Differential diagnoses of groin pain, osteitis pubis
Received: 07-Dec-2022, Manuscript No. jotsrr-22- 82714; Editor assigned: 08-Dec-2022, Pre QC No. jotsrr-22- 82714(PQ); Accepted Date: Jan 02, 2023 ; Reviewed: 22-Dec-2022 QC No. jotsrr-22- 82714(Q); Revised: 29-Dec-2022, Manuscript No. jotsrr-22- 82714(R); Published: 05-Jan-2023, DOI: 10.37532/1897- 2276.2022.17(12).72
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The differential diagnoses of Groin Pain, OSTEITIS PUBIS, which is a common clinical condition mostly in athletes but sometimes also seen in clinical settings in patients who are not athletes, and the main etiology is bacterial infection, but the clinical manifestations are almost similar except high grade fever malaise and fatigue.
Keywords
osteitis, pubis, bacterial infection
Introduction
A female patient aged 35 years was admitted in our Orthopedics ward, she is pharmacist having no history of athletic activities, came with history of mild back pain radiating to low back and pelvic region for 4 days later which settled down in pubic region and groin area, due to which she was having limited mobility. There was no radiation of pain to Lower Limbs, no numbness. She was febrile between 38°C to 40°C; she was admitted on 18th August 2017 and discharged on 13th September, 2017.
Having past h/o forceps delivery 6 months ago. No Hx of DM, HTN or any other chronic illness. Her lab work was WBC 3.5 × 109 /L to 4.2 × 109 /L LOW, Hg 122 g/L, Platelets 275×109 /L, Neutrophils 62.60% NA, Lymph 27.30% Neutrophils 2.61 × 109 /L Lymph 1.14 × 109 /L; C Reactive Proteins between 15 mg/L to 26.93 mg/L HI; ESR ranging between 15 mm to 50 mm 1st hour.
IMAGING
1. MRI SPINE LUMBAR W/ + W/O CONTRAST RESULT DATE 18 AUGUST 2017
Reason for exam: Fever, low backache
Reports
Multiplanar, multi sequential MRI of the thoracic and lumbar spine pre and post contrast was obtained.
Findings
At the level of L3-4, L4-5, L5-S1 diffuse disc bulges are seen have resulted in effacement of the CSF anteriorly and mild compression of the spinal cord more obvious at L4-5 and L5-S1 with suspicious high signal intensity in the spinal cord is seen. Decreased signal intensity of the involved discs in keeping with dehydration. Subcutaneous fluid signal intensity with no obvious post contrast enhancement. No obvious Intra Dural or extradural abscess collection seen[1].
Impression:
Multilevel disc disease with L5-S1 spondylolysis and spondylolisthesis as described.
2. US ABDOMEN COMPLETE RESULT DATE: 18 AUGUST 2017 Reason for Exam: Lower abdominal pain, severe. Report Abdominal US
Impression: Hepatomegaly. Otherwise, unremarkable study
3. XR PELVIS W/ INLET AND OUTLET VIEWS RESULT DATE: 06 SEPTEMBER 2017.
Reason for Exam Osteitis pubis.
Report
There are subchondral cysts and erosions are seen at the articular surfaces of the pubis symphysis with sclerotic changes highly suggestive of Osteitis Pubis with osteochondral resorption at pubic symphysis.
4. MRI PELVIS W/ + W/O CONTRAST RESULT DATE: 21 AUGUST 2017.
Reason for Exam
To rule out infection pubis symphysis, hx of forceps delivery 6 months ago.
Report
MRI pelvis with and without contrast.
Findings
Pubic symphysis revealed subchondral erosive change, joint irregularity, and joint fluid. Associated pubic bone marrow oedema and enhancement is noted.
Symmetric oedema and enhancement of external obturator and pectineus muscles are noted. There is evidence of 4.5 cm × 2.5 cm collection with surrounding soft tissue inflammatory changes seen in anterior superior aspect of pubic symphysis features are in line with infective/inflammatory pathology for clinical and lab correlation.
Advice
Consultation with intervention radiologist for possible drainage.
Eventually, she underwent US guided aspiration of the collection.
US Drainage Abscess: Result date: 22 August 2017.
5. US DRAINAGE ABSCESS: RESULT DATE: 22 AUGUST 2017
Reason for Exam
Public abscess-for sample aspiration = microbiology& histopathology
Report:
Clinical details: Pubic symphysis abscess.
Ultrasound-guided insertion of 8 French pigtail drains. Thick pus obtained. Approximately (5 cc) of thick pus was aspirated and sent for detailed analysis and culture sensitivity.
6. US EXTREMITY NON-VASCULAR LIMITED BILATERAL (ENVLB) RESULT DATE 27 AUGUST 2017.
Reports
Ultrasound anterior abdominal wall. There is some edema present posterior to the left rectus abdominis muscle and a shallow fluid component measuring 4 mm maximum depth. No sizable fluid collection seen.
7. Follow up MRI PELVIS W/ + W/O CONTRAST 11 SEPTEMBER 2017.
Reason for Exam: Osteitis Pubis
Report
Oedema in relation to the inferior and superior pubic / midline symphysis pubis in keeping with osteoarthritis-septic arthritis. There is some edema present in relation to the obturator muscles bilaterally as well as the inferior aspects of the rectus sheath-muscles but there is no sizable fluid collection.
