Complete displaced forearm distal fractures in children: A prospective study of conservative treatment
2 Faculty of Medicine, University of Gjakova FehmiAgani, Gjakova, Republic of Kosovo, Email: skender@gmail.com
3 Faculty of Medicine, University of Tetova, Macedonia, Email: dren.ukaj@gmail.com
4 Regional Hospital Center Prizren, Republic of Kosovo, Email: osman.zhuri@gmail.com
5 University Clinical Center of Ljubljana, Ljubljana, Slovenia, Email: matjaz.veselko@gmail.com
Received: 07-Nov-2017 Accepted Date: Nov 20, 2017 ; Published: 24-Nov-2017
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Complete displaced forearm fractures in children are not very common and are usually a product of indirect trauma. They can be treated with closed reduction with plaster immobilization, closed reduction- pinning with plaster immobilization and open reduction with internal fixation. The purpose of this study is to address the importance of orthopedic treatment namely plaster immobilization for patients with this type of fractures for attaining good functional results, no further dislocation and financially acceptable.
Methods: In the study we have included 104 patients from three to nine years of age presenting between January 2009 and December 2016 with closed displaced forearm fractures and were followed prospectively. Sedation with I.V. anesthesia was performed. Fractures were manipulated and reduced with traction and rotation, followed by radioscopy then immobilized in well molded plaster casts until healed, (radio/carpal and brach/antebrach plaster immobilization). The follow up was done by Radiographs and patient controls after 3 days, 10 days, 17days; this was to reduce chances for re-displacement of the fracture. Follow up was done by radiography checks as well as after 4 weeks and at the end after 6 weeks. Patients were followed for at least 3 months.
Results: One hundred and four children with an average age of 6.27 ± 2.31years were included in the study. All fractures have been displaced of the both distal radius and ulna. The male/female ratio was 3:1. The average duration of casting was forty-three days. Three patients underwent closed re-reduction 3 days after first reduction. During the first two weeks after reduction, re-displacement occurred in none of the children. All hundred and four (104) patients achieved clinical and radiographic union with a full range of wrist motion.
Conclusion: Closed reduction with flexed elbow immobilization of displaced distal forearm fractures results in satisfactory functional outcome. Regular control after immobilization beginning from 3rd day is important for preventing the re-displacement of these fractures. Another major outcome is the cheap treatment compare to open reduction.
Keywords
Displaced forearm fractures, Children fractures, Forearm, Conservative treatment
Abbreviations
UCCK: University Clinical Center of Kosova; CEPI: Committee of Ethical and Professional Issues
Introduction
Distal forearm fractures present some of the most common bony injuries [1], with a reported UK annual adult incidence of around 9/10,000 in men, 37/10,000 in women [2] and 16/1000 in children [3]. A child’s bones heal more quickly than an adult’s, so it is important to treat a fracture promptly—before healing begins—to avoid future problems.
Contrasting to that, complete displaced forearm fractures in children are not very common, with their treatment being yet questionable.
They can be treated with closed reduction and plaster immobilization, closed reduction-pinning with plaster immobilization, and open reduction.
The initial displacement and post reduction residual translation were found to be a statistically significant risk factor for re-displacement by various authors amongst many controversies [4-6].
The main aim of this study old should result in satisfactory functional outcome. This should be since patients of this age do have more remodeling potential and greater acceptable reduction limit. Flexed elbow immobilization after 2 weeks/3 weeks can be replaced by below-elbow immobilization.
Regular control after immobilization beginning from 3rd day is important for preventing the re-displacement of these fractures. The swelling reduces; therefore, the remained deformity can be corrected and also the cast or the gap of the cast can be improved. Additionally, by not having to spend extra nights in hospital makes it more convenient for the child and family in both commodity and economical aspect.
Methods
Study design
A prospective, intervention study was performed in the Orthopedics and Trauma Clinic of the University Clinical Center of Kosovo.
Participants
A total number of 104 subjects, aged between 3-9 years old (mean average 6.27 ± 2.31) took part. 36 or 34.1% of participants were girls, while 68 or 65.9% were boys. All patients were eligible for inclusion in study group.
Inclusion criteria consisted of:
• Group age (3-9),
• Type of fracture (complete displaced forearm distal fracturesipsilateral radius and ulna),
• Study period (January 2009 to December 2016).
