Functional outcomes after anterior cruciate ligament reconstruction procedure: a retrospective, observational study
2 Chief Medical Officer, Healthium Medtech Limited, Ambedkar Colony, Yelahanka, Bengaluru, Karnataka, India
3 Deputy General Manager – Clinical Affairs, Healthium Medtech Limited, Ambedkar Colony, Yelahanka, Bengaluru, Karnataka, India
Received: 04-Apr-2023, Manuscript No. jotsrr-23-94254; Editor assigned: 05-Apr-2023, Pre QC No. jotsrr-23-94254 (PQ); Accepted Date: Apr 20, 2023 ; Reviewed: 15-Apr-2023 QC No. jotsrr-23-94254 (Q); Revised: 18-Apr-2023, Manuscript No. jotsrr-23-94254 (R); Published: 23-Apr-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: The aim of the present study was to evaluate the functional outcomes of arthroscopic Anterior Cruciate Ligament (ACL) reconstruction using Sironix knee devices.
Methods: All the subjects were consented telephonically for the study purpose. Demographic data, surgery details and other baseline characteristics of the subjects who underwent ACL reconstruction surgery between January 2019 to July 2022 were collected from the medical records. Primary objective of the study was to assess the functional outcomes using International Knee Documentation Committee (IKDC) and Modified Cincinnati Rating System (MCRS) questionnaires. Secondary objectives were to assess the pre- and post-surgery activity levels using Tegner Activity Score (TAS) and quality of life evaluation using Quality of Life (QoL) subscale from Knee Injury and Osteoarthritis Outcome Score (KOOS) score. ACL reconstruction failure rate, adverse device effects and surgery-related adverse events information was collected.
Results: A total of 44 subjects completed the study. The mean (SD) age was 34.5 (±11.4) years. Mean (SD) total duration of follow-up was 16 (±7) months. Out of 44 subjects, 35 (79.5%) did not have any comorbid conditions. Mean (SD) of total IKDC score of all enrolled subjects was 85.9 (±7.5) out of 100 and mean (SD) of MCRS questionnaire was 94.5 (± 6.8) out of 100. Mean (SD) of TAS before injury was 7.9 (±0.9) and current status was 5.2 (±1.04) out of 10. Mean (SD) values of quality of life subscale of KOOS score was 88.5 (± 9.2) out of 100. There were no reconstruction failures and adverse device effects reported in this study.
Conclusion: Considering remarkable results in all the functional assessment scores and no incidence of reconstruction failures, this study concludes that ACL reconstruction surgery using Sironix knee devices as safe and effective method.
Keywords
Anterior cruciate ligament, international knee documentation committee, modified cincinnati rating system, functional outcomes
Introduction
ACL is an important stabilizing ligament of the knee that is frequently injured by athletes and trauma victims [1]. In India, the ACL incidence of overall age groups is 68.6 per 1,00,000 person-years, as per a 2014 study [2]. 86.5% of knee injuries in India were related to sports [3]. Other than sports injuries, a study conducted in a rural tertiary care hospital claimed that road traffic accidents as the biggest culprit for ACL injuries [4].
Anterior Cruciate Ligament (ACL) is one of the four major ligaments of the knee joint [5]. The ACL is divided into two functional bundles, the anteromedial and posterolateral bundles, which work together to optimize its restraining function throughout the range of knee motion [6]. ACL is a very important ligament for maintaining the stability of the knee joint. ACL complete tear can lead to a highly unstable knee joint, incapacitating the patient [7].
The principal goal with every ACL reconstruction is to provide a stable initial graft fixation to allow tendon-to bone healing and incorporation within the tibial and femoral tunnels. The modern era of arthroscopy assisted ACL reconstruction has seen the emergence of several graft fixation techniques and devices available to the orthopaedic surgeon [8]. ACL fixation devices must provide strength and stiffness sufficient for rehabilitation and activities of daily living until biologic fixation has taken place. The surgeon must outweigh the pros and cons of the different ACL graft fixation devices before deciding which device to use for a particular patient [9].
