Dysfunctional sacroiliac joint pain following lumbar discectomy/laminectomy
Received: 25-May-2017 Accepted Date: Jul 11, 2017 ; Published: 14-Jul-2017
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Overview of Literature: Pain arising at the sacroiliac joint is in most instances dysfunctional without concomitant radiographic findings. There have been some reports in the literature describing the occurrence of sacroiliac joint pain following lumbar spine surgery including laminectomy, discectomy and fusion. However, the issue hasn’t yet been widely evaluated in the literature.
Purpose: The aim of this study is to evaluate the incidence and laterality of dysfunctional sacroillac joint pain following lumbar spine surgery without fixation and to evaluate the efficacy of fluoroscopic or CT guided injection as a diagnostic and therapeutic tool.
Study Design: Forty-four patients suffering back pain and / or lower extremity pain with recent history of spinal operation are included having pain clinically suspicious of being of sacroiliac origin.
Methods: Clinically suspected patients were offered either fluoroscopy or CT guided sacroiliac joint injection using a 19-gauge spinal needle and injection of intraarticular 4 cc xylocain and 40 mg Triamcinolone acetonide (kenacort R) aiming at the S2 mid-sacral level.
Results: 18 patients were males and 26 patients were females. The age of patients ranged from 22 years to 65 years with a mean of 43 years. Previous operation done included 34 patients undergoing single level discectomy, and 10 patients had laminectomy for canal stenosis. Post injection response classified to negative responders (6) and positive responders (38) patients. The duration of improvement in positive responder group lasted from 14 days to 6 months with an average of 73 days.
Conclusion: A painful SIJ should be more considered as a differential diagnosis in patients with low back pain and leg pain in patients with prior lumbar surgery without fixation. The use of accurate diagnostic, therapeutic injections helps both diagnosis and pain relief.
Keywords
Lumbar surgery, Sacroiliac pain, Sacroiliitis, Injections
Introduction
Cases of recurrent low back pain and/or lower extremity pain after lumbar/lumbosacral surgery are referred to as failed back surgery syndrome [1]. Several authors have suggested that the sacroiliac joint (SIJ) may be a possible source of persistent pain [2,3].
The SIJ as a pain generator results in pseudo-radicular symptoms that may resemble pain generated due to lumbar roots compression. This diversity of diffuse pain referral may be explained by the fact that the sacroiliac joint receives liberal innervations from L2 to S2 roots [4-6]. The SIJ pain referral zones have been reported to include the posterosuperior iliac spine, lower lumbar region, upper lumbar region, buttock, greater trochanteric region, groin and medial thigh, anterior thigh, posterior thigh, lateral thigh, posterior calf, lateral calf, anterior calf, ankle, and foot [7-9]. Early published referral patterns of SIJ provocation or irritation were based on patients’ complaints and physical examination. Dreyfuss et al. reported that only 4% of patients with SIJ pain marked any pain above L5 on self-reported pain drawings [10]. Referral of pain into various locations of the lower extremity does not distinguish SIJ pain from other pain states. For example, Schwarzer et al. found that pain below the knee and into the foot was as common in SIJ pain as for other sources of pain [9]. Slipman et al. conducted a retrospective study to determine the pain referral patterns in 50 patients with injection-confirmed SIJ pain [11]. The most common referral patterns for SIJ pain were found to be radiation into the buttock (94%), lower lumbar region (72%), lower extremity (50%), groin area (14%), upper lumbar lesion (6%), and abdomen (2%). Twenty-eight percent of patients experienced pain radiating below their knee, with (12%) reporting foot pain. Based on the existing data, the most consistent factor for identifying patients with SIJ pain is unilateral pain (unless both joints are affected) localized predominantly below the L5 spinous process.
Pain arising at the sacroiliac joint is in most instances dysfunctional without concomitant radiographic findings [10]. There have been some reports in the literature describing the occurrence of sacroiliac joint pain following lumbar spine surgery including laminectomy, discectomy and fusion [12-16]. Although the occurrence of this condition may yield in un-gratifying results as evaluated by the patient the issue hasn’t yet been widely evaluated in the literature.
The aim of this study is to evaluate dysfunctional sacroiliitis occurring following lumbar discectomy and/or laminectomy and evaluate the efficacy of fluoroscopic or CT guided injection as a diagnostic and therapeutic tool.
Materials and Methods
This study included 44 patients with complaints suggestive of sacroiliac joint pain post lumbar surgery from a total of 461 patients undergoing non-instrumented lumbar surgery during through 24 months between February 2014 and February 2016.