Intervention process
104 patients with complete dislocated forearm fracture underwent a closed reduction and cast immobilizations under fluoroscopy and general anesthesia. Reduction was done with gentle traction by two assistants (one on proximal end and the other one in distal endhand) determining the initial alignment of the ends of the radius and ulna, while the main orthopedic surgeon angulating the fracture in the direction of the original displacement (exaggeration of the deformity - often >90°- disengaging the fragments), correcting rotation and “hinging over” the distal fragment in the fracture site.
A well-molded (3-point indices) above-elbow splint, plus additional radial below-elbow splint was placed (radio/carpal and brach/ antebrach plaster immobilization), with wrist in 20° volar flexion, neutral rotation, and 15° ulnar deviation.
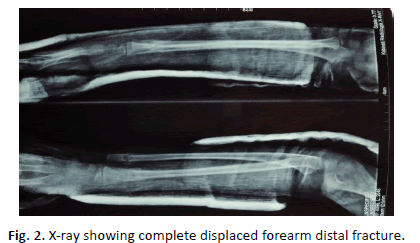
The demographics and clinical variables were recorded during patient recruitment. The evaluated risk factors for re-displacement included swelling, time of reduction (compared to time of injury), quality of reduction, type of plaster (above or below elbow), quality of plaster, and residual post-reduction displacement (translation percentage/angulation), frequent x-ray follow-up. Pre-manipulation fractures were classified as complete dislocated, no bone contact fractures. Quality of reduction was classified as anatomic (reduction without any translation and angulation) [7], good (less than 10° angulation or less than 2 mm translation) [8], and fair (10° to 20° angulation or 2 mm to 5 mm translation or less than 5° of radial deviation or 5°-10° angulation with less than 2 mm translation) [9], according to criteria described by Alemdaroglu et al. [10] (Fig. 1 and 2).
Re-displacement was defined as: [7] ≥ 10 degrees of dorsal or volar angulation, or ≥ 5 degrees of radial deviation [11], or ≥ 3 mm of translation [12], or a combination of 2 mm of translation and ≥ 5 degrees of angulation [11].
Acceptable limits of reduction guidelines were:
In infants (3 yrs to 5 yrs. in our study), < 30° of angulations in the coronal plane – accepted and 5 - 10 years old, residual angulation is no greater than 15° to 20°.
The angulation and translation of the residual post-reduction fragments were measured with standard means, using goniometer.
Patient’s follow up (chronologically):
• 1st day radiographs and patient controls (post reduction with fluoroscopy, plaster cast);
• 3rd day (X-ray) – While re-reduction under fluoroscopy was needed in three patients after the swelling was reduced;
• 14th day – (X-ray);
• 2nd week/3rd week (Depending on previous x-ray changes) - shortening of the plaster below the elbow;
• 4th week – Follow up;
• 6th week – Removing the plaster;
• 3rd month – Last visit.
Statistical analysis
All the statistical analyzes were performed by using SPSS program for statistical analysis, version 12.0 for windows.
Descriptive statistics was generated for all the study variables, including here the mean average for continuous variables and relative frequencies for categorical variables.
Results
As previously indicated, the total number of participants (n) in the study is 104 (Table 1). While recognizing the objective of the study which aims to distinguish among treatment methods between different age groups, the descriptive statistics in terms of age are as follows:
| Participants | Age | Fractured Hand | ||
|---|---|---|---|---|
| Right | Left | |||
| Total | 104 (100%) | 6.27 ± 2.31 | 64 or (61.5%) | 40 or 38.5% |
| Boys | 68 (65.4%) | 6.86 ± 2.26 | 47 or (69.1%) | 21 or (30.9%) |
| Girls | 36 (34.6%) | 5.13 ± 1.99 | 17 or (47.2%) | 19 or (52.8%) |
Table 1: Participants characteristics.
Even though the distribution of data does not depict a normal distribution, a lot can be inferred from the observed characteristics. A standard deviation of 2.31 shows that the data are primarily concentrated close to the mean of the sample, which is 6.27, and thus not widely dispersed.
