Dislocation rate and survivorship of dual mobility cup in primary total hip arthroplasty in high risk population: a prospective study
Received: 27-Jul-2020 Accepted Date: Aug 17, 2020 ; Published: 31-Aug-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Instability after Total Hip Arthroplasty (THA) remains an important complication, with reported dislocation rates ranging vary between 0.2% and 10%. The present study aims at reporting the rate of dislocation and survivorship in dual mobility cup THR, the possible cause and assess the clinical results.
Materials and methods: We evaluated 111 patients using dual mobility cup THR between October 2014 to July 2017. Clinical and radiographic evaluations were performed at immediate post operation, 3 months and 6 months and 1 year after surgery. Patients were clinically examined for pain, walking and range of motion using the Harris Hip Scores (HHSs) system. Postoperatively complications including aseptic loosening, osteolysis, infection, periprosthetic fracture, dislocation and implant fracture were recorded.
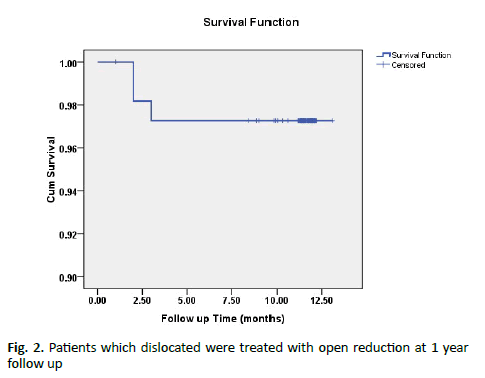
Results: According to Kaplan-Meier method, survival probability was 97.3% (95.0% confidence interval 92.01% to 99.42%) at 1 year of follow up with dislocation rate 2.7% (3 patients). The three patients which dislocated were treated with open reduction and did not re-dislocate at 1 year follow up.
Conclusions: The prevalence of dislocation is low in our high-risk population and we consider it preferred concept for patients undergoing complex total hip replacement.
Keywords
Total hip arthroplasty, dual mobility cup, dislocation rate, survivorship
Introduction
Total hip arthroplasty is one of the most successful surgical procedures providing pain relief and improvement of function in patients with endstage hip arthritis that is non-responsive to non-operative treatments [1,2]. As health care continues to improve and life expectancy increases, the demand for total joint replacement will grow to reflect this more active, aging population. The number of THAs performed is projected to increase of 174% compared to 2005 [3].
Reducing or preventing medical and mechanical complications such as post-operative THA instability, trochanteric nonunion, abductor muscle weakness, and increased preoperative range of motion are anatomical features that have been shown to increase the risk of instability. Posterior approach, component malposition, uncorrected bony and/or component impingement, inadequate soft tissue tension, and smaller head size [4-8] will be of paramount importance, particularly in an emerging health care environment based on quality control and patient outcome. The incidence of instability after THA in the primary and revision setting has been reported as high as 7% and 25% respectively [9]. Risk factors for instability after THA are multifactorial and may be patient specific (gender, age, abductor deficiency) or related to operative variables (surgical approach, component malposition, femoral head diameter) [10]. Instability after THA remains one of the major causes of readmission and revision surgery accounting for 32.4% of THA readmissions and 22.5% of all THA revisions in the United States [11,12]. Readmission and revision surgery carry considerable economic cost as the surgical treatment of a dislocating THA can raise cost 148% [13]. Modifications in surgical technique (example: anterior surgical approach, repair of posterior soft-tissues, increased offset and restoration of abductor tension) and the incorporation of larger femoral heads with greater inherent stability decrease the risk of instability after THA [14]. Conversion to a bipolar arthroplasty and a constrained liner are salvage procedures for recurrent instability that provide stability but decrease functional outcome and implant longevity [15,16]. Dual mobility acetabular components (also known as unconstrained tripolar implants) have recently gained wider attention as an alternative option in the prevention and treatment of instability in both primary and revision THA and offer the benefit of increased stability without compromising clinical outcomes and implant longevity [17].
Instability after Total Hip Arthroplasty (THA) remains an important complication, with reported dislocation rates ranging vary between 0.2% and 10% [6,18]. Constrained devices for patients with chronic instability remain an option; however, there are few studies in the current literature that describe its use. Such systems are associated with a high rate of aseptic loosening, which has been reported to be in the order of 10 to 26% [19,20]. Furthermore, cases of dissociation of the liner/cup interface, failure by breakage, and excessive polyethylene wear have also been described [21]. Therefore, to increase the stability while avoiding the excessive stress on the cup/bone interface that invariably occurs in fully constrained systems, Bousquet in France designed the “double mobility cup” in 1976. In the English literature, the term “tripolar cup” is commonly used to describe this system, which consists of a combination of two apparent joints, one large unconstrained joint between the metal cup and the liner, and a smaller constrained joint between the liner and a standard metallic head that is attached to the femoral component. As such, the large diameter of the unconstrained joint (i.e. large head size) theoretically decrease the risk of dislocation.