Different types of ACL graft fixation techniques used are interference screws, suspensory fixation loops and cortical buttons. On the femoral side, a method is used in which sutures forming an anchor and a loop are integrated. Two types of devices are used here, an Adjustable-Loop Device (ALD) and a Fixed-Loop Device (FLD), by which the loop length can and cannot be adjusted, respectively, after the anchor has been flipped [10]. Interference screw fixation remains an effective technique in Bone- Patellar Tendon-Bone (BPTB) ACL reconstruction [11]. When a tendon is fixed to the femoral side, the use of interference screws has been shown to be highly successful and reproducible technique with excellent long-term outcomes [12]. At present, titanium is the most common material used for this class of devices. Titanium screws provide high initial fixation strength and promote early integration into the bone [13]. Anterior Cruciate Ligament (ACL) injuries are also associated with meniscal lesions and frequently involve the posterior horn of the lateral meniscus [14]. During ACL reconstruction, tears of the lateral meniscus posterior root are found in up to 14% of the patients [15].
However, there’s a dearth of data on functional outcomes after ACL reconstruction in Indian population. Therefore, the hypothesis of this study was to assess the functional outcomes using standardized questionnaires from the present real-world data after ACL reconstruction surgery.
DEVICE DESCRIPTION
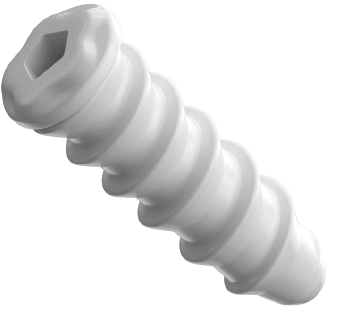
Helysis®PLDLA-BTCP Interference screw: These screws are made up of PLDLA-BTCP material [poly (L-co-DL lactic acid) and Beta Tricalcium phosphate]. The screws are intended for fixation of soft tissue to bone (Fig.1).
Helysis® Titanium Interference screw: These are made up of titanium material. Titanium is considered as the most biocompatible metal due to its resistance to corrosion from bodily fluids, bio-inertness, capacity for osseointegration and high fatigue limit. The screws are intended for fixation of soft tissue to bone (Fig. 2)
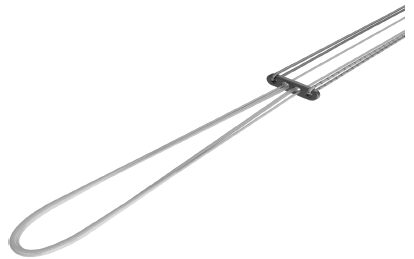
Proloop™- Adjustable Loop UHMWPE suture titanium button: This device consists of titanium button and Ultra-High Molecular Weight Polyethylene (UHMWPE) suture adjustable loop. It is intended for fixation of soft tissue to bone (Fig. 3).
Surestitch™ All Inside Meniscal Repair Implant: This consists of two PEEK non-absorbable implants, pre-tied with USP #2-0 Nonabsorbable UHMWPE suture and preloaded into a needle delivery system (Fig. 4).
Materials and Methods
STUDY DESIGN
This was a retrospective study to assess the functional outcomes after arthroscopic ACL reconstruction procedure using Sironix knee devices. All the enrolled subjects were consented before the telephonic interview for the study purpose. Data of subjects who underwent ACL reconstruction surgery between January 2019 to July 2022 was taken into consideration. Demographic details, medical/surgical history details, and ACL reconstruction surgery details were collected from the subject medical records. Primary outcome of this study was to assess the functional outcomes using IKDC and MCRS questionnaires. Secondary outcomes include TAS questionnaire to evaluate pre- and post-surgery activity level and quality of life subscale of KOOS questionnaire to assess the quality-of-life post-surgery and assessment of ACL reconstruction failure rate. Adverse device effects and surgery-related adverse events information was gathered telephonically along with medication details.
This clinical investigation was conducted in compliance with the ICH GCP E6 R2 2016 (Step 4), Guidance for Good Clinical Practices (GCP), New Drugs and Clinical Trials 2019, Medical Devices Rules (MDR- 17 & Amendment Rules, 2020), Declaration of Helsinki (Taipei 2016) and ISO 14155-2020. The CTRI registration number for this study is CTRI/2022/11/047428.
