Correlation between borderline acetabular dysplasia and hip osteoarthritis: A retrospective cross-sectional radiographic study
2 Department of İndustrial Engineering, Yildiz Technical University, Istanbul, Turkey, Email: abc@gmail.com
3 Faculty of Medicine, Orthopaedics and Traumatology, Yeniyuzyil University, Istanbul, Turkey, Email: abc@gmail.com
4 Faculty of Medicine, Orthopaedics and Traumatology, Istanbul University, Istanbul, Turkey, Email: abc@gmail.com
Received: 20-Apr-2021 Accepted Date: May 11, 2021 ; Published: 18-May-2021, DOI: 10.37532/1897-2276.2021.16(1).19
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Hip osteoarthritis is one of the most prevalent diseases commonly affect older patients. It is also one of the most common causes of functional disability and musculoskeletal pain, but about half of the OA patients do not complain about these symptoms and remain undiagnosed. The aim of this study is to compare the radiological findings of OA with the acetabular dysplasia in patients who have not been diagnosed with OA before.
Methods: 365 patients (200 males, 165 females) aged between 40 and 65 were included in the study. Data were obtained retrospectively, among abdominal and pelvic Computerized Tomographies (CT) of patients consulted in urology department of our hospital with urological complaints. AP Topogram of each patient’s CT’s was evaluated. Center-Edge Angle (CEA), Acetabular Angle (Sharp Angle-SA) were measured and Tönnis Grading of each hip were calculated. Correlation between CEA and SA measurements and Tönnis Grading (grade 0, grade 1 and grade 2) of hip OA were evaluated.
Results: Overall, 8.63% (7.25% in males and 10.30% in females) of the patients had AD, based on at least one of the measurements (CEA<25° or SA>42°). Rate of hip OA was found as 8% in males and 6.36% in females (overall 7.26%). Mean CEA was 35.06° (± 5.58) in males and 34.71° (± 5.91) in females (overall 34.90° (± 5.73). Mean SA was 37.23° (± 2.92) in males and 37.75° (± 3.54) in females (overall 37.46° (± 3.22). There were no significant difference between Tönnis grades 0,1 and 2 groups, with respect to mean CEA and SA rates (p<0.27). The rate of Tönnis grade 2 OA was significantly higher in dysplastic group based on <25 CEA values, but there was no correlation between the hip OA and AD based on >42° SA values (p=0.32). So; unlike SA, CEA seems to have a role in etiology of the hip OA.
Conclusion: This study has provided prevalence values of CEA and SA in patients with radiologic evidence of hip osteoarthritis. AD; based on CEA, but not SA is correlated with radiographic findings of hip OA.
Level of evidence: IV, retrospective series.
Keywords
acetabular dysplasia, hip osteoarthritis, CE angle, sharp angle, computerized tomography
Introduction
The burden of hip Osteoarthritis (OA) has been growing over the past two decades and is estimated to grow 174% by 2030; especially among the elders [1]. One quarter of 45-year-old adults are expected to develop symptomatic hip OA [2]. There is a wide variation of prevalence for mild hip OA between 0.9%-23% in different populations. Its prevalence is reported to be lower in Asian and African populations, and higher in European populations [3-9].
OA is considered to be a multifactorial disease. Both systemic and local factors affect the hip joint, but local factors play the final role [3]. Age, gender, ethnicity, body weight, physical activity, history of trauma, and also structure/alignment of the joint are some of the common risk factors [4]. There are several studies indicating that gross bone abnormalities; including Acetabular Dysplasia (AD) can play role in the formation of OA. AD is thought to cause OA; because in AD, two parts of the hip joint are not equally connected, by giving rise to higher contact pressure over a smaller surface on hip joint [10]. But especially, in mild forms of dysplasia, the relationship between AD and OA is not fully understood.
Although, pain is one of the major symptoms of OA, symptoms just as pain and stiffness are not always correlated with radiographic changes; and about 50% of patients with OA do not complain about related symptoms [11]. OA is usually classified according to radiographic criteria. Tönnis grading system is one of the classification systems, commonly used for evaluating hip OA radiologically. According to this system; degenerative changes of the hip are evaluated in three degrees radiologically, as; Grade 0: no degenerative changes; Grade 1: mild degeneration; Grade 2: moderate degeneration and Grade 3: Severe degeneration [12].