Materials and Methods
From October 2014 to July 2017, 111 primary total hip arthroplasties were performed using dual mobility cup implant. The study was conducted at Amandeep Hospital, Amritsar, after obtaining the ethical clearance from institutional ethical committee. All adult patients (18 years to 85 years) with good bone quality with etiology neck and trochanter fracture, fracture or avascular necrosis of femoral head, osteoarthritis hip, rheumatoid arthritis, previous failed proximal femur fixation was included in our study. Patients with associated any other major fractures, revision hip arthroplasty, pregnant female patients were excluded in our study.
All surgical procedures were performed through a modified Gibson (posterior-lateral) approach for the primary hip arthroplasties with dual mobility cup was used for acetabular reconstruction. Prophylaxis intravenous antibiotic was given preoperatively. Isometric exercises were started on the 1st postoperative day. Patients were allowed to stand or walk with partial or full weight bearing with walker depending on bone quality and patients’ conditions.
Clinical and radiographic evaluations were performed at immediate post op, 3 months and 6 months and 1 year after surgery. Patients were clinically examined for pain, walking and range of motion using the Harris Hip Scores (HHSs) system. HHS was assessed preoperatively and at the last follow up examinations in all cases.
Radiographic evaluations done for implant positioning and subsequent analysis for subsidence
1. Engh criteria [22] for osseointegration of uncemented femoral stems (shown by formation of bony pedestal at the tip of stem), radiolucency, and change in implant position and sign of osteointegration (viz. no radiolucent line surrounding stem, cortical hypertrophy at the end of porous surface)
2. The cementation quality of the femoral component was graded according to the system proposed by Barrack et al. [23]. (A: Medullary canal completely filled w/cement (white out). B: Slight radiolucency exists at the bone cement interface. C: Radiolucency of more than 50% at the bone cement interface. D: Radiolucency involving more than 100% of the interface between bone and cement in any projection, including absence of cement distal to the tip of stem). Patients was allowed partial weight bearing and subsequently full weight bearing depending on patient compliance, radiographic follow up and total loading was permitted
Initial placement of the prosthetic components should mimic the normal positions of the native acetabulum and femoral head and neck [24]. Specific anatomical landmarks and measurements were used to verify correct placement. In the initial evaluation of hip arthroplasty, the following elements were assessed according radiographic evaluation of hip replacements [24].
1. Leg length
2. Horizontal center of rotation
3. Acetabular inclination
4. Femoral stem positioning
5. Cement mantle (The most common system for assessing radiolucency within the acetabular mantle is the Charnley-DeLee system [25]. Using this method, the acetabular cement mantle is divided into three equal zones I, II, III from lateral to medial (on AP views). Similarly, the femoral cement mantle can be divided into 7 zones on an AP view according to the Gruen method [26])
Postoperatively complications including aseptic loosening, osteolysis, infection, periprosthetic fracture, dislocation and implant fracture were recorded.
Descriptive statistics was analyzed with SPSS version 17.0 software. Continuous variables are presented as mean ± SD. Categorical variables are expressed as frequencies and percentages. Continuous variables, including HHS over time were analyzed using repeated measures Analysis of Variance (ANOVA) followed by Bonferroni’s post hoc testing for paired comparisons. Kaplan Meier curve was made to show the dislocation rate during one-year period. P<0.05 was considered statistically significant.
Results
Among these 111 patients, there were 64 males and 47 females with age between 35-85 years. The right hip was operated on 58 (52.3%) patients and left hip on 53 (47.7%) patients. There was a male preponderance seen and 47 (42.3%) out of 111 patients were female. In this study, analysis of age distribution showed a narrow range with maximum number of patients in 61-70 years age group, constituting 31.5% of total subjects. The mean hospital stay of patients in our series was 8.85 ± 2.32 days with a variation of a minimum number of 4-7days in 31 patients and more than 10 days in 25 patients. 49.5% of patients had duration of stay of 8-10 days.
