Double-button technique for the treatment of high degree AC-joint dislocations
2 Department of Orthopedic Surgery, Hospital Traumatologico, Concepcion, Chile
Received: 28-Apr-2020 Accepted Date: May 18, 2020 ; Published: 26-May-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: To evaluate clinical and radiological outcomes of Rockwood Type-V Acromioclavicular joint (AC-joint) dislocations, surgically treated with a double button device, within 5 days after trauma.
Methods: Eighty-six patients (80 males, 6 females) operated under radiological guidance with the Zip-Tight® fixation device were evaluated. The mean age of these patients was 37.9 years old (18-60). Radiological evaluation measuring Clavicle-coracoid (CC) distance was performed. Clinical evaluation was made by Acromioclavicular Joint Instability score (ACJI) and Simple Shoulder Test (SST).
Results: The average Follow-up (FU) was 24.2 months (12-32). The mean CC distance was 8.5 mm after surgery, and at the last FU it was 8.9 mm (not significant). Clinical outcomes at the last FU were; mean ACJI score: 84.7. Mean SST score: 11.5. Thirty-six patients (41.9%) present some degree of horizontal displacement of the clavicle (mean ACJI score: 73.5) and 50 patients (58.1%) did not present displacement (mean ACJI score: 95.2). This difference was statistically significant (p<0.001). There were no significant differences in either subjective (pain, tenderness, daily live activities and cosmesis) or in strength parameters between these groups.
Conclusion: The surgical treatment of high degree AC-joint dislocation using double-button device provides a stable fixation and satisfactory clinical and radiological results at intermediate-term FU.
Keywords: Acromioclavicular dislocation, double-button fixation, outcomes, shoulder surgery
Introduction
Traumatic Acromioclavicular (AC) joint dislocations are frequent among the young athletic population [1,2]. Nine percent of the shoulder girdle lesions affect the AC-joint, and the reported incidence in the U.S.A. is 3-4 per 100.000 [3]. The most frequent injury mechanism leading to a dislocation of the AC-joint is a direct trauma applied over the shoulder region (a fall or a direct blow), with the arm in an adducted position. Less frequently AC-joint dislocations result from an indirect trauma: by falling over an adducted outstretched hand or elbow, causing the humerus to translocate superiorly and driving the humeral head into the acromion [2].
Biomechanically, AC joint separation involves a sequential injury of different shoulder structures: it starts with the acromioclavicular ligaments disruption, progressing into the Clavicle-coracoid (CC) ligament complex rupture and finally involving the deltoid and trapezius muscles and fascia [4]. Rockwood and Green classified the AC joint dislocations into 6 types, according to its degree of severity [5]. Rockwood types I and II are managed conservatively, whereas in the case of Rockwood types IV to VI surgical stabilization is indicated [2,6]. However, management of Rockwood type III remains controversial, because some authors recommend a conservative treatment and others suggest surgical stabilization, particularly for athletes or manual workers who perform overhead activities [7-10]. Furthermore, there is still controversy about which kind of technique is advisable to use in patients with surgical indication.
More than 70 different surgical procedures have been reported, including coracoacromial ligament transfer, plate fixation, wire fixation and screw fixation, with no gold standard established until now. Many of these techniques are often associated with complications, such as coracoid fracture, loosening, breakage and/or migration of the hardware, loss of reduction and postoperative osteoarthritis [9,11,12]. Recent evidence suggests that an anatomical reconstruction of the ACjoint would improve the results [13-24].
For that purpose, novel anatomical-like techniques of acute ACjoint dislocation have been introduced [22,23]. One of them is the use of 2 flip-button devices with or without biological reinforcement to independently augment the conoid and trapezoid ligaments with non-absorbable sutures in order to get an anatomical healing of the CC ligaments, which would act as a scaffold to permit this process while maintaining a stable reduction of the AC-joint [22]. Nonetheless, even after anatomical reconstruction of the AC-joint, radiological and clinical improvements are still debatable, due mostly to residual pain associated with postoperative posterior displacement of the clavicle.