The aim of the present study is to compare the radiological findings of OA with AD in patients who have not been diagnosed with OA before.
Patients and Methods
Study design
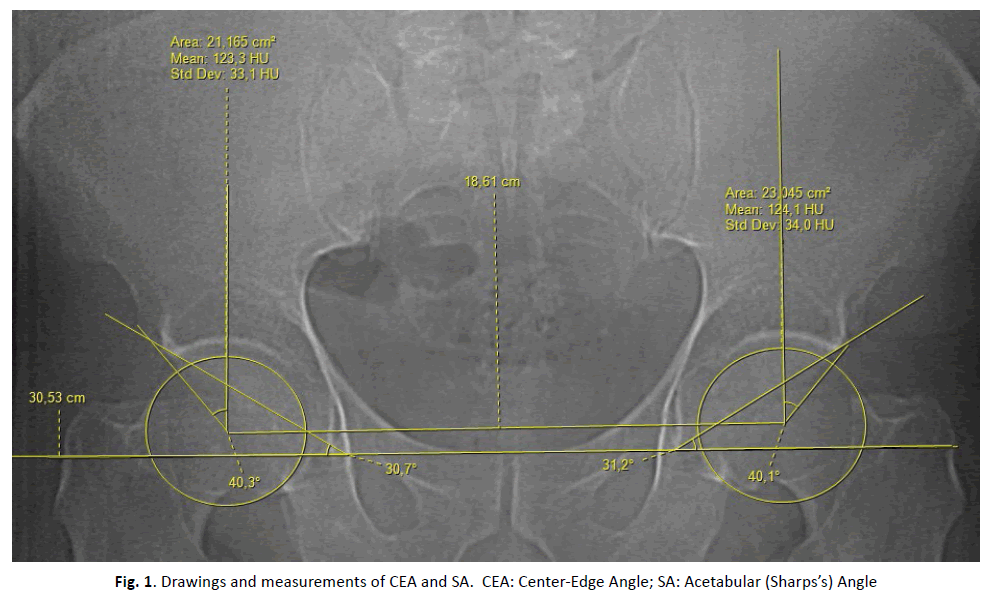
365 patients (200 males, 165 females) aged between 40 and 65 were included in this retrospective study. Patients with hip replacement and those with pelvic bone tumour and those with hip deformity due to a previous disease were excluded. Each patient had a pelvic or abdominal Computerized Tomography (CT) for an indication without orthopedic inducement. Lower abdomen and pelvic CT’s were retrieved, and individual hip joints were assessed. CT topograms of each abdomen and/or pelvic CT (10 ma, 120 kv, GE Bright Spears; simple AP topogram) were evaluated. Tönnis grading for the radiographic OA was performed by two orthopedists blinded to study. 2 hips (0.27%) of 2 patients which classified by only one of two authors as Tönnis grade 3 and 2 hips (0.27%) who had undergone a contralateral total hip arthroplasty were excluded since the change in the loading pattern of the contralateral hip joint due to previous surgery may lead to the development of osteoarthritis. Level of agreement was qualified using kappa statistics. Acetabular Dysplasia (AD) was assessed by two observers blinded to the results of the Tönnis grading, using two measures: Center-Edge Angle (CEA) and Sharp Angle (SA). The CEA was defined as the angle between the line joining the center of the femoral head to the lateral margin of the acetabular roof and the line perpendicular to the line joining the centers of the femoral heads [13]. The centers of the heads were located and all angles were measured with the help of measurement function of Clear Canvas Software, Version 2.0.1272937986 SP1 by Synaptive Medical (Figure 1). Level of agreement was qualified using kappa statistics. The reproducibility of the radiological parameters was good to excellent, and the kappa values were all >0.8.