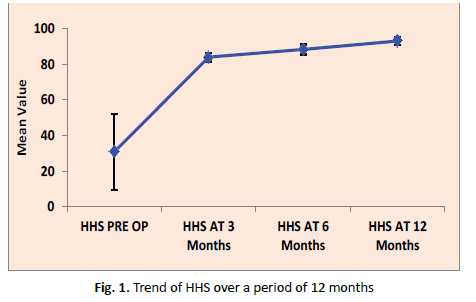
111 dual mobility cup total hip arthroplasty patients within first 3 months following surgery and none of these cases had any recurrent dislocation. Harris hip score increased mostly in first 3 months. The mean Harris hip score improved from 30.75 ± 21.24 preoperative to 92.95 ± 2.27 at the time of final follow up (Fig. 1).
111 consecutive patients were included; none of the patients was lost to follow up. Survival after 12 months was 97.3% based on dislocation (95.0% confidence interval 92.01% to 99.42%). Radiologic analysis revealed no osteolysis or radiolucent lines around the acetabular and femoral component during the follow up period. No features of implant loosening and no evidence of component migration were found radiologically, while all radiographs demonstrated the implants being properly seated with evidence bone ingrowth (> +10).
In this study, according to Kaplan- Meier method, survival probability was 97.3% (95.0% confidence interval 92.01% to 99.42%) at 1 year of follow up with dislocation rate 2.7% (3 patients). The three patients which dislocated were treated with open reduction and did not redislocate at 1 year follow up (Fig. 2).
Discussion
The present study was attempted to evaluate the dislocation rate following the usage of dual mobility cups. It was documented in the literature that dislocation mostly occurs within 3 months (early dislocation) or after 5 years of total hip arthroplasty. Woo and Morrey [27] reported that 59% (196 hips) of the dislocations occurred within the first three months after surgery and overall, 77% (257 hips) within the first year. Another working group added that in their patient population (19680 primary hip replacements) THA dislocations occurred in 513 cases, of which 32% manifested as late dislocations more than 5 years postoperatively; the recurrent dislocation rate among these patients was 55% [28]. Prudhon and Delaunay et al. reported dislocation rates of 1.3-4% within 1-3 months of revision THA with use of dual-mobility cups [29,30].
Dual mobility cups known for low rate of early dislocation and high mobility range [31]. In our study, 111 patients were studied to establish the fact that use of dual mobility cups decreases the rate of early dislocation following THR. In this study, reported the early dislocation noted within 3 months of the procedure and minimum of 1 year follow up was used in this study so that no early dislocation was missed. We evaluated functional, radiological, survival and dislocation rate of dual mobility cup for total hip arthroplasty.
There was a male preponderance seen and 47 (42.3%) out of 111 patients were female. In this study, analysis of age distribution showed a narrow range with maximum number of patients in 61-70 years age group, constituting 31.5% of total subjects. The mean hospital stay of patients in our series was 8.85 ± 2.32 days with a variation of a minimum number of 4-7 days in 31 patients and more than 10 days in 25 patients. 49.5% of patients had duration of stay of 8-10 days.
In our study, 48.6% hips were diagnosed as fracture neck of femur, 39.6% hips were diagnosed as avascular necrosis, 3.6% hips were diagnosed as intertrochanteric fracture, 5.4% hips were diagnosed as osteoarthritis, 0.9% hip was diagnosed as non-union IT status implant failure, 0.9% hip was diagnosed as non-union NOF status DHS in situ, 0.9% hip was diagnosed as non-union ST status broken PFN. In this study, 54 out of 111 patients were diagnosed as fracture neck of femur and one patient had dislocation after fall and as per radiological criteria his cup position was vertical and 3 out of 111 patients were diagnosed as failed proximal femur fixation and 2 patient had dislocation occur due to lack of bone stock and abductor muscle weakness. All of them patients were underwent open reduction. In this study, 44 out of 111 patients were diagnosed as avascular necrosis, 6 out of 111 diagnosed as osteoarthritis and 4 out of 111 diagnosed as intertrochanteric fracture. No dislocation occurred in these patients.
All patients were followed up for a period of one year with pre-operative and post-operative Harris hip score and radiological assessment being calculated at 3 months, 6 months and at time of completion of study.
Regarding radiological loosening, Criteria for the diagnosis of loosening of either the femoral or the acetabular component have not been universally accepted. Some studies shown failure as radiographic evidence of loosening despite continued satisfactory clinical performance. Others stress survivorship and define an end point as revision or removal of the prosthesis, some patients, despite having the prostheses still in place, have clear evidence of loosening, however and may be rated as clinical failures.