Male/female subjects aged ≥ 18 years and ≤ 60 years at the time of surgery, subjects who had undergone arthroscopic ACL reconstruction procedure between Jan 2019 to July 2022 and subjects who were willing to provide written informed consent (in case of a physical visit to the site) or verbal informed consent (in case of a telephonic visit) were included in the study. Subjects who had suffered traumatic injury to the operated knee post ACL reconstruction procedure and subjects who were not willing to attend the follow-up were excluded from the study.
INTERPRETATION OF SCORES
International Knee Documentation Committee (IKDC): The IKDC questionnaire is a knee-specific patient-reported outcome measure. It is a subjective scale that provides patients with an overall function score. The questionnaire looks at 3 categories: symptoms, sports activity, and knee function. Scores are obtained by summing the individual items, then transforming the crude total to a scaled number that ranges from 0 to 100. This final number is interpreted as a measure of function with higher scores representing higher levels of function. The IKDC subjective knee form score can be calculated when there are responses to at least 90% of the items (i.e., when responses have been provided for at least 16 items) [16].
Modified Cincinnati Rating System (MCRS): The MCRS questionnaire consists of 12 questions, 8 of which are included in the summary score. These scored questions cover the domains of pain, swelling, function and activity level. The total score is calculated as the sum of all questions responses, higher scores representing the best/excellent knee function, and lesser scores representing the worst/poor knee function [17].
Tegner Activity Scale (TAS): Tegner activity level scale is a scale that aims to provide a standardized method of grading work and sporting activities. Tegner activity level scale is a graduated list of activities of daily living, recreation, and competitive sports. The patient is asked to select the level of participation that best describes their current level of activity and that before injury on a scale of 0 to 10. Zero represents disability because of knee problems and 10 represents participation in higher level activities [18].
Knee Injury and Osteoarthritis Outcome Score (KOOS): The KOOS is a valid, reliable, and responsive self-administered instrument that can be used for short-term and long-term follow-up of several types of knee injury including osteoarthritis. A modified version, knee-related quality of life is taken up for this study to assess the quality of life in patients after ACL reconstruction surgery. Higher scores represent the best quality of life and lower scores represent the poor quality of life [19].
Statistical Methods
Demographic measurements, medical history and surgery details were summarized descriptively. The primary endpoint of this study was functional outcomes using IKDC and MCRS questionnaires summarized using n, mean, median, standard deviation, minimum and maximum. Secondary endpoints of this study were TAS and quality of life subscale of KOOS score summarized as n, mean, median, standard deviation, minimum and maximum. ACL reconstruction failure rate was summarized descriptively. The adverse device effects (if any) were summarized as the number and percentage of the subjects with adverse events as well as the number of events.
Results
In this study, 44 subjects satisfying all the eligibility criteria were enrolled. The disposition of subjects was summarized in Table 1. The mean (SD) age was 34.5 (± 11.4) years. The number of males were 36 (81.8%) and females were 8 (18.2%) in the study. Out of 44 subjects, 35 (79.5%) did not have any comorbid conditions, followed by 4 (9.1%) had diabetes mellitus and 2 (4.5%) had hypertension. Demographic and surgery details were summarized in Table 2. Total mean (SD) duration of follow-up was 16 (± 7) months.