Statistical Analysis
R 3.6.1 (R Foundation for Statistical Computing, Viena, Austria) software was used for statistical analysis. Correlations between mean CEA-radiologic OA, mean SA-radiologic OA, and mean CEA-age groups (>55 and <55) were analyzed by two sample t-test. The rate of patients with dysplastic hips based on CEA and SA in patient groups with OA (Tönnis grade 0-1 and Tönnis grade 2) was compared using a proportion test. Two-sided p-values <0.05 were considered significant in all analysis.
Results
A total of 730 hips of 365 patients were studied. 68 hips of 43 patients were found as dysplastic. 33 hips were dysplastic based on only >42° SA values. 23 hips were dysplastic based only on <25° CEA values. There were no patients with CEA<20°. Mean CEA values of right hips and left hips were 34.69 ± 5.55° and 35.11 ± 5.90°; respectively. Mean SA values of right hips and left hips were 37.36 ± 2.98° and 37.56 ± 3.46°; respectively. When men and women were analyzed separately, mean CEA values of males and females were 35.06 ± 5.58° and 34.71 ± 5.91°; mean SA values of males and females were 37.23 ± 2.92° and 37.75 ± 3.54°; respectively. Also, rate of AD was found 7.26% in men and 10.30% in women. Overall, 8.63% of the hips had AD based on at least one of the measurements (CEA<25° and/or SA >42°). There was a significant increase in mean CEA measurements in age>55 group (p=0.032). Tönnis grades 0, 1 and 2 OA were seen in 56.16%, 36.58% and 7.26% of the hips; respectively (Table 1).
| MALE | FEMALE | TOTAL | |
|---|---|---|---|
| Number of joint | 400 | 330 | 730 |
| CEA | |||
| Mean CEA R | 34.83 (± 5.37) | 34.53 (± 5.78) | 34.69 (± 5.55) |
| Mean CEA L | 35.30 (± 5.78) | 34.89 (± 6.04) | 35.11 (± 5.90) |
| Mean CEA (R+L) | 35.06 (± 5.58) | 34.71 (± 5.91) | 34.90 (± 5.73) |
| SA | |||
| Mean SA R | 37.14 (± 2.82) | 37.64 (± 3.14) | 37.36 (± 2.98) |
| Mean SA L | 37.32 (± 3.02) | 37.85 (± 3.91) | 37.56 (± 3.46) |
| Mean SA (R+L) | 37.23 (± 2.92) | 37.75 (± 3.54) | 37.46 (± 3.22) |
| Tönnis Rates | |||
| Right Hip Tönnis | |||
| 0-1 R | 189 (47.25%) | 158 (47.88%) | 347 (47.53%) |
| 2 R (Mean OA rate) | 11 (2.75%) | 7 (2.12%) | 18 (2.47%) |
| Left Hip Tönnis | |||
| 0-1 L | 179 (44.75%) | 151 (45.76%) | 330 (45.21%) |
| 2 L (Mean OA Rate) | 21 (5.25%) | 14 (4.24%) | 35 (4.79%) |
| R+L Hip Tönnis | |||
| 0-1 L | 368 (92.00%) | 309 (93.64%) | 677 (92.74%) |
| 2 L (Mean OA Rate) | 32 (8.00%) | 21 (6.36%) | 53 (7.26%) |
| Prevalance of AD | 29 (7.25%) | 34 (10.30%) | 63 (8.63%) |
| Tonnis vs CEA (Prevelance) | |||
| CEA<25 in Tönnis grade 0-1 | 13 (1.78%) | 8 (1.10%) | 21 (2.88%) |
| CEA<25 in Tönnis grade 2 | 5 (0.68%) | 3 (0.41%) | 8 (1.10%) |
| Tönnis vs SA (prevelance) | |||
| SA>42 in Tönnis grade 0-1 | 14 (1.92%) | 22 (3.01%) | 36 (4.93%) |
| SA>42 in Tönnis grade2 | 3 (0.41%) | 1 (0.14%) | 4 (0.55%) |
CEA: Center-Edge Angle; SA: Acetabular (Sharps’s) Angle; OA: Osteoarthritis; AD: Acetabular Dysplasia
Table 1. Comparative evaluation of Tönnis Grading with SA and CEA measurements in male and female patients
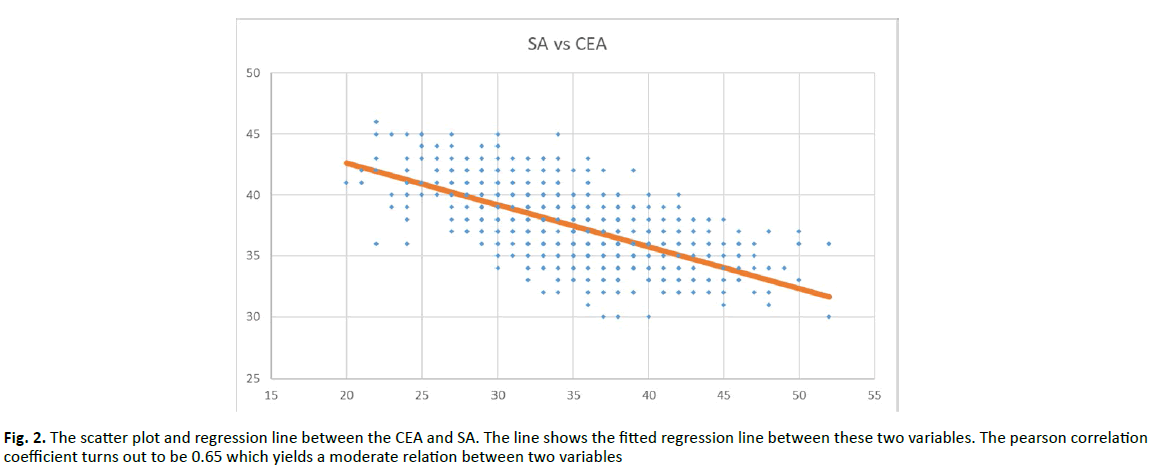