In search of a more significant outcome for the AC-joint dislocated patient, we introduced an early intervention scheme for these types of lesions in our center by performing surgery within 5 days after the trauma occurs. We found that, by introducing this scheme, joint stabilization was significantly improved in terms of clinical and radiological outcomes.
Materials and Methods
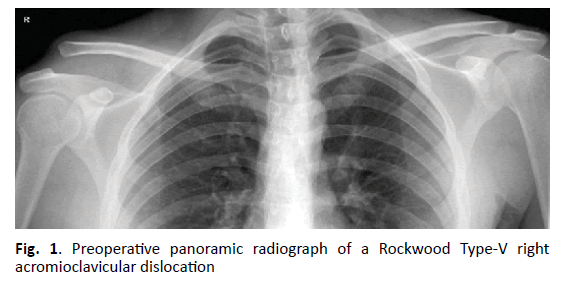
All surgical procedures, clinical Follow-up (FU), and data analyses were in accordance with the Institutional Review Board of the hospital. Between September 2014 and June 2017, 123 consecutive patients (108 males, 15 females) with an acute AC-joint dislocation were operated on using an open and radiological guided technique. For this prospective cohort study, 95 patients were included under the following criteria: Rockwood Type-V AC-joint dislocations and surgery performed within 5 days after trauma. Exclusion criteria were previous shoulder surgery and concomitant presence of acromial, coracoid or clavicular fracture. Preoperative evaluation was performed with panorama (bilateral) AP view (Fig. 1). Postoperatively bilateral AP view and Alexander view were performed at 1 month, 6 months and at last FU. Clinical evaluation was performed with the Simple Shoulder Test (SST) and the Acromioclavicular Instability Score (ACJI) [23,25].
Surgical Technique
General anesthesia and interscalene brachial plexus block were used for all the patients along with perioperative antibiotics. The patient was placed in the supine decubitus position, with 20° of thoracic elevation. The shoulder and ipsilateral arm were prepared and draped in a sterile fashion. A vertical 5 cm incision was done, taking care of preserving the clavipectoral fascia adequately. To perform the AC-joint stabilization, the X ray image intensifier was positioned anteriorly showing an AP view of the AC-joint.
A 2.5 mm tunnel was subsequently drilled 4 cm medial to the ACjoint. Keeping the drill in this position, this tunnel was overdrilled with a cannulated 4.5 drill, and the AC-joint was considered reduced. Under X-ray inspection, a 2.5 mm tunnel was drilled through the center of the coracoid, followed by a 4.5 cannulated drill. While keeping the joint reduced, a Zip-Tight® fixation system (Biomet, Warsaw, USA), consisting on a self-retained round clavicular (6.5 mm diameter) and an oblong coracoid titanium button (10 mm × 3.5 mm), connected by high resistance non-absorbable Nº 5 super-suture, was inserted under radiological view. The position of the devices and the reduction of the AC-joint were then observed under an image intensifier. The deltotrapezoidal fascia was then closed. The sub-dermic tissue and skin were stitched separately.
A sling was postoperatively used to protect the shoulder for 6 weeks. During that time, a passive range of motion exercises were allowed up to 45° of abduction and flexion during the first 3 weeks and up to 90° in following 3 weeks. After 6 weeks, an active range of motion exercises were allowed. Weight-bearing exercises were allowed when the patient achieved full range of motion (not before 7 weeks).
Postoperative Evaluation
Postoperative clinical and radiological evaluations were performed by two examiners, different from the surgeons. Complete physical examination of both shoulders was done. Two tests or scores were used to evaluate the outcomes: SST (maximum 12 points) and ACJI (maximum 100 points).
ACJI score was described and published in detail by Scheibel et al. [23]. Abduction strength was measured with an isometric dynamometer (Isobex TM dynamometer, Medical Devices Solutions AG, Burgdorf, Switzerland) in 90° of abduction in the scapular plane of both shoulders. Postoperative AP radiographic view with 10 kg load and Alexander view of both shoulders were performed to evaluate the presence of AC-joint osteoarthritis, and to evaluate vertical and horizontal displacement of the clavicle.