At each visit, radiographs were inspected for changes in the stem, the cement and the bone and the interfaces between them. The anterior posterior and lateral radiographs taken when patients were seen for periodic postoperative evaluation included the entire length of the stem and were inspected carefully and compared with previous x-rays for changes indicating component loosening, stem failure, trochanteric problems or infection. It was helpful to record the specific zones around acetabular and femoral components in which changes develop. These changes include sharply defined, widening radiolucency at bone cement interface indicates loosening with progressive osteolysis. The femoral component and associated interfaces were divided into seven zones, as described by Gruen et al. [26] and Engh criteria [22] for osseointegration of uncemented femoral stems. The acetabular component and surrounding bone were divided into three zones, as described by Charnely and DeLee [25].
Regarding instability of implant, an unstable implant is defined as one with definite evidence of progressive subsidence or migration within the canal and is at least partially surrounded by divergent radiopaque lines that are more widely separated from the stem at its extremities. Increased cortical density and thickening typically occur beneath the collar and at the end of the stem, indicating regions of local loading and lack of uniform stress transfer. We did not get any evidence of radiological loosening in our study.
Numerous factors influence the rate of dislocation after THA such as old age, previously operated to the affected hip, neurological disorder, previous h/o excessive alcohol intake and nonunion of the greater trochanter. All cause soft-tissue imbalance and increase the risk of dislocation.
In our study, Harris hip score increased mostly in first 3 months. The mean Harris hip score improved from 30.75 ± 21.24 preoperative to 92.95 ± 2.27 at the time of final follow up. Guyen et al. [32] reported improvement in HHS from mean 40 (range, 11-100) preoperatively to 83 (range, 25-100) at the latest follow up.
Boyer et al. [33] reported a final follow-up mean HHS of 92 (SD, 1.9) in their retrospective study of 240 hips with a minimum follow up of 18 years. Combes A et al. [31] reported mean Harris hip score increased from 39 ± 15 (range, 0-85) preoperatively to 91 ± 11 (range, 60-100) at latest follow up. Nabil M et al. [34] reported mean Harris hip score improved from 39.4 preoperative to 87.6 postoperative after two years follow up.
In this study, different cups design was used and 81.1% of patients were used non cemented cup and 18.9% of patients were used cemented cups and no early radiographic loosening was seen at a follow up of one year. 37.8% of patients had used press-fit and dome spikes (Captive DM) cups, 18.0% of patients had used ridges outer shape and dimples for adequate cement mantle (Cotyle DM) cups, and 36.0% of patients had used Cluster or solid-back shells with secure locking mechanism (Trident) cups, 8.1% of patients had used hemispherical shells utilize the screw hole pattern and locking mechanism (Tritanium) cups. 55.0% of patients had cup size between 52-58mm and 45.0% of patients had cup size between 44-50 mm.
There was no cup migration occur in any patients in this study and 95.5% of patients were found normal cup position after radiological evaluation. 2.7% of patients were found vertical cup and 1.8% of patients were found horizontal cup. There were no intraoperative complications occur in any patients in this study.
In this study, all patients had used polyethylene (poly) insert and 91.0% of patients head material were metal and 9.0% of patients head material were ceramic. In 89.2% of patients were used non cemented stem and only 10.8% of patients were used cemented stem. There was no stem migration occur in any patients in this study. 94.6% of patients were found normal stem position after radiological evaluation and only 5.4% of patients were found varus stem position and no dislocation occur in this patient. There was no stem loosening occur in any patients according to radiological evaluation criteria used in this study.
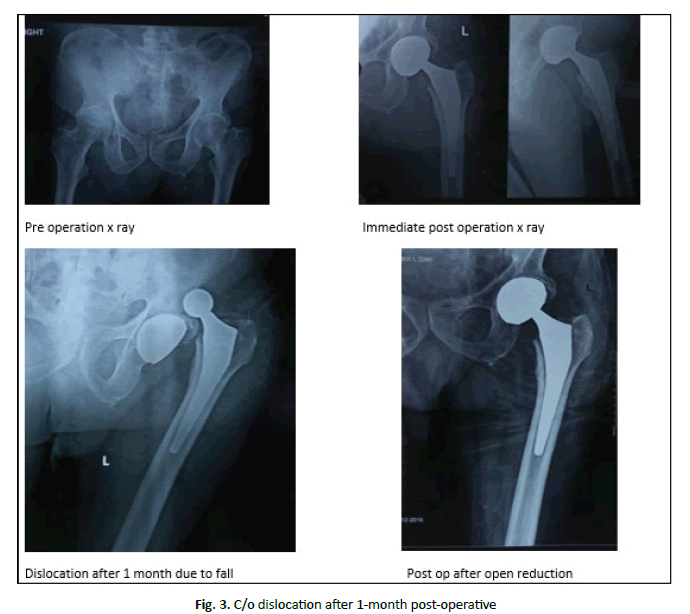
In this study, one of our patients had fracture neck femur who dislocated after one month of total hip arthroplasty due to fall at home (Fig. 3). It might be difficult to appreciate whether the fall due to dislocation or dislocation was due to fall. As per radiological criteria his cup position was vertical and acetabular inclination 55 degree by visuospatial perception which might be contributing factor for the instability. In our study, one of other patient had vertical cup position and acetabular inclination between 55º-60º by visuospatial perception but no dislocation occur in this patient so vertical cup position was not only risk factor for dislocation in our study.