There were no significant difference in terms of mean CEA and mean SA values, between groups of Tönnis Grade 0-1 and Tönnis grade 2 (p=0.29 and p=0.27; respectively.) The rate of Tönnis grade 2 OA was significantly higher in dysplastic hips, based on <25° CEA values (p<0.001), but there was no correlation between the OA and diysplastic hips based on >42° SA values (p=0.33). So, in contrast with SA, it seems that CEA has a significant correlation with the development of hip OA. There were moderate correlation between CEA and SA (Figure 2).
Discussion
In the present study; the prevalence of mild hip OA in Turkish population is found to be 7.26%, lower than some European countries but higher than some eastern populations. This rate varies among different populations between 5%-23% [5-9]. Radiological parameters of Tönnis grading were used to classify the hip OA [14-16]. AD was defined as the presence of measurements; CEA <25° or/and SA>42°. We demonstrated that, AD based on <25° CEA measurement is associated with mild hip OA and is thought to play a major role in development of hip OA. On the other hand; dysplasia based on >42° SA measurement is not found to be associated with hip OA. We observed 63 dysplastic hips (8.63% of all hips): 6 of these were dysplastic based on both CEA and SA measurements, remaining 57 hips were dysplastic based on one of the CEA (29 hips) or SA (40 hips) measurements.
OA of the hip is one of the main causes of functional disability and pain. For preventive and treatment strategies, understanding of the disease process is very important. Although mild AD suggested as initiator of subsequent joint degeneration due to stress loading on the superolateral border of the hip and assumed to be an etiological factor of OA [17], there is a controversy in the literature about correlation of AD and OA. Although the risk of hip OA is especially higher in younger subjects with AD, the cause/effect relationship between AD and hip OA in older subjects remains controversial. We aimed to investigate the potential effects of radiographic measurements of AD on this debate. In our study, AD prevalence was 8.63%. AD prevalence is reported between 1.8%-9.8% in various populations [5,6,18,19], compatible with the present study. There are also various studies reporting higher prevalence of AD in certain populations [7]. Jacobsen et al studied 4151 hips within a subset of the Copenhagen City Heart Study and showed that AD was significantly associated with OA [19]. Cooperman et al. reported that almost all patients with stable AD (CEA<20° and no sublux) will develop OA by 65 years of age, and unstable AD (CEA<20°, with subluxation) always leads to OA by 65 years of age [20]. Interestingly, Gosvig et al. used the same database with Jacobsen and concluded that AD was not statistically associated with OA [21]. The evidence for the influence of AD on the occurrence of hip OA, at ages of 50-60 or older, is limited [22]. Chitnavis reported that, up to 40% of hips of patients who underwent total hip replacement manifested AD [23]. The studies cited so far showed that AD and OA are correlated. On the other hand; some of the researchers claim that there is no relation between AD and OA. Some cross-sectional studies conducted with older subjects and utilized urography suggested no relationship between AD and OA [6,24,25]. Lane et al. [13] and Goker et al. reported that; AD did not seem to play a major role in the development of radiographic hip OA [18].