The displacement of the clavicle was measured in the bilateral AP stress view with 10 kg load. The Coracoclavicular (CC) distance of both sides was measured, as the distance between the inferior cortex of the clavicle and superior cortex of the coracoid process. The horizontal position of the joint was evaluated in the Alexander view. The position of the clavicle regarding the acromion was evaluated. A stable joint was defined as the clavicle in line with the acromion. A subluxated joint was described when the joint was incongruent, with a displacement of the clavicle less than one clavicle shaft width. A dislocated joint was defined when the displacement of the clavicle was more than one width.
Migration of the implants between the clavicle and the coracoid process were classified as: none, up to the superior cortex of the clavicle, up to the clavicle or the coracoid process, and full migration, as described by Scheibel et al. [23]. Ossifications between the clavicle and the coracoid were evaluated and differentiated into none, mild, moderate and severe.
Descriptive and univariate statistics analysis were performed using SSPS 13.0. Groups were compared using the Mann-Whitney U test. Comparison of metric data within one group was performed with Wilcoxon Signed Ranks Test. Statistical differences were defined with a P value<0.05.
Result
Ninety-five patients with Rockwood Type-V AC-joint dislocation were surgically treated with a double button technique, using a Zip- Tight® fixation device. There was a mean of 2.3 days (range, 0-5 days) delay between the trauma and the surgery for this group of patients.
After a mean of 24.2 months (range, 12-32 months) 86 patients were available for clinical and radiological evaluation. Six patients were women and 80 were men. The mean age of this group was 37.9 years (range, 18-60 years). The dominant side was affected in 47 cases (54.7%) and the nondominant side in 39 patients (45.3%). Of the 9 patients lost to FU, one case had presented a skin infection that recovered after antibiotic treatment.
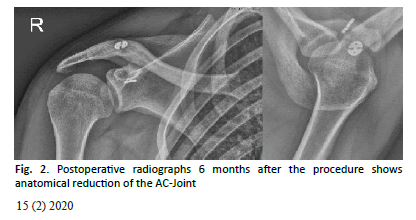
Radiological assessment was performed at 1 month, 6 months and at last FU (Fig. 2). The mean CC distance was 8.5 mm (4-13.3) after surgery and at the last FU was 8.9 mm (4.3-13.4). This difference was not significant. The mean CC distance in the non-affected side was 8.1 mm (5-12.6). Compared to the mean CC distance of the injured shoulder with non-affected side at last FU, this difference was not significant. Three patients (9.3%) showed moderate ossification between the clavicle and the coracoid in the area of the CC ligaments.
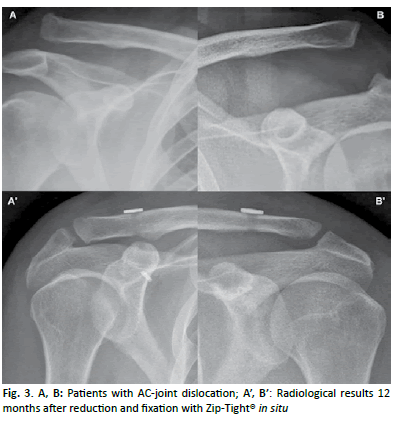
At the last FU mean SST score was 11.5 points (range, 9-12 points) and mean ACJI score was 84.7 points (range, 62-98 points) for the entire group. For pain items patients reached 17.1 points (range, 0-20 points), for Activities of Daily Living (ADL) 9.6 points (range, 5-10 points), for cosmesis 7.6 points (range, 0-10 points), for function 23.1 points (range, 10-25 points) and for radiological assessment, 24.5 points (range, 4-25 points). Return to contact sports was allowed 6 months after the surgical procedure. One patient showed an elongation of the sutures, with a stable but dislocated joint. In this case, a new surgery of the AC-joint was not required. There was no migration or dislocation of the implants at the last FU (Fig. 3).