The selection criteria include:
1. New pain clinically pointing to sacroiliac origin with no previous preoperative suspicion of sacroiliac joint generated pain.
2. Spinal operation within 6 months.
3. Initial improvement of patients back and /or leg pain (complete resolution of preoperative complaint) followed by occurrence of new pain ipsilateral or contralateral to pain of previous complaint.
4. Failed improvement after conservative therapy and nonsteroidal drugs.
5. Absence of neurological deficit.
All patients had full history taking and complete neurological examination.
Physical examination tests have been advocated as diagnostic aids in patients with presumed SIJ pain [17]. Examples of these tests include Patrick’s test, Yeoman’s test, [18] The Patrick, or FABER (flexion abduction and external rotation) which stresses the hip and SIJ. The test is performed by moving the flexed, abducted, and externally rotated hip to an extended position. If the test is positive, the patient describes pain at the posterior superior iliac spine and the SIJ. The Yeoman test is performed with the patient prone. The test is performed by extending the hip and rotating the ilium. Usually, the patient will report pain over the posterior SIJ, specific tenderness over the sacral sulcus as well as the posterior sacroiliac spine Gaenslen’s test, Gillet’s test, the compression test, and the thigh thrust test. However, when applying pain provocation tests, it is nearly impossible to define which structures are actually stressed [19]. Even structures such as the iliolumbar ligament or piriformis muscle cannot be excluded as potential sources of pain because they are functionally related [3,20]. Consequently, it is very difficult to determine whether the pain that is provoked is exclusively intra-articular or whether it is related to capsular ligaments. Previous studies have reported that there is no one single specific physical examination that can accurately identify a painful SIJ [5,17,21,22]. Dreyfuss et al. [5,19] found that 20% of asymptomatic adults had positive findings on commonly performed SIJ provocation tests and that the test with the highest sensitivity was the test of sacral sulcus tenderness (89%), although this test exhibited poor specificity. Slipman et al. [22] reported a positivepredictive value of 60% in diagnosing SIJ pain in patients using a positive response to three SIJ provocation tests. Broadhurst and Bond [23] reported a sensitivity of 77% to 87% for positive responses to three SIJ provocation tests. Thus, there is evidence of good diagnostic validity of positive responses to a threshold of three SIJ provocation tests to identify SIJ pain [23,24]. However, there are no studies that have specifically examined provocation tests in patients with SIJ pain after lumbar/lumbosacral fusion.
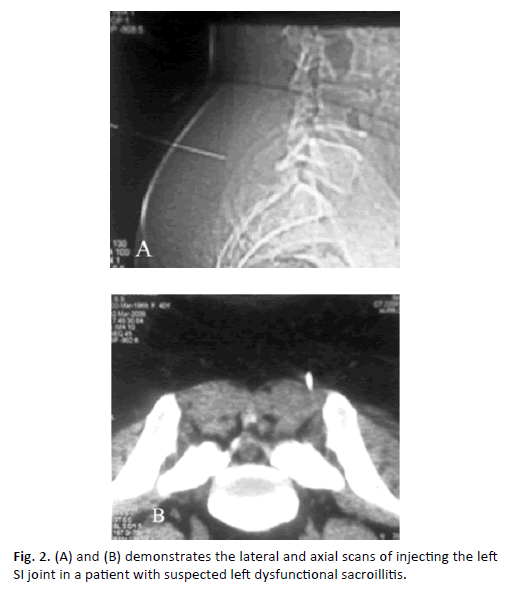
Clinically suspected patients were offered either fluoroscopy or CT guided sacroiliac joint injection using a 19-gauge spinal needle and injection of intraarticular 4 cc xylocain and 40 mg Triamcinolone acetonide (kenacort R) aiming at the S2 mid-sacral level.
The clinical response was evaluated and documented.
The outcome of injection was assessed as described by patients in terms of pain and movement and was classified into two groups:
1. Negative responders (non-sacroiliac joint pain): including those with no clinical improvement or rapid recurrence of symptoms within 14 days [7].
2. Positive responders: including those with sustained clinical improvement further than 14 days (38 patients).
The duration of maximal clinical improvement is recorded.
Results
Forty-four patients meeting the selection criteria were included. 18 patients were males and 26 patients were females. The age of patients ranged from 22 years to 65 years with a mean of 43 years. The nature of previous operation done included 34 patients undergoing single level discectomy (12 patients with microdiscectomy or fenestration and 22 with formal laminectomy). Ten patients had laminectomy for canal stenosis. Table 1 demonstrates the type of previous procedure.
| Type of intervention | Number of patients (%) |
|---|---|
| Discectomy | 34(77.3%) |
| Microdiscectomy | 12 |
| Discectomy through formal laminectomy | 22 |
| Simple laminectomy | 10(22.7%) |
Table 1: Shows the type of initial intervention.