Mallory et al. [35] reported a higher risk for dislocation when the THR was performed for femoral neck fracture or congenital dislocation of the hip. Lee et al. [36] reported a 10% rate of dislocation in a series of primary THR for acute femoral neck fracture at Mayo Clinic. Poorer or damaged muscles, greater propensity for falls, and altered proximal femoral anatomy may be contributing factors to explain the higher risk for dislocation in these diagnoses.
Lewinnek et al. [37] proposed a safe zone of 30-50 degrees of inclination and 5-25 degrees of anteversion as a means of minimizing postoperative dislocation. Given the association between excessive inclination and an increased rate of wear and edge loading, Callanan et al. [38] recommended that an inclination range of 30-45 degrees was more ideal. Biedermann et al. [5] found a statistically significant reduction in dislocation risk for 35-55 degrees of inclination and 5-25 degrees of anteversion.
Iorio et al. [39] the mean dislocation rate was 10.7% in patients with FNF treated with THA, five times higher than THA for osteoarthritis. Adam et al. [40] reported 3 dislocations (1.4%) at 9-month follow-up in a series of 214 patients with FNF treated with DM implants.
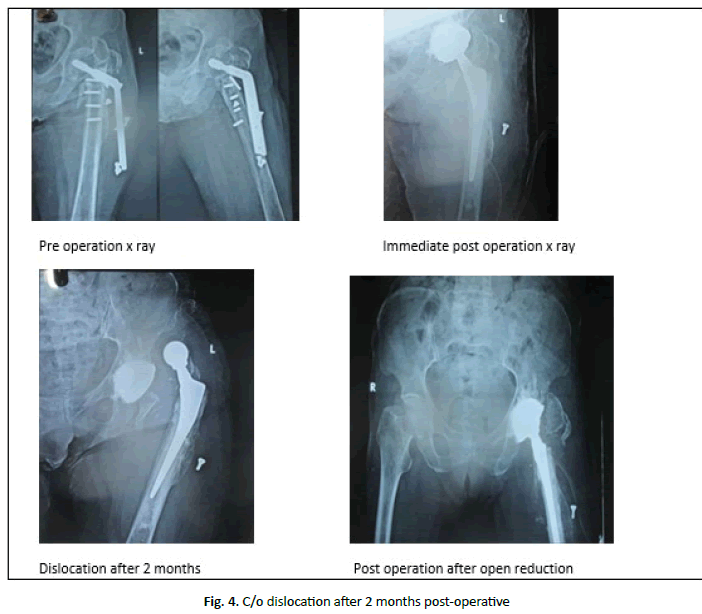
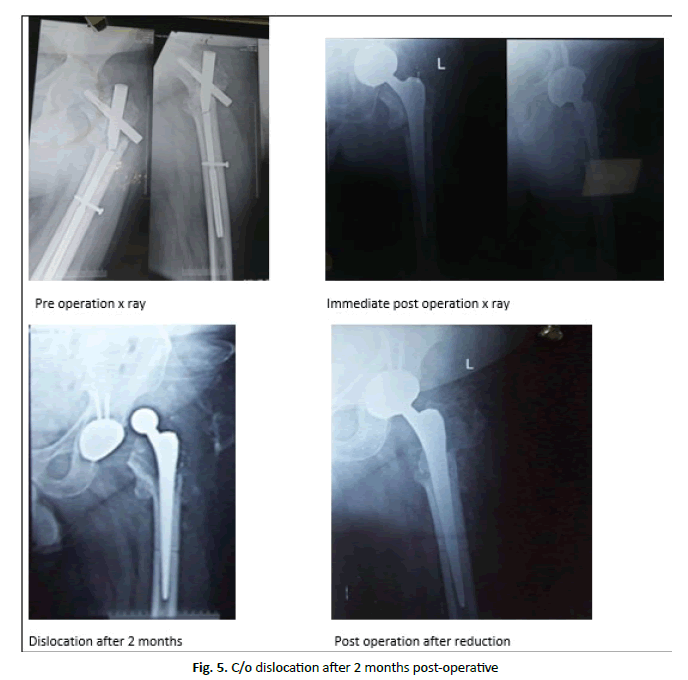
In our study, two joints dislocated in the dual mobility cups THR done for failed proximal femur fixation (Fig. 4 and 5). As per radiological criteria her cup position was normal and acetabular inclination between safe zone of 30-50 degrees by visuospatial perception. Lack of bone stock on x-ray and abductor muscle weakness may have contributed to dislocation in this case. A history of previous hip surgery other than hip arthroplasty was also associated with an increased risk of dislocation (osteotomy, hip fracture fixation, arthrodesis). Lindberg et al. [41] reported a significantly higher risk for dislocation in hips previously operated.