The term of CEA was developed by Wiberg [15] as a measurement of the degree of acetabular development and the degree of dislocation of the femoral head in children. Fredensborg reported that; CEA increases slowly until the age of 15 and after this age there is only a slight increase, the curve was reported to be almost identical in both sexes [26]. CEA values of 20°-25° is considered to be borderline dysplasia [26,27]. The normal values of CEA in adults are between 27±7° and 37.9 ± 5.6°, with slight differences among different populations [14,18,19,24,26,28-37]. In our study, mean of CEA values was 35.06° (± 5.58) in males, 34.71° (± 5.91) in females, overall 34.90° (± 5.73).
SA measurement was devised to assess the degree of a patient’s hip dysplasia without considering the position of the femoral head [14]. SA describes the angle formed between the inter-teardrop-line and the line connecting the inferior tip of the teardrop to the lateral acetabular rim. It reflects the acetabular morphology and frontal deviation of acetabulum. It is not affected by pelvis position. The normal values for this angle are reported by Sharp as 33°-38°. Upper limit of SA is determined by Sharp as 42° and by Ozcelik et al as 45° in adults [38]. Mean SA values are found to be different in different populations [14,19,31,33,34,36,38-40]. In our study we found that mean SA value was 37.23° ± 2.92 in males, and 37.75°± 3.54 in females (overall 37.46°± 3.22).
Results of the present study indicate that; CEA is useful to detect the relation between femoral head and acetabulum and it is strongly correlated with mild hip OA. On the other hand; we could not observe any relation between SA and OA. SA only gave us information about structure of acetabulum. In the literature, there are many studies investigating the relation between CEA and OA [6- 8,14,16,18,25,28,32,41-43] but there is limited information that reveal the relation between SA and OA. The results of these limited studies about SA-OA relationship are also controversial. Nakamura [36] reported that, SA values showed no significant difference between normal and hip OA groups. In their study by surveillance of 86 hips of 59 patients more than 10 years, Hasegawa et al. [44] reported that, SA is not correlated with OA. Ipach [45] found significant relationship between SA and OA. Jingushi [46] et al. reported that SA values >45° significantly increase odds ratios for OA in comparison to <40°.
Our study has many limitations. First of all, our study is retrospective in nature. We measured only CEA and SA which may not be enough to evaluate the three-dimensional structure of the hip joint. CEA does not indicate the shape or depth of acetabulum and does not assess vertical migration of femoral head. We were able to measure only SA and the lateral CEA on CT topogram. But in dysplastic hips CEA decrease significantly in all three directions 46. Hence measuring the lateral CEA might not be enough to predict the progression of OA. However, it is a retrospective study and we avoid to additional radiation exposure to our patients by extra XR and CT.
Conclusion
The results of the present study suggest that there is a significant relationship between OA and CEA however there is no evidence that shows an association between SA and OA. These results are comparable to other published data.
Disclosure of Interest
The authors declare that they have no competing interest.
Authors Contributions
Z Soydan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design: Z Soydan, HH Ceylan, C Sen
Acquisition of data: Z Soydan, A Kasabaligil, M Mert,
Statistical Analysis and interpretation of data: Z Soydan, MG Guler, C Sen
All authors read and approved the final version of the manuscript.
REFERENCES
- Nho S.J., Steven M.S., Kymes M., et al.: The Burden of Hip Osteoarthritis in the United States: Epidemiologic and Economic Considerations. J Am Acad Orthop Surg. 2013;21:1-6.