In the study 36 (34.6%) girls and 68 (65.4%) boys (1:3) were enrolled, with the overall mean age of 6.3 years (range of 3 to 9 yrs), meaning patients were skeletally immature. In terms of fracture distribution per age, it was more common on children of six years and younger.
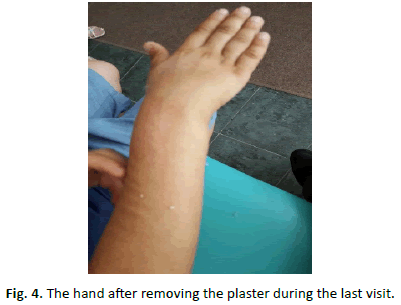
One patient presented with bilateral fracture. Sixty-four (64) fractures were of the right wrist (61.5%) and forty (40) fractures of the left wrist (38.5%). No patient had any other associated injury. Time interval between injury and reduction: in 97 patient’s reductions was done within a 1 hour after injury, and in 7 patients’ reduction was done 4 hours after injury (due to swelling and anesthesia team request). In delayed reduction, patients were placed in Chinese Fingers for traction and elevation, and cryotherapy was applied (Fig. 3 and 4).
As per quality of reduction, in 79% or 76% of patients an anatomic reduction has been achieved, in 12 or 11.5% (9 patients with 8° angulation and 3 with 5° angulation, no translation) a good reduction and in 7 or 6.7% (5 patients with no angulation and 2 mm translation, 2 patients with 10° angulation and no translation) of patients a fair reduction. In 6 patients or 5.8% we couldn’t do orthopaedic reposition, so it was done with open reduction fixation with 2 (Kirschneri) K- wires and plaster immobilization for 6 weeks.
The quality of reduction was fair in one patient (with delayed reduction of four hour from the injury). Re-reduction under fluoroscopy was needed in three patients on the third day of followup, after the swelling was reduced, all of them with: primarily good/ fair reduction (8° angulation; 10° angulation and no translation), slight displacement (>3 mm of translation; >5 degrees of radial deviation) and above 8 yrs old. The remained deformity was corrected, and the second cast was placed.
The frequency of reduction correction outcomes divides the data in two subsets: those of age 3-5 years old (Group I) and those of age 6-9 (Group II). Given the dispersion of the observations in the data set, children of age 6 do not pertain to any form of correct, namely “null”. Group I have resulted in 5 non-anatomic scenarios (elaborated below) whereas Group II has resulted in 3 non-anatomic scenarios. Nevertheless, out of the 5 cases in Group 1 none resulted in reduction correction (0%), whereas out of the 3 cases in Group 2 all 3 resulted in reduction correction (100%).
During the first two weeks after reduction, re-displacement occurred in none of the children. Above-elbow cast is removed after 2 weeks/3 weeks and replaced with well-molded below elbow cast for another 4 weeks (a circular in normal position). In re-reduction cases above-elbow cast is removed after 5 weeks and replaced with well-molded below-elbow cast for another 1 week. In the 17th day, 4 and 6 week’s follow-ups, no loss of reduction was noticed.
Patients were followed for at least 3 months. All forty-four patients achieved clinical and radiographic union with a full range of wrist motion.
Discussion
Forearm fractures are common injuries in childhood. They account for 45% of all fractures in children, mainly older than 5 years, with a peak incidence of distal forearm fractures occurring at ages 10 to 12 in girls and 12 to 14 in boys [13]. Blount noted that approximately 75% of fractures of the forearm are in the distal third, and that these almost never require open reduction and internal fixation [11]. Nevertheless, controversies still exist, with several other studies suggesting operative management as the appropriate way to deal with these fractures [14,15]. Additionally, increased risk of distal radius fracture has been noted in children with decreased bone mineral density and increased body mass [16].
85% of patients with displaced fractures achieve satisfactory results from closed reduction of the forearm, but a number of important principles should be followed: accurately align, both axially and rotationally, the distal fracture fragments with the proximal fragments and maintain this position until the fracture has healed [13].
Fractures of the distal radial metaphysis have great potential for remodeling because of their proximity to the distal growth plate [16]. Several studies have shown that complete remodeling does not always occur, especially in children older than 8 to 10 years [13].
Treatment of displaced or angulated fractures consists of closed reduction and immobilization in a molded three-point pressure plaster cast [16]. Well-molded sugar tong splints are an alternative [12].