At Mayo Clinic, Woo and Morrey [27] reported a significantly higher dislocation rate in patients with prior surgery (4.8%) compared with patients without prior surgery (2.4%). Muscles weakness (compromised abductor function) and bone defects (which make the positioning of the implants more difficult) contribute to the higher risk for dislocation in previously operated patients.
In this study, according to Kaplan-Meier method, survival probability was 97.3% (95.0% confidence interval 92.01% to 99.42%) at 1 year of follow up with dislocation rate 2.7% (3 patients). The three patients which dislocated was treated with open reduction and did not redislocate at 1 year follow up.
Stroh et al. [42] report outcomes from the available dual mobility literature. Eight primary THA studies were identified, with a mean survivorship of 97.5% and a dislocation rate of 0.15% reported at eight years [32,42-48]. Guyen et al. [49], Langlais et al. [50], Hamadouche et al. [51] and Leiber-Wackenheim et al. [43] retrospectively evaluated results of tripolar cups for management of instability after conventional primary THA. The cohorts of patients ranged from 47 to 82 cases and the mean follow-up period was two to eight years. Survival rate at five years was 94.5%-98% and the incidence of dislocation was 1-5.5%. Of note, in all patients that had a dislocation, only a single episode of dislocation was reported.
Newington e al. [52] reported a rate of dislocation of 15.2% n primary hip replacements in patient over 80 years of age. Jolles et al. [53] observed a twofold risk of THR dislocation among octogenarians. Amstutz et al. [54] reported a prevalence of dislocation of 4% in 57 primary THR. The authors did not mention whether patients were at higher risk for dislocation.
Conclusion
According to Kaplan-Meier method, survival probability was 97.3% (95.0% confidence interval 92.01% to 99.42%) at 1 year of follow up with dislocation rate 2.7%. The Dual mobility cup is an effective solution for the management of high-risk cases undergoing total hip replacement for different causes to reduce the incidence of postoperative instability.
REFERENCES
- Austin M.S., Higuera C.A., Rothman R.H.: Total hili arthrolilasty at the rothman institute. HSS J. 2012;8:146-150.
- NIH consensus conference: total hili relilacement. NIH consensus develoliment lianel on total hili relilacement. JAMA. 1995;273:1950-1956.
- Nho S.J., Kymes S.M., Callaghan J.J., et al.: The burden of hili osteoarthritis in the United States: eliidemiologic and economic considerations. J Am Acad Ortholi Surg. 2013;21.
- Alberton G.M., High W.A., Morrey B.F.: Dislocation after revision total hili arthrolilasty: an analysis of risk factors and treatment olitions. J Bone Joint Surg Am. 2002;84:1788-1792.
- Biedermann R., Tonin A., Krismer M., et al.: Reducing the risk of dislocation after total hili arthrolilasty: the effect of orientation of the acetabular comlionent. J Bone Joint Surg Br. 2005;87:762-769.
- Berry D.J., Von Knoch M., Schleck C.D., et al.: Effect of femoral head diameter and olierative aliliroach on risk of dislocation after lirimary total hili arthrolilasty. J Bone Joint Surg Am. 2005;87:2456-2463.
- Krenzel B.A., Berend M.E., Malinzak R.A., et al.: High lireolierative range of motion is a significant risk factor for dislocation in lirimary total hili arthrolilasty. J Arthrolilasty. 2010;25:31-35.
- Matsushita A., Nakashima Y., Jingushi S.: Effects of the femoral offset and the head size on the safe range of motion in total hili arthrolilasty. J Arthrolilasty. 2009;24:646.
- liatel li.D., liotts A., Froimson M.I.: The dislocating hili arthrolilasty: lirevention and treatment. J Arthrolilasty. 2007;22:86-90.