The occurrence of pain was in the ipsilateral side as preoperative complaint in 18 patients, and in the contralateral side in 22 patients. Four patient had no preoperative sciatica but bilateral neurogenic claudications and developed a new onset of limb pain one in the right side the other in left side. The distribution of pain was recorded as shown in Table 2.
| Area of pain distribution | Number of patients |
|---|---|
| Paramedian low back pain | 40 |
| Buttock, groin and thigh | 38 |
| Leg pain (below knee referral) | 26 |
| Ankle and foot | 14 |
Table 2: Shows the distribution of pain among patients.
Examination of patients revealed local tenderness over the sacroiliac joint in 38 patients, Yeoman test positive in 34 patients, Faber test positive in 32 patients. The clinical signs are shown in Table 3.
| Test | Number of patients (Total 44) |
Number of patient in positive responders (total 38) (%) |
|---|---|---|
| SIJ local tenderness | 38 | 34 (89.5%) |
| Yeoman test | 34 | 30 (79%) |
| Faber test | 32 | 28 (73.7%) |
Table 3: Shows the clinical sign elicited.
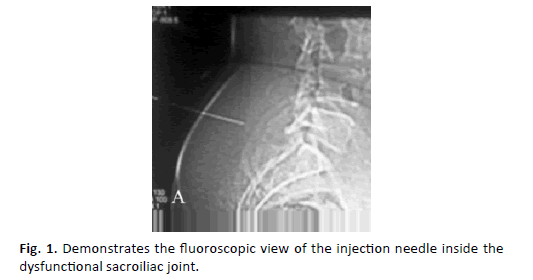
X-ray of the sacroiliac joint revealed sclerosis of joint in 6 patients otherwise it was normal in 38 patients. Fluoroscopy or CT guided injection was successfully done in all patients with no complications reported (Figure. 1).
These x-ray findings were detected in older preoperative studies and were not considered correlating to the new onset of symptoms.
The clinical response of patients was recorded as follows:
* Negative responders: 6
* Positive responders: 38 patients.
Among the positive responder group (38 patients): 16 patients reported the pain in the same side as preoperative complaint and 18 patients had pain in the contralateral side to preoperative complaint and four patient had no preoperative sciatica but was only complaining neurogenic claudication on exercise. Thirty-four (89.5%) patients, had positive local tenderness over the joint.
All 38 patients in the positive responder group had more than one clinical test positive of sacroiliac source of pain.
The incidence of patients proved to have sacroiliac joint generated pain was 8.2% (38 out of 461).
The duration of improvement in positive responder group lasted from 14 days to 6 months with an average of 73 days (Figure. 2A and Figure. 2B).
Patients with improvement sustained for 6 month or more: 10 patients.
Patients with improvement sustained for 3-6: 14 patients.
Patients with improvement sustained for 1-3 month: 12 patients.
Patients with improvement sustained for less than 1 month: 2 patients.
The duration of improvement is shown in Table 4.
| Duration | Number of patients (%) |
|---|---|
| 6 month or more | 10 (26.3%) |
| 3-6 months | 14 (36.8%) |
| 1-3 months | 12 (31.6%) |
| less than 1 month | 2   (5.3%) |
Table 4: Shows the duration of improvement in positive responder group (Total 38 patients).
Discussion
The sacroiliac joint is a well-known pain generator that may very much mimic pain generated due to lumbar radiculopathy. This diversity of diffuse pain referral may be explained by the fact that the sacroiliac joint receives liberal innervations from L2 to S2 roots [24,25]. The typical symptoms include low back pain that frequently radiates to the buttocks and thigh or even the leg and foot [20,26,27].
The clinical examination points to the suspicion of involved sacroiliac joint as a pain generator, and even though a large number of provocative clinical tests are described still sure diagnosis may not be clinically ascertained. These manoeuvres have been demonstrated to have poor inter- and intratester reliability [28,29], and have been found positive in 20% of asymptomatic individuals [19].
Radiological investigations including magnetic resonance imaging, computed tomography, and bone scans of the sacroiliac joint cannot also reliably determine whether the joint is the source of the pain and thus controlled analgesic injections of the sacroiliac joint are the most important tool in the diagnosis [10].
Few reports in the literature have pointed to the occurrence of sacroiliac joint pain following lumbar spine surgery including laminectomy, discectomy and fusion [12-16].