- Courties A., Berenbaum F.: Is hip osteoarthritis preventable? Joint Bone Spine. 2019;87:371-375.
- Felson D.T., Zhang Y.: An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheumatism. 1998;41:1343-1355.
- O'Neill T.W., McCabe P.S., McBeth J.: Update on the epidemiology, risk factors and disease outcomes of osteoarthritis. Best Practice Res Cli Rheumatol. 2018;32:312-326.
- Roux C.H., Saraux A., Mazieres B., et al.: Screening for hip and knee osteoarthritis in the general population: predictive value of a questionnaire and prevalence estimates. Ann Rheum Dis. 2008; 67:1406-1411.
- Lau E.M.C., Symmons D.P.M., Croft P.: The Epidemiology of Hip Osteoarthritis and Rheumatoid Arthritis in the Orient. Cli Ortho Rel Res. 1996;323:81-90
- Johnsen K., Goil R., Reikerås O.: Acetabular dysplasia as an aetiological factor in development of hip osteoarthritis. Int Orthop. 2009;33:653-657.
- Ingvarsson T., Hagglund G., Lindberg H., et al.: Assessment of primary hip osteoarthritis: comparison of radiographic methods using colon radiographs. Ann Rheum Dis. 2000;59:650-653.
- Cvijetic S., Campbell L., Cooper C., et al.: Radiographic osteoarthritis in the elderly population of Zagreb: distribution, correlates, and the pattern of joint involvement. Croatian Med J. 2000;41:58-63.
- Thomas G.E., Palmer A.J., Batra R.N., et al.: Subclinical deformities of the hip are significant predictors of radiographic osteoarthritis and joint replacement in women: a 20 year longitudinal cohort study. Osteoarthritis Cartilage 2014;22:1504-1510.
- Hannan M.T., Felson D.T., Pincus T.: Analysis of the discordance between radiographic changes and knee pain in osteoarthritis of the knee. J Rheumatol 2000;27:1513-1517.
- Brückl R., Hepp W., Tönnis D.: Differentiation of normal and dysplastic juvenile hip joints by means of the summarized hip factor [in German]. Arch Orthop Unfallchir. 1971;74:13-32.
- Lane N.E., Nevitt M.C., Cooper C., et al.: Acetabular dysplasia and osteoarthritis of the hip in elderly white women. Ann Rheumatic Dis. 1997;56:627-630.
- Park J.M., Gun-Il Im.: The correlations of the radiological parameters of hip dysplasia and proximal femoral deformity in clinically normal hips of a korean population. Clinics Orthop Sur. 2011;3:121-127.
- Wiberg G.: Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand.1939;83:1-135
- Murray R.O.: The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810-824.
- O'Brien T.M., Moran R., McGoldrick F.: The aetiology of degenerative disease of the hip. A review of 400 cases. Ir J Med Sci. 1989;158:63-66.
- Goker B., Sancak A., Haznedaroglu S.: Radiographic hip osteoarthritis and acetabular dysplasia in Turkish men and women. Rheumatol Int. 2005;25:419-422.
- Jacobsen S., Sonne-Holm S., Soballe K. et al.: Hip dysplasia and osteoarthrosis: a survey of 4151 subjects from the Osteoarthrosis Substudy of the Copenhagen City Heart Study.Acta Orthop. 2005; 76:149-58.
- Cooperman D.R.: How good is the evidence linking acetabular dysplasia to osteoarthritis? J Pediat Orthop. 2019;39:S20-S22
- Gosvig K.K., Jacobsen S., Sonne-Holm S., et al.: Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92:1162-1169.
- Lievense A.M., Bierma-Zeinstra S.M.A., Verhagen A.P. et al.: Influence of hip dysplasia on the development of osteoarthritis of the hip. Ann Rheum Dis. 2004;63:621-626.
- Chitnavis J., Sinsheimer J.S., Suchard M.A.: End-stage coxarthrosis and gonarthrosis. aetiology, clinical patterns and radiological features of idiopathic osteoarthritis. Rheumatol. 2000;39:612-619.
- Yoshimura N., Campbell L., Hashimoto T., et al.: Acetabular dysplasia and hip osteoarthritis in Britain and Japan. Br J Rheumatol. 1998;37:1193-1197.