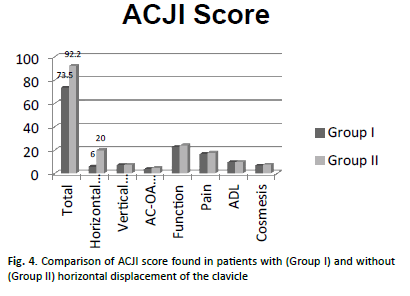
Fifty patients (58.1%) did not show postoperative horizontal displacement in the Alexander view and had a mean ACJI score of 92.2 points (range, 68-98 points). Thirty-six patients (41.9%) presented some degree of horizontal postoperative displacement (subluxation or dislocation) of the AC-joint in the Alexander view. They had a mean ACJI score of 73.5 points (range, 61-85 points). This difference was statistically significant (p<0.001). The subcategories of the ACJI scoring system for these two groups are compared in Fig. 4.
Discussion
Surgical treatment of acute AC-joint dislocation has a large number of techniques and normally all of them can achieve a satisfactory rate, but until now there is no reported gold standard. Many techniques result in difficulties, e.g. fracture of the coracoid, loosening of the implants, breakage and/or migration of the hardware, loss of reduction and postoperative osteoarthritis [11,12,26,27].
Recent biomechanical studies have described that an anatomical reconstruction of the CC ligaments could lead to better clinical outcomes [10,28]. Beitzel et al. found a significantly higher load to failure for superior translation, less translation in all 3 directions and higher superior stability when comparing reconstruction of the AC-joint with single or double clavicular tunnels using suture pulley and 2 or 3 buttons versus modified Weaver Dunn reconstruction [28]. Therefore, new surgical techniques have been described using biological [3,20,29,30] and non-biological [10,19,22-24] materials to anatomically reconstruct the CC ligaments. However, it is not yet clear if these techniques will have any clinical advantage [30].
Two studies, with over 2 years of FU, have presented the clinical results of the reconstruction of acute AC joint dislocation using the double Tight Rope technique. Salzmann et al. after a mean FU of 30.6 months, reported the results of 23 patients (3 Rockwood type III, 3 Rockwood type IV and 17 Rockwood type V). The mean Constant Score (CS) was 94.3 points (range, 88-98 points). They had 8 patients with unsatisfactory radiological outcomes. There were 3 complications that were further examined surgically: one coracoid fracture, one slip of the medial coracoid button associated to vertical instability and one superficial infection at 6 months follow-up [22].
Scheibel et al. presented the outcomes for 28 out of 37 patients with a Rockwood type V AC-joint dislocation, operated on with double Tight Rope arthroscopically and radiologically assisted ACjoint reconstruction. Mean age was 38.8 years (18-66 years), average FU 26.5 months (20.1-32.8 months), mean CS 91.5 points (84-100), mean subjective shoulder value was 95.1% (85%-100%) and the mean Taft score was 10.5 points (7-12). They also introduced a new evaluation tool, the ACJI score, to attenuate the overestimation of the rate of success after surgical reconstruction of the AC-joint. In fact, this score seems to be a more specific tool to evaluate AC-joint dislocation outcomes than the previously reported Taft score, because it considers different categories such as subjective degree of satisfaction, clinical objective parameters and radiological measurements [23].
The ACJI score is currently being validated but could be a more comprehensive and specific tool than other shoulder scores used in the literature. The mean ACJI score for Scheibel et al. series was 79.9 points (84-100 points). In their study, the CC distance at the last FU was 13.6 mm (5 mm-27 mm) on the operated side, versus 9.4 mm (4 mm- 15 mm) on the contralateral side (p<0.05). They found postoperative posterior displacement of the clavicle in the Alexander view in 42.9% of cases. These patients had significantly inferior results in the Taft and ACJI scores (p<0.05). Unlike these patients, they did not find significant differences between patients with some degree of vertical displacement versus those without displacement in the AP view. Twenty-five (89.3%) patients had implant migration. Seventeen (60.7%) had a mild migration to the level of the superior cortex of the clavicle; 8 patients presented migration of both buttons, one at least migrated completely into the clavicle or into the coracoid. They did not find a significant difference between migration of the medial and lateral buttons, neither a correlation between implant migration and CC distance [23].