The proposed mechanism behind sacroiliac dysfunction following lumbar procedures particularly spinal fixation include altered mechanics and new stresses placed over the joint due to correction of pelvic tilt that accompanies unilateral limb pain [13-15]. In one study conducted to evaluate sacroiliac joints by SPECT scan it was found that the uptake of sacroiliac joints increased in patients who had undergone prior lumbar laminectomy and/or spinal fusion. Such spinal surgery can increase impact loading on the SIJ, leading to mechanical overload and functional sacroiliitis [14].
Although the sure diagnosis of this condition requires diagnostic injection, the presence of sacroiliac tenderness is one of the most consistent findings in patients with sacroiliac dysfunction. The positivity of multiple provocative tests raises more confidence in the diagnosis [18]. Sacroiliac joint local tenderness was present in 38 (86.4%) patients in the positive responder group in this series. All negative responders (6 patients) had a single clinical positive test suspecting sacroiliac joint pain.
In this study we have selected patients with high clinical suspicion of having sacroiliitis as a pain generator following initial improvement after lumbar spine surgery. We have selected to perform a diagnostic/ therapeutic injection but using the fluoroscopic or CT guidance technique. Several techniques for injection has been described. The free hand technique has a very high incidence of improper placement of needle in about 50% of cases [25,30] and thus bedside injection may be very misleading in result. Fluoroscopy guided injections are also accurate but may require the injection of dye into the joint and utilizes large dose of radiation. The use of CT for needle placement is unmatched in accuracy besides the easy localization in obese patients and selection of the target whether intra-articular or periarticular [31].
Our results have shown that the sacroiliac joint was the pain generator in 38 patients (86.4%) of those clinically suspected of having the condition and only 6 patients (13.6%) were nonresponders, whereas most surgeons are familiar with causes of failed back including scarring, adhesions, recurrence of disc and facet arthropathy, painful sacroiliac joint may not be as familiar and therefore may not be considered in patients with back or leg pain after spinal operations [13].
The selection criteria of patients in this study, included absence of spinal pathology that might be responsible for the patient’s complaint. In clinical practice, however, concomitant asymptomatic radiological findings including a lumbar disc herniation may coincidently be present but not responsible for the patient’s complaint. Irwin and Haris [25], reported two cases of lumbar disc herniation who failed to improve after transforaminal steroid root injection. Both patients proved to be of dysfunctional sacroiliac joint nature later on. Thus, patients with clinical suspicion of having sacroiliac joint pain even in presence of MRI findings that might cause the radiculopathy should undergo a diagnostic injection before unnecessary discectomy is performed.
The numbers of patients in who prolonged improvement among positive responders in our study were 24 patients (63.2%) whereas 14 patients (36.8%) were documented as sacroiliac joint pain but with shorter duration of clinical improvement. Patients with documented diagnosis can further be managed by repeated injection and in resistant cases, radiofrequency ablation or sacroiliac arthrodesis may be considered [1,32].
The overall incidence of post non-instrumented SIJ pain was found to be 8.2% which is lower than the reported incidence of SIJ pain in instrumented posterior lumbar fixation. The new onset lower extremity symptoms among positive responder patient group occurred in the ipsilateral side of previous complaint in 42.1% of cases and in contralateral side in 47.4% denoting that the stress loads may affect either side.
Conclusion
The use of diagnostic injections should increase by the spine surgeons. A painful SIJ should be more considered as a differential diagnosis in patients with low back pain and leg pain in patients with prior lumbar. The use of accurate diagnostic, therapeutic injections helps both diagnosis and pain relief.
REFERENCES
- Ferrante F.: Regional anesthesia & pain medicine. 2001; 26(2): 137-142.
- Ebraheim N.A., Elgafy H., Semaan H.B.: Computed tomographic findings in patients with persistent sacroiliac pain after posterior iliac graft harvesting. Spine. 2000; 25: 2047-2051.
- Maigne J.Y., Planchon C.A.: Sacroiliac joint pain after lumbar fusion. A study with anesthetic blocks. Eur Spine J. 2005; 14: 654-658.
- Bernard T., Cassidy J.D.: The sacroiliac joint syndrome: pathophysiology, diagnosis, and management. In: Frymoyer JW, ed. The adult spine: principles and practice, 2nd ed. New York: Raven Press, 1997; 2343-2366.
- Dreyfuss P., Michaelson M., Pauza K., et al.: The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine. 1996; 21: 2594-2602.
- Grob K.R., Neuhuber W.L., Kissling R.O.: Innervation of the human sacroiliac joint. Rheumatol. 1995; 54: 117-122.