Table 1. Disposition of subjects
| Population | Overall |
|---|---|
| Screened | 44 |
| Enrolled, n (%) | |
| Yes | 44 (100.0) |
Table 2. Demographics and other baseline characteristics
| Demographic Characteristics | Overall (N=44) |
|---|---|
| Age (years) | |
| N | 44 |
| Mean | 34.57 |
| SD | 11.43 |
| Median | 34 |
| Min; Max | (19.00, 57.00) |
| Gender, n (%) | |
| Female | 8 (18.2) |
| Male | 36 (81.8) |
| Race, n (%) | |
| Asian | 44 (100.0) |
| Medical condition, n (%) | Overall (n = 44) |
| NA | 35 (79.5%) |
| Diabetes mellitus | 4 (9.1%) |
| Hypertension | 2 (4.5%) |
| Appendectomy | 1 (2.3%) |
| Asthma | 1 (2.3%) |
| Ear polyp removal | 1 (2.3%) |
| Hypothyroidism | 1 (2.3%) |
| ORIF with K-wires fracture of 5th finger | 1 (2.3%) |
| * NA - Not applicable; ORIF â?? Open reduction and internal fixation; SD - Standard deviation | |
| *Medical condition represents mixed data with one subject had both diabetes mellitus and ear polyp removal. Another subject had both hypothyroidism and asthma | |
Out of 44 subjects, 41 subjects received titanium interference screws of different dimensions on both femoral and tibial ends, 2 subjects had adjustable loop button on femoral side and titanium interference screw on tibial end, only 1 subject got PLDLA- BTCP interference screw on both femoral and tibial ends and 7 subjects had received all-inside meniscal repair devices. Disposition of the devices was summarized in Table 3.
Table 3. Disposition of implants
| Name of the Implants | Overall N=44 n (%) | |
|---|---|---|
| Femoral | ||
| Helysis® Interference Screw- Titanium | 41 (93.2) | |
| Helysis® ACL Screw-Titanium 9 mm×25 mm | 15 (34.1) | |
| Helysis® ACL Screw-Titanium 8 mm×25 mm | 12 (27.3) | |
| Helysis® ACL Screw-Titanium 7 mm×25 mm | 10 (22.7) | |
| Helysis® ACL Screw-Titanium 10 mm×25 mm | 4 (9.1) | |
| Proloop™ Adjustable Loop Button – 60 mm | 2 (4.5) | |
| Helysis® Interference Screw - PLDLA BTCP 9mmX30mm | 1 (2.3) | |
| Tibial | ||
| Helysis® Interference Screw- Titanium | 43 (97.7) | |
| Helysis® ACL Screw-Titanium 10 mm×30 mm | 12 (27.3) | |
| Helysis® ACL Screw-Titanium 8 mm×25 mm | 7 (15.9) | |
| Helysis® ACL Screw-Titanium 9 mm×30 mm | 7 (15.9) | |
| Helysis® ACL Screw-Titanium 10 mm×25 mm | 6 (13.6) | |
| Helysis® ACL Screw-Titanium 9 mm×25 mm | 6 (13.6) | |
| Helysis® ACL Screw-Titanium 10 mm×30 mm | 2 (4.5) | |
| Helysis® ACL Screw-Titanium 7 mm×30 mm | 1 (2.3 ) | |
| Helysis® ACL Screw-Titanium 7 mm×25 mm | 1 (2.3) | |
| Helysis® ACL Screw-Titanium 8 mm×30 mm | 1 (2.3) | |
| Helysis® Interference Screw – PLDLA BTCP 10mmX25mm | 1 (2.3) | |
| Meniscus | ||
| Sure Stitch™ - All inside meniscus repair implant | 7 (15.9) | |
* ACL – Anterior cruciate ligament; PLDLA BTCP - poly (L-co-DL lactic acid) and beta tricalcium phosphate |
||
Mean (SD) value of total IKDC score was 85.9 (±7.5) and MCRS score was 94.5 (± 6.8). Mean (SD) values of TAS before injury was 7.9 (± 0.9) and current status was 5.2 (±1.04). Mean (SD) value of quality of life subscale of KOOS score was 88.5 (± 9.2). Summary of all the scores were represented in Table 4.