In our study, the mean ACJI score was 84.7 points (range 62-98 points) for the entire group at a mean of 24.2 months (12-32 months) of FU. The mean SST was 11.5 points.
These clinical outcomes are comparable with the results from both of the studies previously described [22,23]. We did not find a significant loss of reduction in the vertical plane when we compared the CC distance in the immediate postoperative radiographies with the last FU radiographies. On the other hand, we found that 41.9% of our patients had some degree of displacement of the clavicle in the horizontal plane in the radiological evaluation, who displayed a significantly lower ACJI score. These results were also reported by Scheibel et al. [23]. There were no statistic differences between all other parameters from both groups of patients, with and without horizontal displacement of the clavicle. Although horizontal postoperative instability is relevant, all of our patients pointed good and excellent in the subjective and objective items (e.g. strength and range of motion). No patients showed dislocation or migration of the implants [31].
Our study suggests that the ACJI score may overestimate horizontal displacement of the clavicle under stress, in the postoperative Alexander view, misleading the interpretation of the specialist. This study also suggests that attention should be emphasized on the function and strength of patients, as well as on subjective outcomes rather than on radiological FU. Among the strengths of this study we highlight the evaluation of a homogeneous cohort of patients with high degree (Rockwood V) AC-joint dislocations, operated on within 5 days after trauma as part of a prospective study with an adequate number of patients and FU. We are conscious that our study does not have a control group and that the FU period is relatively short.
Conclusion
The surgical management of patients with an acute high degree of AC-joint dislocation using double-button device provides a stable fixation and the hardware does not need to be removed. This technique shows satisfactory subjective results, such as cosmesis and activities of daily living, as well as objective parameters like the strength and range of motion at the intermediate-term FU. The future studies regarding AC-joint dislocation will need to focus on diagnosis, evaluation and management of horizontal instability considering there is no consensus in surgical treatment strategies for this group of patients.
Level of Evidence
Level 3
Funding
NoConflict of Interest
None
Ethical Responsibilities
Protection of people and animals. The authors state that no experiments have been conducted on humans or animals for this research.
Confidentiality of data. The authors state that they have followed their workplace protocols on publishing patient data.
Right to privacy and informed consent. The authors state that this article does not contain patient data.
REFERENCES
- Flik K., Lyman S., Marx RG.: American Collegiate men’s ice hockey: an analysis of injuries. Am J Sports Med. 2005;33:183-187.
- Lemos M.J.: The evaluation and treatment of the injured acromioclavicular joint in athletes. Am J Sports Med. 1998;26:137-144.
- Costic R.S., Labriola J.E., Rodosky M.W., et al.: Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32:1929-1936.
- Cadenat F.: The treatment of dislocations and fractures of the outer end of the clavicle. Int Clin. 1917;1:145-169.
- Rockwood C.A. Jr.: Injuries to the acromioclavicular joint, in Rockwood CA Jr, Green DP (eds): Fractures in Adults. Volume 1. Second edition. Philadelphia, JB Lippincott, 1984:860-910, 974-982.
- Rockwood C.A. Jr.: Disorders of the acromioclavicular joint. In: Rockwood CA Jr, Matsen III FA, (eds): The shoulder, vol. I Philadephia, PA: WB Saunders. 1990:413-476.
- Bradley J.P., Elkousy H.: Decision making: operative versus nonoperative treatment of acromioclavicular joint injuries. Clin Sports Med. 2003;22:277-290.
- Guy D.K., Wirth M.A., Griffin J.L., et al.: Reconstruction of chronic and complete dislocations of the acromioclavicular joint. Clin Orthop Relat Res. 1998;347:138-149.
- MacDonald P.B., Alexander M.J., Frejuk J., et al.: Comprehensive functional analysis of shoulder following complete acromioclavicular separation. Am J Sports Med. 1988;16:475-480.
- Spencer E.E.: Treatment of grade III acromioclavicular joint injuries: a systematic review. Clin Orthop Relat Res 2007;455:38-44.