- Bernard T., Kirkaldy-Willis W.: Recognizing specific characteristics on non-specific lower back pain. ClinOrthop. 1987; 217: 266-280.
- Fortin J., Aprill C., Dwyer A., et al.: Sacroiliac joint: pain referral maps upon applying a new injection/arthrography technique. Part I: Asymptomatic volunteers. Spine. 1994; 19: 1475-1482.
- Schwarzer A.C., Aprill C.N., Bogduk N.: The sacroiliac joint in chronic low back pain. Spine. 1995; 20: 31-37.
- Dreyfuss P., Dreyer S., Cole A., et al: Sacroiliac joint pain: J Am AcadOrthop Surg. 2004; 12(4): 255-265.
- Slipman C.W., Jackson H.B., Lipetz J.S., et al.: Sacroiliac joint pain referral zones. Arch Phys Med Rehabil. 2000; 81: 334-338.
- Elias W., Simmons N., kaptain J.: Complications of posterior lumbar interbody fusion when using a titanium threaded cage device. J Neurosurg (Spine 1). 2000; 93: 45-52.
- Katz V., Schofferman J., Reynolds J.: The sacroiliac joint: A potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech. 2003; 16(1): 96-99.
- Onsel C., Collier B.D., Kir K.M., et al.: Increased sacroiliac joint uptake after lumbar fusion and/or laminectomy. ClinNucl Med. 1992; 17(4): 283-287.
- Slipman C.W., Shin C.H., Patel R.K., et al.: Etiologies of failed back surgery syndrome. Pain Med. 2002; 3: 200-207.
- Waguespack A., Schofferman J.: Etiology of long-term failures of lumbar spine surgery. Pain Med. 2002; 3: 18-22.
- Cohen S.P., Rowlingson J., Abdi S.: Low back pain. In: Warfield XA, Bajwa ZA (eds) Principles and practice of pain medicine, 2nd edn. McGraw-Hill, New York, 2004; 273-284.
- Zelle A., Gruen G., Brown S., et al.: Sacroiliac joint dysfunction, evaluation and management. Clin J Pain. 2005; 21: 446-455.
- Dreyfuss P., Dreyer S., Griffin J., et al.: Positive sacroiliac screening tests in asymptomatic adults. Spine. 1994; 19: 1138-1143.
- Fortin J., Aprill C., Ponthieux B., et al. Sacroiliac joint: pain referral maps upon applying a new injection/arthrography technique: II. Clinical evaluation. Spine. 1994; 19: 1483-1489.
- Ahn Y., Lee S.H. Iatrogenic sacroiliac joint syndrome after percutaneous pedicle screw fixation at the L5-S1 level: case report. Neurosurgery. 2010; 67: E865-E866.
- Slipman C.W., Sterenfeld E.B., Chou L.H., et al.: The predictive value of provocative SIJ stress maneuvers in the diagnosis of sacroiliac joint syndrome. Arch Phys Med Rehabil. 1998; 79: 288-292.
- Broadhurst N.A., Bond M.J.: Pain provocation test used for assessment of SIJ dysfunction. J Spinal Disord. 1998; 11: 341-345.
- Young S., Aprill C., Laslett M.: Correlation of clinical examination characteristics with three sources of chronic low back pain. Spin J. 2003; 3: 460-465.
- Irwin R.W., Harris M.B.: Concomitant sacroiliac joint pain in patients with lumbar disc herniation: case series. J SurgOrthop Adv. 2004; 13(4): 224-227.
- Maigne J., Aivaliklis A.: Results of sacroiliac joint double block and value of sacroiliac provocative tests in 54 patients with low back pain. Spine. 1996; 21: 1889-1892.
- Slipman C.W., Patel R.V., Whyte W.S., et al.: Diagnosing and managing sacroiliac pain. J Musculoskel Med. 2001; 18: 325-332.
- Carmichael J.P.: Inter- and intra-examiner reliability of palpation for sacroiliac joint dysfunction. J ManipPhysTher. 1987; 10: 164-171.
- Potter N., Rothstein J.: Intertester reliability for selected clinical of the sacroiliac joint. PhysTher. 1992; 12: 903-916.
- Murakami E., Tanaka Y., Aizawa T., et al.: Effect of periarticular and intraarticular lidocaine injections for sacroiliac joint pain: prospective comparative study. J Orthop Sci. 2007; 12(3): 274-280.
- Pulisetti D., Ebraheim N.A.: CT-guided sacroiliac joint injections. J Spinal Disord. 1999; 12(4): 310-312.
- Buchowsk I., Kebaish K., Sinkov V., et al.: Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint.The Spine Journal. 2005; 5: 520-528.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.