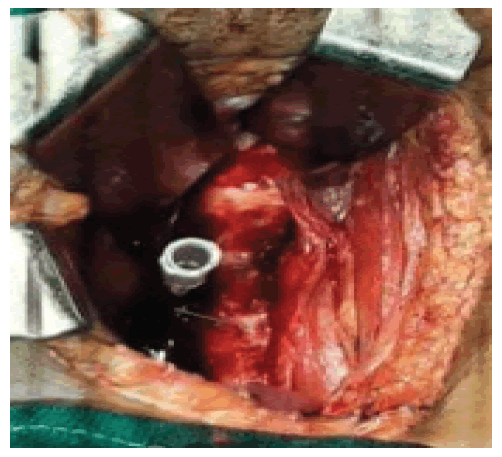
Postoperatively neurological status was assessed immediately after surgery. TLC, CRP were main blood markers used for post-operative status of infection. Broad spectrum antibiotics were used including vancomycin 1 gm for 2 weeks, linezolid 600 mg, levofloxacin 750 mg for 2 weeks-4 weeks. Antibiotics were taken on oral Tablets with pain medication tab. Pcm 500 TDS was given post operatively. Postop drain was used which was measured 24 hourly and was removed accordingly ion post -op day 5th, 6th, 7th, 8th, 9th day. Sitting and standing was allowed on post-op day 0 and walking was started from post-op day 1 with help of walker and taylor’s brace as according to patients need along with multivitamins, vit d3, physiotherapy. Complete regression of infection was based on radiological, clinical and lab investigations. Pain assessments were assessed at 3 months, 6 months, 12 months and 24 months respectively along with neurological status. In all cases instrumented fixation with pedical screws, rods, spinal cages, bone grafts were used according to patients need as per Fig. 1-8. MRI was done at 9 months or according to patient’s neurological status. X-rays were done every month.
Surgical Technique
Posterior approach for spine was used for dorsal, lumbar and sacral segments, anterior cervical approach was used in cervical spondylodiscitis. Posterior approach was used for dorsal, lumbar and sacral spine. Posterior decompression and fixation was done as needed according to patient assessments.
Statistical Analysis
The results are presented in frequencies, percentages and mean and SD. Chi-square test and ANOVA test were used for comparisons. The p-value<0.05 was considered significant. All the analysis was carried out on SPSS 24.0version (Chicago, Inc, USA)
Keywords
Visual Analogue Scale (VAS), Oswestry Disability Index (ODI)
Inclusion Criteria
All patients with spinal instability, neurological deficit, spinal cord compression, cord myelopathy was included.
Materials and Methods
40 patients who were operated here between 2020-2022(including covid-19) were included in our study which were operated by a single surgeon. Patient evaluation was done accordingly based on clinical presentation, neurological status, radiological studies and laboratory analysis. X-rays, MRI were main radiological tools prior and postsurgery. Pre-op and post-op assessment scores was based on ODI and VAS and modified McCormick scale.
Sample Size
To calculate the sample size based on the prevalence with an approximate 95% confidence level, following formula will be used,
Sample Size (n)=Z2 x P(100-P)
Z=1.96 at 95% confidence interval
P=Prevalence
Q=100-P r=Absolute error=10%
Study design
Prospective study
Study population
Patients operated between 2020-2022 (including covid-19) with and without neurological deficits.
STUDY SITE
Department of Orthopaedics, Rajshree Medical Research Institute, Bareilley.
Aim and Objectives
To evaluate the outcome and result of patients operated in our institution for the management of complicated spondylodiscitis.
To evaluate the improvement in neurological status of patients operated on the basis of:
1. Severity of pain–Visual Analogue Scale (VAS).
2. Disability score– Oswestry Disability Index (ODI).
3. Time taken to resume work (in days).
4. Modified McCormick scale for neurological deficit
Introduction
Spondylodiscitis is an infectious inflammation that affects the vertebrae, vertebral discs and adjacent structures. It may have a bacterial and a relatively broad spectrum of pathogens is considered to induce spondylodiscitis; the largest proportion of spondylodiscitis cases are caused by Staphylococcus aureus [1–3]. The incidence of spondylodiscitis is on average seven per million, with men three times more frequently affected than women. Although spondylodiscitis is a rare disease, the widespread use of drugs that suppress the immune system and an ageing population have led to an increase in the number of cases [3, 4]. Though the disease is most often seen in the sixth decade of life, it may occur at any age. In addition to age, risk factors include diabetes mellitus, malnutrition, steroid therapy, rheumatic diseases and spinal surgery. Surgical management was advised according to the presenting factors of the patients including pain, neurological deficit, sepsis, compressive myelopathy, spinal cord compression, spinal instability [5-7].
The aims of this study were to report our institution experience in the management of patients with severe and complicated SD, to provide analysis of the patients in this series, comparing several aspects in the multiple management plans we provided; and interpreting their postoperative recovery course as well as outcome results, to identify points of strengths and weaknesses of current management strategies, while give final recommendations accordingly, to improve the quality of care given to patients with challenging SD. In our study of 40 patient outcome was assessed on the basis of postoperative VAS scores and ODI all sequential changes in TLC and CRP along with assessment of neurological status being evaluated at 3 month, 6 month, 1 year, and at 2 years.




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.