The cast is molded with three-point pressure dorsally over the distal fragment, centrally on the volar surface of the forearm, and proximally on the dorsal surface of the forearm. This cast molding technique is designed to counter the tendency for later radial and dorsal fracture displacement. An above-elbow splint or bivalved cast is recommended for immobilization, but it has been demonstrated that a well-molded, below-elbow cast can also effectively stabilize these fractures [16]. The position of immobilization is determined by the position and rotational alignment of the proximal fragment. The fracture is immobilized in the position in which the alignment is correct, and the reduction feels stable [13].
Displaced or angulated bicortical fractures because the latter have a propensity for secondary angulation [16]. It is reported that 21% to 39% of fractures of distal radius in children can re-displace early after closed reduction [17]. Loose cast seems to be one of the main problems. A loose cast may be detected by radiography as can the possibility of angular deformation. It is important that the fracture be radiographed within a week after initial reduction [18,19].
Acceptable limits of reduction guidelines: In infants, <30° of angulation in the coronal plane - accepted. 5 - 10 years old, residual angulation is no greater than 15° to 20°. In children >10 years, <15° in the coronal plane and 10° of radial deviation [13].
Conclusion
Previous studies have analysed, as well as emphasized the importance of plaster cast immobilisation in the management of forearm fractures [20-24], whereas this study proved that closed reduction and immobilization of complete displaced forearm distal fractures in children younger than 9 years of age, results in satisfactory functional outcome. In fact, initial displacement and post reduction residual translation presents a statistically significant risk factor for re-displacement. We believe the reason behind this is that this group-age has more remodeling potential and greater acceptable reduction limit.
Another important factor behind this process is the regular follow up, especially the 3rd day regular control, when the possibilities for the re-displacement are obvious. This (our suggested) conservative method, ends up with lower costs and much more comfort.
Finally, our study (and its nature) has a couple limitations. Firstly, a greater sample size (perhaps) could have given stronger results, but due to the specificity of this condition (complete displaced forearm distal fractures) and its rarity amongst other similar fractures didn’t allow us to have more than 104 subjects within a period of 8 consecutive years (2009-2016). Secondly, the lack of previous supportive studies regarding this specific condition might have also affected the results, and therefore, further studies should be done to support our theory method of treatment.
Declarations
Ethics approval and consent to participate
Procedures performed in the study involving human participants were in accordance with the ethical standards of the national research committee (CEPI of the UCCK), Law No.03/L-172 on protection of personal data in the Republic of Kosovo and with the current version of the Declaration of Helsinki [19].
Before the intervention, every participant and his/her legal representatives were completely informed about each procedure, while an informed and singed consent was obtained in every case. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Consent for publication
Individual data were used in accordance with Law No.03/L-172 on protection of personal data in the Republic of Kosovo, while participants signed a consent form for the publication of their data (according to the current laws).
Availability of data and materials
The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
The whole study was performed in the Orthopedics and Trauma Clinic of the University Clinical Center of Kosovo in Prishtina, Kosova, which is a tertiary healthcare provider of public sector.
Authors’ contributions
SU conceived the study, participated in the study design, did the literature search, performed interventions and data collection, statistical analysis as well as drafted the manuscript. VP and OZ participated in performing the interventions, collecting the data and in the drafting of manuscript. MV participated in study design and in the drafting and critical revision of the manuscript.
DU, IB and KG were consulted on the statistical analysis and interpretation of data, participated in the drafting and critical revision of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to acknowledge the clinical and administrative staff in the Orthopedics and Trauma Clinic of the University Clinical Center of Kosovo in Prishtina where the interventions were done, as well as the honored professor Matjaz Veselko.
Trial registration Number
CEPIUCCK1035, Prospective trial, registered on 9th December 2008.
REFERENCES
- Cunnings S.R., Kelsey J.L., Nevitt M.C., et al.: Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985;7:178-208.
- O'Neill T.W., Cooper C., Finn J.D., et al.: Incidence of distal forearm fracture in British men and women. Osteoporos Int. 2001;12:555-558
- Abraham A., Handoll H.H.G., Khan T.: Intervention in treating wrist fractures in children. Cochrane Database Syst Rev. 2008;2:CD004576.