Table 4. Summary of IKDC, MCRS, Tegner activity score and quality of life subscale from KOOS
| Characteristics | Overall (N=44) |
|---|---|
| Total IKDC Score | |
| Mean | 85.96 |
| SD | 7.54 |
| Median | 89.7 |
| Min; Max | (60.90, 93.10) |
| 95% CI for Mean | (83.67, 88.26) |
| Total MCRS Score | |
| Mean | 94.55 |
| SD | 6.87 |
| Median | 96.5 |
| Min; Max | (70.00, 100.00) |
| 95% CI for Mean | (92.46, 96.63) |
| Tegner Activity Score | |
| Level: Before Injury | |
| Mean | 7.93 |
| SD | 0.9 |
| Median | 8 |
| Min; Max | (6.00, 9.00) |
| 95% CI for Mean | (7.66, 8.21) |
| Level: Current | |
| Mean | 5.27 |
| SD | 1.04 |
| Median | 6 |
| Min; Max | (3.00, 7.00) |
| 95% CI for Mean | (4.96, 5.59) |
| Quality of life subscale of KOOS score | |
| Mean | 88.53 |
| SD | 9.25 |
| Median | 93.8 |
| Min; Max | (56.30, 93.80) |
| 95% CI for Mean | (85.72, 91.34) |
| *CI – Confidence Interval; IKDC - International Knee Documentation Committee; KOOS - Knee Injury and Osteoarthritis Outcome Score; MCRS - Modified Cincinnati Rating System Questionnaire; SD – Standard Deviation |
|
There was no significant association observed between the IKDC and MCRS scores with respect to type of implant used and duration of follow-up as presented in Table 5.
Table 5. Association of mean IKDC & MCRS Scores with type of implant and duration of follow-up
| Type of the Implant | Number of subjects, n | Mean IKDC Score | Mean MCRS Score |
|---|---|---|---|
| Helysis® titanium interference screw on both femoral and tibial ends | 41 | 87.4 | 94.9 |
| Surestitch™ - All inside meniscal repair implant | 7 | 86.5 | 94 |
| Proloop™ - Adjustable loop button on femoral end and Helysis® titanium interference screw on tibial end | 2 | 85.8 | 94.6 |
| Helysis® PLDLA-BTCP interference screw on both femoral and tibial ends | 1 | 87.4 | 93.9 |
| Duration of follow-up | Overall N (%) | ||
| < 6 months | 1 (2.2) | 60.9 | 70 |
| 6 months to 1 year | 11 (25) | 86.3 | 94.7 |
| 1 year to 2 years | 25 (56.8) | 85.9 | 94.5 |
| >2 years | 7 (15.9) | 87.2 | 94.9 |
| Mean (SD) of Total duration of follow-up (in months) | 16 (7) | ||
| *IKDC - International Knee Documentation Committee; MCRS - ; PLDLA BTCP - poly (L-co-DL lactic acid) and beta tricalcium phosphate; SD – standard deviation | |||
Discussion
This study results had shown certainly good post-operative functional outcomes pertaining to the standardized questionnaires. Majority of the enrolled subjects were males [36 (81.8%)]. Most of them [35 (79.5%)] did not have any comorbid conditions.
In this study, 41 subjects received titanium interference screws on both femoral and tibial ends and 2 subjects received adjustable loop button on femoral side and titanium screws on tibial side. The use of adjustable-loop devices has increased to compensate for the micromovement due to cortical suspensory fixation [20]. A recent study states that interference screw fixations have the advantage of reducing graft movement in the tunnel and synovial fluid influx and tunnel widening with interference screws was less than that with cortical suspensory fixation [21].
Primary objective was to assess the functional outcomes utilizing IKDC and MCRS questionnaires. Mean (SD) of IKDC score was 85.9 (±7.5) elucidating progress in symptoms, sports activity, and function postsurgery. Similar results found in a study comparing titanium and PEEK interference screws in which post-operative IKDC scores were 90 (± 8.9) and 89 (± 9.1) respectively indicating no significant differences between both [22]. Another study reported post-operative IKDC scores as 75.3 ± 17.4 and 80.5 ± 13.6 in the groups comparing adjustable-loop and interference screw fixation [23].
Substantial results were achieved with mean (SD) values of 94.5 (± 6.8) for MCRS questionnaire indicating excellent knee function. Similar results found in a study evaluating Single Bundle (SB) and Double Bundle (DB) ACL reconstruction with different techniques, scores were 90 in SB and 91 in DB postoperatively [24]. Another study of primary ACL reconstruction using biodegradable screws showed MCRS score as 92.9 (± 6.0) at 2-year post-operative follow-up [25].