- Guttmann D., Paksima N.E., Zuckerman J.D.: Complications of treatment of complete acromioclavicular joint dislocations. Instr Course Lect. 2000;49:407-413.
- Hoffler C.E., Karas S.G.: Transarticular erosion of a locked subacromial hook plate: case report and review of literature. J Shoulder Elbow Surg. 2010;19:e12-e15.
- Baumgarten K.M., Altchek D.W., Cordasco F.A.: Arthroscopically assisted acromioclavicular joint reconstruction. Arthroscopy. 2006;22:228.e1-228.e6.
- Breslow M.J., Jazrawi L.M., Bernstein A.D., et al.: Treatment of acromioclavicular joint separation: suture or suture anchors? J Shoulder Elbow Surg. 2002;11:225-229.
- Fukuda K., Craig E.V., An K.N., et al.: Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986;68:434-440.
- Harris R.I., Wallace A.L., Harper G.D., et al.: Structural properties of the intact and the reconstructed coracoclavicular ligament complex. Am J Sports Med. 2000;28:103-108.
- Hubble M.J., Bannister G.C.: A new drill guide to simplify coraco-clavicular screw fixation. Injury. 1995;26:572-573.
- Lafosse L., Baier G.P., Leuzinger J.: Arthroscopic treatment of acute and chronic acromioclavicular joint dislocation. Arthroscopy. 2005;21:1017.e1-1017.e8.
- Lim Y.W.: Triple endobutton technique in acromioclavicular joint reduction and reconstruction. Ann Acad Med Singap. 2008;37:294-299.
- Mazzocca A.D., Santangelo S.A., Johnson S.T., et al.: A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34:236-246.
- Rios C.G., Arciero R.A., Mazzocca A.D.: Anatomy of the clavicle and coracoid process for reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2007;35:811-817.
- Salzmann G.M., Walz L., Buchmann S., et al.: Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med. 2010;38:1179-1187.
- Scheibel M., Dröschel S., Gerhardt C., et al.: Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39:1507-1516.
- Xue C., Song L.J., Zhang H., et al.: Truly anatomic coracoclavicular ligament reconstruction with 2 Endobutton devices for acute Rockwood type V acromioclavicular joint dislocations. J Shoulder Elbow Surg. 2018;27:e196-e202.
- Lippitt S.B., Harryman D.T. II, Matsen F.A. III.: A practical tool for evaluation of function: the simple shoulder test. In Matsen FA III, Fu FH, Hawkins RJ [eds]: The Shoulder: A balance of mobility and stability. Rosemont IL: American Academy of Orthopaedic Surgeons. 1993:501-518.
- Chiang C.L., Yang S.W., Tsai M.Y., et al.: Acromion osteolysis and fracture after hook plate fixation for acromioclavicular joint dislocation: a case report. J Shoulder Elbow Surg. 2010;19:e13-e15.
- Defoort S., Verborgt O.: Functional and radiological outcome after arthroscopic and open acromioclavicular stabilization using a double-button fixation system. Acta Orthop Belg. 2010;76:585-591.
- Beitzel K., Obopilwe E., Chowaniec D.M., et al.: Biomechanical properties of repairs for dislocated AC joints using suture button systems with integrated tendon augmentation. Knee Surg Sports Traumatol Arthrosc. 2012;20:1931-1938.
- Shin S.J., Yun Y.H., Yoo J.D.: Coracoclavicular ligament reconstruction for acromioclavicular dislocation using 2 suture anchors and coracoacromial ligament transfer. Am J Sports Med. 2009;37:346-351.
- Yoo Y.S., Tsai A.G., Ranawat A.S., et al.: A biomechanical analysis of the native coracoclavicular ligaments and their influence on a new reconstruction using a coracoid tunnel and free tendon graft. Arthroscopy. 2010;26:1153-1161.
- Aliberti G.M., Kraeutler M.J., Trojan J.D.: Horizontal instability of the acromioclavicular joint. A systematic review. Am J Sports Med. 2020;48:504-510.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.