Cemented hemiarthroplasty versus proximal femoral nail for neglected intertrochanteric femur fractures in the elderly at the philippine orthopedic center
2 Former President, Philippine Orthopedic Center, Philippine Hip and Knee Society, Philippines
Received: 01-Mar-2022, Manuscript No. jotsrr-22-55837; Editor assigned: 03-Mar-2022, Pre QC No. 22-55837(PQ); Accepted Date: Mar 26, 2022 ; Reviewed: 17-Mar-2022 QC No. 22-55837(Q);; Revised: 19-Mar-2022, Manuscript No. 22-55837(R); Published: 28-Mar-2022, DOI: DOI. 10.37532/1897-2276.2022.17(3).72
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Despite the advances in technique and implants available, the treatment of neglected, unstable, irreducible intertrochanteric fractures in the elderly remains to be a challenge. The purpose of this study is to compare the functional outcome, complication rate, revision rate and mortality rate between the use of cemented Bipolar Hemiarthroplasty (BPH) and Proximal Femoral Nail (PFN) in the treatment of neglected, unstable, irreducible intertrochanteric fractures in patients aged 65 years old and above. A total of 35 patients (17 for BPH, 18 for PFN) were gathered prospectively for this study. Results show that there was no difference in functional outcome, complication rate, and revision rate between the two groups. There was a higher amount of blood loss and more mortality in the BPH group. The use of cemented hemiarthroplasty is a viable option for the treatment of intertrochanteric fracture in elderly patients who have a higher amount of allowable blood loss and for patients compliant with necessary rehabilitation protocols. Given the distorted anatomy, it is more challenging to perform arthroplasty in intertrochanteric fractures. The level of skill required for this procedure is yet to be determined.
Keywords
Hemiarthroplasty, femur fracture, intertrochanteric femoral, proximal
Introduction
The treatment of unstable intertrochanteric femoral fracture in the elderly remains to be a challenge even in the present day. Patient factors such as poor bone quality, osteoporosis and concomitant medical co-morbidities contribute to a high incidence of complications associated with internal fixation of unstable intertrochanteric fractures in the elderly. Such complications may include excessive collapse, loss of fixation and lag screw cut-out. In the attempt to reduce these complications, the use of arthroplasty has been suggested; however, literature on arthroplasty for unstable intertrochanteric fractures in the Philippine setting is limited. The purpose of this study is to compare the functional outcome, complication rate, revision rate and mortality rate between the use of cemented hemiarthroplasty and proximal femoral nail in the treatment of unstable, irreducible neglected intertrochanteric fractures.
Intertrochanteric fractures are extracapsular fractures of the proximal femur involving the greater and lesser trochanter. Stable fractures have an intact posteromedial cortex. Unstable fractures included the following: comminution of the posteromedial cortex, a thin lateral wall (less than 20.5 mm), displaced lesser trochanteric fracture, subtrochanteric extension and reverse obliquity fractures [1]. Irreducible fractures were determined by failure to achieve adequate reduction after closed manipulation. The etiology of an irreducible pattern was interposed soft tissue, more commonly the psoas tendon [2]. Tronzo described an irreducible pattern in that the lesser trochanter is bisected and the lesser trochanter tendon remains attached to the proximal fragment [3]. Open reduction was required for these types of fractures. Despite the success of utilizing internal fixation for the treatment of intertrochanteric hip fracture, failure rates have been reported to be as high as 56% in association with unstable fractures in elderly patients. According to Bonamo, the poor mechanical properties of the weak and porotic bone in these elderly patients do not usually provide a firm purchase for the screws leading to early biomechanical failure. Poor bone purchase can lead to collapse, varus malalignment and retroversion, resulting n shortening and decreased abductor muscle lever arm. To avoid these complications and subsequent revision surgery, especially in the elderly population, arthroplasty has been utilized.
Several studies such as those written by Kumar have found results favourable for use of hemiarthroplasty even in unstable, osteoporotic patients. Clinical outcomes of these studies are based on the functional outcome using the Harris Hip Score and prevention of recumbency complications [4-6].
Given the available information on the functional outcome of hemiarthroplasty in intertrochanteric fractures, the study aims to provide clinicians with more information in assessing the use of such a procedure. By analyzing the functional outcome, complications, revision rate and mortality rate that can be attributed to the said procedure, clinicians can weigh potential benefits against possible risks [7-9].