Mean (SD) values of Tegner activity scale before injury was 7.9 ( ± 0.9) and current status was 5.2 ( ± 1.04) and that shows notable return to pre-injury activity levels in the daily living, recreation, and competitive sports. Equivalent results found in a study comparing functional outcomes in isolated Posterior Cruciate Ligament (PCL) group and combined ACL & PCL group with titanium interference screws, in which pre- injury to post-injury Tegner activity scores at 5 years followup in both groups were 6.83 to 6.23 and 6.72 to 5.82 respectively [26].
A favourable outcome with mean (SD) value of quality-of-life subscale of KOOS score obtained was 88.5 (± 9.2) representing better quality of life post-surgery. Similar results found in a study which showed improved quality of life in asymptomatic patients post ACL reconstruction was 81.8 [27].
There were no adverse device effects and reconstruction failures observed in this study. Contrast to this, a study from the Multi-center Orthopedic Outcomes Network (MOON) consortium found that a 4.4% graft re-tear rate which was positively associated with factors like younger age, type of the graft used (autograft or allograft), concomitant meniscal injuries or sport played [28], which we could not analyse in this study. Further studies investigating the factors effecting reconstruction failures such as type of ACL ruptures, types of meniscal lesions, tunnel widening, bone ingrowth etc. needs to be evaluated.
Limitations in the study include small sample size, retrospective nature and heterogenous reconstruction techniques. No comparison of the pre- and post-operative scores also bears as a limitation for the study.
Conclusion
Considering remarkable results in all the functional assessment scores and no incidence of reconstruction failures, this study concludes that ACL reconstruction using Sironix knee devices as safe and effective method. In addition, prospective studies with comprehensive clinical and functional evaluation need to be taken into account.
References
- Gordon MD. Anterior cruciate ligament injuries. Orthop. knowlegde update: sports med. 2004:169-81. [Google Scholar] [Cross ref]
- Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am. j. sports med. 2016;44(6):1502-7. [Google Scholar] [Cross ref]
- John R, Dhillon MS, Syam K, et al Epidemiological profile of sports-related knee injuries in northern India: an observational study at a tertiary care centre. J. clin. orthop. Trauma 2016;7(3):207-11. [Google Scholar] [Cross ref]
- Kochhal N, Thakur R, Gawande V. Incidence of anterior cruciate ligament injury in a rural tertiary care hospital. J. fam. med. prim. care 2019;8(12):4032. [Google Scholar] [Cross ref]
- Kiapour AM and Murray MM. Basic science of anterior cruciate ligament injury and repair. Bone jt. res. 2014;3(2):20-31. [Google Scholar] [Cross ref]
- Barber FA. Tripled semitendinosus–cancellous bone anterior cruciate ligament reconstruction with bioscrew fixation. Arthrosc. J. Arthrosc. Relat. Surg. 1999;15(4):360-7. [Google Scholar] [Cross ref]
- Sayampanathan AA, Howe BK, Bin Abd Razak HR, et al. Epidemiology of surgically managed anterior cruciate ligament ruptures in a sports surgery practice. J. Orthop. Surg. 2017;25(1). [Google Scholar] [Cross ref]
- Gamboa JT, Shin EC, Pathare NP, et al Graft retensioning technique using an adjustable-loop fixation device in arthroscopic anterior cruciate ligament reconstruction. Arthrosc. tech. 2018;7(2):e185-91. [Google Scholar] [Cross ref]
- Herickhoff PK, Safran MR, Yung P, et al. Pros and Cons of Different ACL Graft Fixation Devices. Controv. Tech. Asp. ACL Reconstr.: Evid.-Based Med. Approach 2017:277-88. [Google Scholar] [Cross ref]
- Kamitani A, Hara K, Arai Y, et al. Adjustable-loop devices promote graft revascularization in the femoral tunnel after ACL reconstruction: comparison with fixed-loop devices using magnetic resonance angiography. Orthop. J. Sports Med. 2021;9(2). [Google Scholar] [Cross ref]
- Barrett GR and Brown TD. Interference Screw Fixation in Bone–Patellar Tendon–Bone Anterior Cruciate Ligament Reconstruction.