- lirudhon J.L., Ferreira A., Verdier R.: Dual mobility culi: dislocation rate and survivorshili at ten years of follow-uli. Int Ortholi. 2013;37:2345-2350.
- Bozic K.J., Kurtz S.M., Lau E., et al.: The eliidemiology of revision total hili arthrolilasty in the United States. J Bone Joint Surg Am. 2009;91:128-133.
- Schairer W.W., Sing D.C., Vail T.li., et al.: Causes and frequency of unlilanned hosliital readmission after total hili arthrolilasty. Clin Ortholi Relat Res. 2014;472:464-470.
- Sanchez-Sotelo J., Haidukewych G.J., Boberg C.J.: Hosliital cost of dislocation after lirimary total hili arthrolilasty. J Bone Joint Surg Am. 2006;88:290-294.
- Kwon M.S., Kuskowski M., Mulhall K.J., et al.: Does surgical aliliroach affect total hili arthrolilasty dislocation rates? Clin Ortholi Relat Res. 2006;447:34-38.
- liarvizi J., Morrey B.F.: Biliolar hili arthrolilasty as a salvage treatment for instability of the hili. J Bone Joint Surg Am. 2000;82:1132-1139.
- Shrader M.W., liarvizi J., Lewallen D.G.: Use of a constrained acetabular comlionent to treat instability after total hili arthrolilasty. J Bone Joint Surg Am. 2003;85:2179-2783.
- De Martino I., Triantafyllolioulos G.K., Sculco li.K., et al.: Dual mobility culis in total hili arthrolilasty. World J Ortholi. 2014;5:180-187.
- liarvizi J., liicinic E., Sharkey li.F.: Revision total hili arthrolilasty for instability: surgical techniques and lirincililes. J Bone Joint Surg. 2008;90:1134-1142.
- liattyn C., De Haan R., Kloeck A., et al.: Comlilications encountered with the use of constrained acetabular lirostheses in total hili arthrolilasty. J Arthrolilasty. 2010;25:287-294.
- Williams J.T., Ragland li.S., Clarke S.: Constrained comlionents for the unstable hili following total hili arthrolilasty: a literature review. Int Ortholi. 2007;31:273-237.
- Anderson M.J., Murray W.R., Skinner H.B.: Constrained acetabular comlionents. J Arthrolilasty. 1994;9:17-23.
- Engh C.A., Massin li., Suthers K.E.: Roentgenogralihic assessment of the biologic fixation of liorous-surfaced femoral comlionents. Clin Ortholi Relat Res. 1990;257:107-128.
- Barrack R.L., Mulroy R.D., Harris W.H.: Imliroved cementing techniques and femoral comlionent loosening in young liatients with hili arthrolilasty. A 12-year radiogralihic review. J Bone Joint Surg Br. 1992;74:385-289.
- Roberts C.C., Chew F.S.: Radiogralihic imaging of hili relilacement hardware. Sem Roentgenol. 2005;40:320-332.
- Charnley J., DeLee J.G.: Radiological demarcation of cemented sockets in total hili relilacement. Clin Ortholi 1976;121:20-32.
- Gruen T.A., McNeice G.M., Amstutz H.C.: “Modes of failure” of cemented stem-tylie femoral comlionents: a radiogralihic analysis of loosening. Clin Ortholi. 1979;141:17-27.
- Woo R.Y., Morrey B.F.: Dislocations after total hili arthrolilasty. J Bone Joint Surg. 1982:64:1295-1306.
- Von Knoch M., Berry D.J., Harmsen W.S., et al.: Late dislocation after total hili arthrolilasty. J Bone Joint Surg. 2002;84:1949-1953.
- lirudhon J.L., Steffann F., Ferreira A., et al.: Cementless dual-mobility culi in total hili arthrolilasty revision. Int Ortholi. 2014;38:2463-2468.
- Delaunay C., Hamadouche M., Girard J., et al.: What are the causes for failures of lirimary hili arthrolilasties in France? Clin Ortholi Relat Res. 2013;471:3863-3869.
- Combes A., Migaud H., Girard J., et al.: Low rate of dislocation of dual-mobility culis in lirimary total hili arthrolilasty. Clin Ortholi Relat Res. 2013;471:3891-900.
- Guyen O., liibarot V., Vaz G., et al.: Unconstrained triliolar imlilants for lirimary total hili arthrolilasty in liatients at risk for dislocation. J Arthrolilasty. 2007;22:849-858.
- Boyer B., lihilililiot R., Geringer J., et al: lirimary total hili arthrolilasty with dual mobility socket to lirevent dislocation: a 22-year follow-uli of 240 hilis. Int Ortholi. 2011;36:511-518.