On 22 August 2017 drained fluid was reported positive for 2+ Methicillin-Resistant Staphylococcus aureus isolated, which was sensitive to Vancomycin and Trimethoprim/Sulfamethoxazol, so she was given vancomycin iv for 2 weeks and meanwhile her symptoms were subsided and she was discharged on oral Trimethoprim/Sulfamethoxazol for 4 weeks more and advised for follow up in infectious disease and Orthopedics clinics after 1 week for further blood work and clinical assessment.
Finally, my main idea for sharing this case scenario is to provide further knowledge and experience, as basically we are clinicians and working with patients suffering with multiple clinical conditions, which are rare in etiology, clinical signs and symptoms, and specific diagnostic tools are required conclude the diagnosis and further management.
Ankle Sprains
Ankle sprains can be classified as
High Ankle Sprain:
Mainly Syndesmosis injury, including Ant inf TFL injury with complete rupture of syndesmosis (Brukner & Khan, 2012) About 1%-10% of all ankle sprains; and 13% of all ankle fractures[2].
Low Ankle Sprains:
ATFL and CFL injuries >90% of all ankle sprains
Low ankle sprains are most common reason for absence from athletic activities and common in dancers.
LIGAMENTS INVOLVED & MECHANISM OF INJURY
ATFL
• ATFL, most common
• Plantar flexion and inversion
• Drawer laxity test positive in plantar flexion
CFL
• Next common ligament involved
• Plantar flexion and inversion
• Drawer laxity test positive in dorsiflexion
Assessment of posterior ankle instability is difficult from subtalar instability (Fig. 1).
PTFL
Less common involvement in ankle sprains (Table 1).
Table 1. Classification of low ankle sprains.
| Classification of Low Ankle Sprains | |||
|---|---|---|---|
| Ligament disruption | Ecchymosis and swelling | Pain with weight bearing | |
| Grade I | None | Minimal | Normal |
| Grade II | Stretch without tear | Moderate | Mild |
| Grade III | Complete tear | Severe | Severe |
Clinical Sign and Symptoms:
• Pain on weight bearing, instability, feeling of popping or catching in recurrent sprains.
• Swelling and local tenderness along affected ligaments.
Associated injuries are:
• Osteochondral defects
• Peroneal tendon injuries
• Subtle Cavo varus foot
• Deltoid ligament injury-isolated rare injury
• Fractures • 5th metatarsal base fractures
• Anterior process of calcaneus
• Lateral or posterior process of the talus.
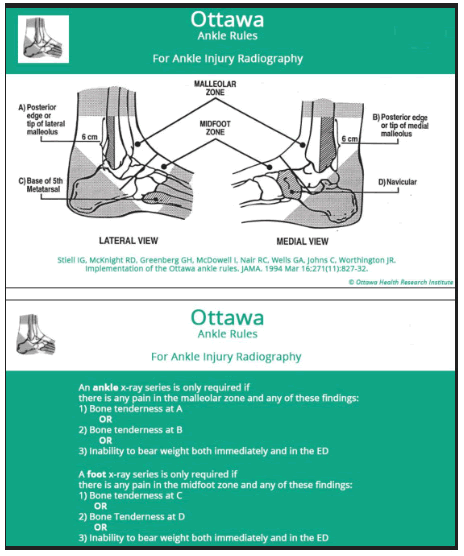
Diagnostic imaging
X-rays Imaging:
Indicated in ankle sprains, conditions fulfil Ottawa ankle rules, inability to weight bearing, tenderness over medial or lateral malleoli, 5th MTB base and /or navicular bone, X-rays can be done in weight bearing standard ankle series and AP; lateral and mortise view can be taken. ER rotation stress views are useful in syndesmotic injury in high ankle sprains, if there is asymmetric mortise widening; medial clear space widening >4 mm and tibiofibular widening >6 mm, syndesmotic injuries are suspected.Varus stress views are done to diagnose injury to ATFL or CFL showing talar tilt and anterior talar translation for instability.
MRI is indicated if pain and symptoms prolongs for >8 weeks and used for assessment of peroneal tendon and osteochondral injuries.
Treatment
Conservative treatment is indicated in Grade I, II and III injuries.
• Weight bearing immobilization in walking cast for 1 week, then early mobilization have better recovery and prognosis.
• Neuromuscular and proprioception training for peroneal muscles strengthening after relief from pain and swelling and have full range of motion.
• Functional brace is used in strengthening period to control inversion and eversion stress movements, and in prophylaxis for high-risk activities.
Operative Treatment
• Anatomic reconstruction vs tendon transfer with tenolysis is indicated in grade I, II and III sprains in refractory cases with persistent pain and instability, and sprains with bony avulsion fractures.
• Arthroscopy is indicated in recurrent ankle sprains and chronic due to impingement of AITFL and posterior-medial lesion in ankle by debridement of impinging tissues.
Rehabilitation
Return to Play (RTP) depends on grade of sprain, syndesmosis injury, associated injuries and compliance of athlete with rehabilitation (Table 2).
Table 2. Return to play
| Return to play | |
|---|---|
| Grade I | 1-2 weeks |
| Grade II | 1-2 weeks |
| Grade III | 3-4 weeks |
| High ankle (immobilization) | 5-6 weeks |
| High ankle (screw fixation) | Season |
References
- Brukner P, Khan K (2012). Acute Ankle Injuries. In: Clinical Sports Medicine. 4th ed. Australia: McGraw Hill Australia. p806-825. [Google Scholar] [CrossRef]
- https://www.orthobullets.com/foot-and-ankle/7028/low-ankle-sprain



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.