Materials and Methods
This is a prospective analytical cohort study. The primary objective of the study is to determine and compare the functional outcome, complication rate, revision rate and mortality rate between the two treatment groups.
A total of 35 patients with unstable intertrochanteric fractures, were gathered via convenience sampling. These patients were admitted to the Philippine Orthopedic Center and balanced skeletal traction was applied in the affected limb. Upon admission, patients were referred to consultants who determined whether patients should undergo hemiarthroplasty or proximal femoral nail. In our hospital setting, delay in surgery is often encountered due to the procurement of implants, diagnostics and blood transfusion units. The average duration from admission to surgery was 32 days, the earliest being 14 days while the most delayed was 67 days. No patient developed Deep Vein Thrombosis (DVT) pre-operatively. Not all patients were started on DVT prophylaxis medications as the decision was based on the suggestion of the internal medicine specialist. Informed consent for the study was required of the patients.
The inclusion criteria for the study are the following:
1. Unstable intertrochanteric fractures
2. Irreducible by closed reduction
3. Independently mobile prior to injury
4. Age 65 years old and above
5. More than 2 weeks post-injury
6. Fit for surgery
The intertrochanteric fracture was determined to be unstable by the main author with the following radiographic parameters; comminution of the posteromedial cortex, a thin lateral wall (less than 20.5 mm), displaced lesser trochanteric fracture, subtrochanteric extension and reverse obliquity fractures. These included AO Classification 31 A2 and A3 fractures. Fractures were determined to be irreducible by closed reduction maneuvers with or without the use of a fracture table.
The exclusion criteria include the following:
1. Polytrauma
2. Patient unfit for surgery.
3. Previous hip surgery
To estimate the minimum sample size for this prospective cohort study, the difference in proportions formula is used:
The following parameters were set: Power=80%;
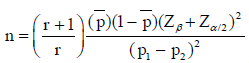
Level of significance = 5%, and ratio of sample size=1. According to literature, certain unstable fracture patterns treated with internal fixation have been reported to have failure rates as high as 56%, while patients who underwent bipolar hemiarthroplasty had 10% failure rates Substituting the given parameters in the formula, the computed minimum number of participants is n=34, with a minimum number of patients for internal fixation=17, and a minimum number of patients for hemiarthroplasty=17.
18 patients were treated with proximal femoral nail (PFN). Surgery was performed by either an orthopaedic resident or a consultant. 7 were performed by residents, 11 by consultants. Patients were placed supine with the use of a fracture table. Open reduction was performed through a direct lateral approach to the hip. Exposure and identification of the fracture pattern were done, followed by gentle osteoclasis. Fractures edges were freshened. Reduction was achieved with use of K-wires as joysticks/ temporary fixation, Schanz pins to manipulate bigger fragments, and bone hook/ tenaculum/ collinear clamp to reduce the shaft. Once an adequate reduction was achieved, a proximal femoral nail with a helical blade was used for final fixation. Post-operatively, patients are allowed passive and active range of motion exercises and toe-touch weight bearing with assistance. Weight bearing was gradually progressed for each succeeding follow-up.
17 patients were treated with the cemented bipolar hemiarthroplasty. Fellowship-trained arthroplasty surgeons performed the surgery. Patients were placed on lateral decubitus position. Either a MIS posterior or Kocher-Langenback approach would be utilized. Intraoperatively, there were no noted chondral defects nor arthritic changes observed in the acetabulum. A cemented bipolar hemiarthroplasty was used for replacement. Post-operatively, patients are instructed hip dislocation precautions by avoiding flexion past 90 degrees, adduction and internal rotation of the hip. Patients are allowed immediate weight bearing as tolerated with assistance and supervision.
During surgery, the following data were collected:
1. Amount of blood loss.
2. Operative time as recorded by the anesthesiologist.
3. Incidence of iatrogenic fractures.
4. Incidence of malreduction.
After surgery, patients were monitored at 1 week, 1 month, 3 months, 6 months and 1 year post-operatively. The following will be noted during follow-up: incidence of iatrogenic fracture, malalignment, infection, complications requiring revision surgery. The reduction of the fracture was considered anatomical (<5 degrees of varus/valgus/ anterversion/retroversion), acceptable (5 to 10 degrees), or poor (>10 degrees). Any erosion of the acetabular cartilage with horizontal or vertical migration of the bipolar cup of >2 mm was documented. A stem was considered to be unstable if there is noted subsidence exceeding 3 mm, any change in position or a continuous radiolucent line wider than 2 mm at the bone-cement interface. A total number of complications were tallied per treatment group. Harris Hip Score was evaluated at 1-year post-op to determine the functional outcome. Weeks until independent ambulation on level surfaces were also recorded. Independent ambulation on level surfaces is defined as the ability to do full weight-bearing for more than 10 feet without the need for supervision nor physical assistance from another person. Assistive devices are allowed. A number of patients who underwent revision surgery and a number of mortalities were also recorded.