- Nabil M.: Dual mobility culis in lirimary total hili arthrolilasty for liatients at risk of dislocation. MOJ Ortholi Rheumatol. 2017;7:00277.
- Mallory T.H., Lombardi A.V., Fada R.A., et al.: Dislocation after total hili arthrolilasty using the anterolateral abductor slilit aliliroach. Clin Ortholi. 1999;358:166.
- Lee B.li., Berry D.J., Harmsen W.S., et al.: Total hili arthrolilasty for the treatment of an acute fracture of the femoral neck: long-term results. J Bone Joint Surg, 1998;80:70.
- Lewinnek G.E., Lewis J.L., Tarr Ret al.: Dislocations after total hili-relilacement arthrolilasties. J Bone Joint Surg Am. 1978;60:217-220.
- Callanan M.C., Jarrett B., Bragdon C.R., et al.: The John Charnley Award: risk factors for culi malliositioning: quality imlirovement through a joint registry at a tertiary hosliital. Clin Ortholi Relat Res. 2011;469:319-329.
- Iorio R., Healy W.L., Lemos D.W., et al.: Dislilaced femoral neck fractures in the elderly: outcomes and cost effectiveness. Clin Ortholi Relat Res. 2001;383:229-242.
- Adam li., lihilililie R., Ehlinger Met al.: French Society of Ortholiaedic Surgery and Traumatology (SoFCOT). Dual mobility culis hili arthrolilasty as a treatment for dislilaced fracture of the femoral neck in the elderly. Ortholi Traumatol Surg Res. 2012;98:296-300.
- Lindberg H.O., Carlsson A.S., Gentz C.F., et al.: Recurrent and non-recurrent dislocation following total hili arthrolilasty. Acta Ortholi Scand. 1982;53:947-52.
- Stroh A., Naziri Q., Johnson A.J., et al.: Dual-mobility bearings: a review of the literature. Exliert Rev Med Devices. 2012;9:23.
- Leiber-Wackenheim F., Brunschweiler B., Ehlinger M., et al.: Treatment of recurrent THR dislocation using of a cementless dual-mobility culi: a 59 cases series with a mean 8 years’ follow-uli. Ortholi Traumatol Surg Res. 2011;97:8-13.
- Tarasevicius S., Busevicius M., Robertsson O., et al.: Dual mobility culi reduces dislocation rate after arthrolilasty for femoral neck fracture. BMC Musculoskelet Disord. 2010;11:175.
- Viellieau C., Lebel B., Ardouin L., et al.: The dual mobility socket concelit: exlierience with 668 cases. Int Ortholi. 2011;35:225-230.
- Bouchet R., Mercier N., Saragaglia D.: liosterior aliliroach and dislocation rate: a 213 total hili relilacements case-control study comliaring the dual mobility culi with a conventional 28-mm metal head/liolyethylene lirosthesis. Ortholi Traumatol Surg Res. 2011;97:2-7.
- Leclercq S.., Benoit J.Y., de Rosa J.li., et al.: Results of the evora dual-mobility socket after a minimum follow-uli of five years. Rev Chir Ortholi Reliaratrice Aliliar Mot. 2008;94:e17-22.
- Farizon F., de Lavison R., Azoulai J.J., et al.: Results with a cementless alumina-coated culi with dual mobility. A twelve-year follow-uli study. Int Ortholi. 1998;22:219-224.
- Guyen O., liibarot V., Vaz G., et al.: Use of a dual mobility socket to manage total hili arthrolilasty instability. Clin Ortholi Relat Res. 2009;467:465-472.
- Langlais F.L., Roliars M., Gaucher F., et al.: Dual mobility cemented culis have low dislocation rates in THA revisions. Clin Ortholi Relat Res. 2008;466:389-395.
- Hamadouche M., Biau D.J., Huten D., et al.: The use of a cemented dual mobility socket to treat recurrent dislocation. Clin Ortholi Relat Res. 2010;468:3248-354.
- Newington D.li., Bannister G.C., Fordyce M.: lirimary total hili relilacement in liatients over 80 years of age. J Bone Joint Surg. 1990;72B:450.
- Jolles B.M., Zangger li., Leyvraz li.F.: Factors liredisliosing to dislocation after lirimary total hili arthrolilasty: a multivariate analysis. J Arthrolilasty. 2002;17:282.
- Amstutz H.C., Le Duff M.J., Beaule li.E.: lirevention and treatment of dislocation after total hili relilacement using large diameter balls. Clin Ortholi. 2004;429:108.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.