- Accabled F., Foster B.K.: Management of growth plate injuries. In: Children's Orthopaedics and Fractures, 3rd Ed. Benson M, Fixsen J, Macnicol M, Parsch K (Eds). Springer, London; 2010. p. 687-699.
- Lee B., Esterhai J.L., Das M.: Fracture of the distal radial epiphysis: Characteristics and surgical treatment of premature, post-traumatic epiphyseal closure. Clin Ortho Relat Res. 1984;185:90-96.
- Waters P.M., Bae D.S.: Fractures of the distal radius and ulna. In Rockwood and Wilkins' Fractures in Children, 7th edn. Beaty JH, Kasser JR (Eds). Lippincott Williams & Wilkins, Philadelphia 2010. p.292-346.
- Neil E., Green M.D., Marc F., et al. Skeletal trauma in children (3rd Ed, 2003, Saunders), Fractures of the forearm, Wrist, and Hand pg.186-224.
- Heckman J.D., Campbells operative orthopaedics 4 Volume Set 11th Edn. Part XI • Fractures and dislocations in children. 2008. pg.1546.
- Macnicol M.F., Parsch K.: Childrens Orthopedics and Fracture 3rd ed. 2010. Chapter 45: Wrist and Hand Fractures. p. 743.
- Alemdaroglu K.B., Iltar S., Çimen O., et al.: Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg. 2008;90A:1224-1230.
- Ozcan M., Memisoglu S., Copuroglu C., et al.: Percutaneous Kirschner wire fixation in distal radius metaphyseal fractures in children: Does it change the overall outcome? Hippokratia. 2010;14:265-270.
- Miller B.S., Taylor B., Widmann R.F., et al.: Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: A prospective, randomized study. J PediatrOrthop. 2005;25:490-494.
- Chivers D.A., Hilton T.L., Orth S.A.: An assessment of the three-point index in predicting the redisplacement of distal radial fractures in children. SA Orthopaedic Journal Winter. 2013;12.
- Dhoju D., Shrestha D., Parajuli N., et al.: Ipsilateral supracondylar fracture and forearm bone injury in children: A retrospective review of thirty one cases. Kathmandu Univ Med J (KUMJ). 2011;9:11-6.
- Ladenhauf H.N., Schaffert M., Bauer J. The displaced supracondylar humerus fracture: Indications for surgery and surgical options: a 2014 update. Curr Opin Pediatr. 2014;26:64-69.
- Morrissy R.T., Weinstein S., Lovell L.: Winter's Pediatric Orthopaedics, 6th edn, 33 - Management of fractures, distal metaphyseal fractures of the radius and ulna. 2007;p.1471-1473.
- Asadollahi S., Ooi K.S., Hau R.C.: Distal radial fractures in children: Risk factors for redisplacement following closed reduction. J Pediatr Orthop. 2015;35:224-228.
- Ogden J.A.: Skeletal injury in the child, 3rd edn. Springer-Verlag New York, Inc. Radius and Ulna, 2000; p. 621.
- World Medical Association. Declaration of Helsinki—Ethical principles for medical research involving human subjects. In: Proceedings of the 59th WMA General Assembly, Seoul, Korea, October 2008.
- Zamzam M.M., Khoshhal K.I.: Displaced fracture of the distal radius in children: Factors responsible for re-displacement after closed reduction. J Bone Joint Surg. 2005;87B:841-843.
- McLauchlan G.J., Cowan B., Annan I.H., et al.: Management of completely displaced metaphyseal fractures of the distal radius in children. A prospective, randomised controlled trial. J Bone Joint Surg Br. 2002;84:413-417.
- Voto S.J., Weiner D.S., Leighley B.: Redisplacement after closed reduction of forearm fractures in children. J Pediatr Orthop. 1990;10:79-84.
- Webb G.R., Galpin R.D., Armstrong D.G.: Comparison of short and long arm plaster casts for displaced fractures in the distal third of the forearm in children. J Bone Joint Surg Am. 2006;88:9-17.
- Chess D.G., Hyndman J.C., Leahey J.L., et al.: Short arm plaster cast for distal pediatric forearm fractures. J Pediatr Orthop. 1994;14:211-213.





 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.