- Croft P., Cooper C., Wickham C.: Osteoarthritis of the hip and acetabular dysplasia. Ann Rheum Dis. 1991;50:308-310.
- Fredensborg N.: The CE angle of normal hips. Acta Orthop Scand. 1976;47:403-405.
- Murphy S.B., Kijewski P.K., Millis M.B., et al.: Acetabular dysplasia in the adolescent and young adult. Clin Orthop 1990; 261: 214-223.
- Mechlenburg I., Stilling M., Romer L., et al. Reference values and variation of acetabular angles measured by computed tomography in 170 asymptomatic hips. Acta Radiol 2019; 60:895-901.
- Umer M., Sepah Y.J., Asif S., et al.: Acetabular morphometry and prevalence of hip dysplasia in the South Asian population Orthop Rev (Pavia). 2009;1:10.
- Aydin M., Kircil C., Polat O., et al.: Adult acetabulo-pelvic parameters in Turkish society: A descriptive radiological study. Acta Orthop Traumatol Turc. 2016;50:623-627.
- Houcke J.V., Yau W.P., et al.: Prevalence of radiographic parameters predisposing to femoroacetabular impingement in young asymptomatic chinese and white subjects. J Bone Joint Surg Am. 2015;97:310-317
- Daysal G.A., Goker B., Gonen E., et al.: The relationship between hip joint space width, center edge angleand acetabular depth. Osteoarthritis and Cartilage. 2007;15:1446-1451
- Laborie L.B., Engesæter O., Lehmann T.G.: Radiographic measurements of hip dysplasia at skeletal maturity-new reference intervals based on 2,038 19-year-old Norwegians. Skeletal Radiol. 2013;42:925-935.
- Jeremic D., Macuzic I.Z., Vulović M.: Sex differences in anatomical parameters of acetabulum among asymptomatic Serbian population. Vojnosanit Preg. 2011;68:935-939.
- Fujii M., Nakashima Y., Jingushi S., et al.: Intraarticular findings in symptomatic developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:9-13.
- Nakamura S., Ninomiya S., Nakamura T.: Primary osteoarthritis of the hip joint in Japan. Clin Orthop Relat Res. 1989:190-196.
- Johnsen K., Goll R., Reikerås O.: Acetabular dysplasia in the Sami population: a population study among Sami in north Norway. Int J Circumpolar Health. 2008;67:147-153.
- Sharp I.K.: Acetabular Dysplasia. J Bone Joint Sur. 1961;43: 268-272.
- Ozçelik A., Omeroglu H., İnan U., et al.: Normal values of several acetabular angles on hip radiographs obtained from individuals living in the Eskişehir region. Acta Orthop 2002;36:100-105.
- Tannast M., Hanke M.S.: What are the radiographic reference values for acetabular under-and overcoverage? Clin Orthop Relat Res. 2015;473:1234-1246.
- Aktas S., Pekindil G., Ercan S., et al.: Acetabular dysplasia in normal Turkish adults. Bull Hosp Jt Dis. 2000;59:158-162
- Han C.D., Yoo J.H., Lee W.S. et al.: Radiographic parameters of acetabulum for dysplasia in Korean adults. Yonsei Med J. 1998;39:404-408.
- Birrell F., Silman A., Croft P. et al.: Syndrome of symptomatic adult acetabular dysplasia (SAAD syndrome). Ann Rheum Dis. 2003;62:356-358.
- Hasegawa Y., Iwata H., Mizuno M., et al.: The natural course of osteoarthritis of the hip due to subluxation or acetabular dysplasia. Arch Orthop Trauma Surg 1992;111:187-191.
- Ipach I., Rondak I.C., Sachsenmaier S.: Radiographic signs for detection of femoroacetabular impingement and hip dysplasia should be carefully used in patients with osteoarthritis of the hip. BMC Musculoskelet Disord. 2014;8:150
- Jingushi S, Ohfuji S, and Sofue M. Osteoarthritis hip joints in Japan: involvement of acetabular dysplasia. J Orthop Sci. 2011; 16:156–164



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.