- Bourke HE, Gordon DJ, Salmon LJ, et al The outcome at 15 years of endoscopic anterior cruciate ligament reconstruction using hamstring tendon autograft for ‘isolated’anterior cruciate ligament rupture. J. bone jt. surg., Br. vol. 2012;94(5):630-7. [Google Scholar] [Cross ref]
- Papalia R, Vasta S, D'Adamio S, et al Metallic or bioabsorbable interference screw for graft fixation in anterior cruciate ligament (ACL) reconstruction?. Br. med. bull. 2014;109(1):19-29. [Google Scholar] [Cross ref]
- Pache S, Aman ZS, Kennedy M, et al. Meniscal root tears: current concepts review. Arch. Bone Jt. Surg. 2018;6(4):250. [Google Scholar] [Cross ref]
- Forkel P, Reuter S, Sprenker F, et al Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg. Sports Traumatol. Arthrosc. 2015;23:112-8. [Google Scholar] [Cross ref]
- Irrgang JJ, Anderson AF, Boland AL, et al Development and validation of the international knee documentation committee subjective knee form. Am. j. sports med. 2001;29(5):600-13. [Google Scholar] [Cross ref]
- Noyes Fr, Barber Sd, Mooar La. A rationale for assessing sports activity levels and limitations in knee disorders. Clin. Orthop. Relat. Res. (1976-2007). 1989;246:238-49. [Google Scholar] [Cross ref]
- Tegner YE and Lysholm JA. Rating systems in the evaluation of knee ligament injuries. Clin. Orthop. Relat. Res. 1985;198:42-9. [Google Scholar] [Cross ref]
- Roos EM, Roos HP, Lohmander LS, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. Clin Orthop Relat Res. 1998;28(2):88-96. [Google Scholar] [Cross ref]
- Onggo JR, Nambiar M, Pai V. Fixed-versus adjustable-loop devices for femoral fixation in anterior cruciate ligament reconstruction: a systematic review. Arthrosc.: J. Arthrosc. Relat. Surg. 2019;35(8):2484-98. [Google Scholar] [Cross ref]
- Mayr R, Smekal V, Koidl C, et al. Tunnel widening after ACL reconstruction with aperture screw fixation or all-inside reconstruction with suspensory cortical button fixation: volumetric measurements on CT and MRI scans. The Knee. 2017;24(5):1047-54. [Google Scholar] [Cross ref]
- Shumborski S, Heath E, Salmon LJ, et al. A randomized controlled trial of PEEK versus titanium interference screws for anterior cruciate ligament reconstruction with 2-year follow-up. Am. J. Sports Med. 2019;47(10):2386-93. [Google Scholar] [Cross ref]
- Lee TJ, Jang KM, Kim TJ, et al. Adjustable-Loop Cortical Suspensory Fixation Results in Greater Tibial Tunnel Widening Compared to Interference Screw Fixation in Primary Anterior Cruciate Ligament Reconstruction. Medicina. 2022;58(9):1193. [Google Scholar] [Cross ref]
- Toker B, Erden T, Dikmen G, et al Clinical outcomes of single-bundle versus double-bundle ACL reconstruction in adolescent elite athletes: A retrospective comparative study. Acta Orthop. Traumatol. Turc. 2022;56(1):20-5. [Google Scholar] [Cross ref]
- Zhao N, Tao K, Wang G, et al. Global obesity research trends during 1999 to 2017: A bibliometric analysis. Medicine. 2019;98(4). [Google Scholar] [Cross ref]
- Gupta R, Singhal A, Kapoor A, et al Similar functional outcomes of arthroscopic reconstruction in patients with isolated Posterior Cruciate Ligament (PCL) and combined Anterior Cruciate Ligament (ACL) and PCL tears. J. Clin. Orthop. Trauma 2021;16:65-9. [Google Scholar] [Cross ref]
- Davis-Wilson HC, Thoma LM, Longobardi L, et al. Association of Quality of Life With Moderate-to-Vigorous Physical Activity After Anterior Cruciate Ligament Reconstruction. J. Athl. Train. 2022;57(6):532-9. [Google Scholar] [Cross ref]
- Kaeding CC, Pedroza AD, Reinke EK, et al. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am. j. sports med. 2015 Jul;43(7):1583-90. [Google Scholar] [Cross ref]





 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.