Summary statistics were reported as mean and standard deviation (SD) for continuous data with normal distribution, as median and interquartile range (IQR) or range for skewed continuous data and discrete quantitative data, and as count and percent for qualitative measures. Minimum and maximum values of continuous data were also reported.
Shapiro-Wilks test was used to determine if continuous variables deviate from normal distribution. Chi-square test, Fisher’s exact test or Yate’s chi-square test were used to compare proportions. Pairwise comparison of proportions was based on Bonferroni adjusted pvalues. Independent t-test or Mann-Whitney U test was used to compare the mean between cemented hemiarthroplasty vs. proximal femoral nail. A median test was also used to compare the median between the two procedures. Complication and mortality rates with 95% confidence intervals were also reported. Statistical significance was based on p-value ≤ .05. STATA version 15 (Stata Corp LLC, College Station, TX, US) was used in data processing and analysis.
Results
Out of 35 elderly patients, the mean age was 77.8 years, range from 65 to 95 years. The majority were women (85.7%). There were 68.6% with at least one comorbidity, the most common of which was hypertension (42.9%). Most of the elderly patients were non-smokers (91.4%). There were 65.7% who had home ambulators and 34.3% used community ambulators. The total median time to surgery was 36 days, range from 24 to 65 days. These patients were treated for unstable, irreducible neglected intertrochanteric femur fracture using either cemented hemiarthroplasty (48.6%) or proximal femoralnail (51.4%). Comparisons between these two procedures showed longer time to surgery in the cemented hemiarthroplasty group than proximal femoral nail (42 vs. 32 days, p=0.028). However, there was insufficient evidence of significant differences between the two groups with respect to age, sex, past medical history, smoking history, and pre-injury ambulation (Table 1).
Table 1. Demographic data, mortality and PROMs of the three cohorts of hip replacements
| Characteristic | All Patients | Proximal femoral nail | Cemented hemiarthroplasty | p-value |
|---|---|---|---|---|
| Age, years | 77.8 ± 7.5 | 76.4 ± 8.8 | 79.2 ± 5.8 | 0.267 |
| Sex | ||||
| Male | 5 (14.3%) | 3 (16.7%) | 2 (11.8%) | 0.944 |
| Female | 30 (85.7%) | 15 (83.3%) | 15 (88.2%) | |
| Past medical history | ||||
| Any medical illness | 23 (65.75) | 12 (66.7%) | 11 (64.7%) | 0.815 |
| Hypertension | 15 (42.9%) | 7 (38.9%) | 8 (47.1%) | 0.738 |
| Diabetes mellitus | 7 (20.0%) | 3 (16.7%) | 4 (23.5%) | 0.691 |
| Others | 8 (22.9%) | 4 (22.2%) | 4 (23.5%) | 0.755 |
| Smoking history | ||||
| Non-smoker | 32 (91.4%) | 16 (88.9%) | 16 (94.1%) | 0.486 |
| Former | 1 (2.9%) | - | 1 (5.9%) | |
| Current | 2 (5.7%) | 2 (11.1%) | - | |
| Pre-injury ambulation | 0.075 | |||
| Community ambulator | 12 (34.3%) | 9 (50.0%) | 3 (17.6%) | |
| Home ambulator | 23 (65.7%) | 9 (50.0%) | 14 (82.4%) | |
| Days to surgery | 36 (14) | 32 (9) | 42 (16)† | 0.028 |
| Data are mean ± SD or count (%) on 35 elderly patients, 18 treated with proximal femoral nail and 17 treated cemented hemiarthroplasty. Other past medical history at one reported case each included bronchial asthma, gout, hypercholesterolemia and thyroid disease among those treated with cemented hemiarthroplasty, and cervical cancer, emphysema, heart disease, and pulmonary tuberculosis among those treated with proximal femoral nail. | ||||
The total median blood loss was 800 cc, ranging from 200 to 2,700 cc. Comparison between the two procedures showed higher median blood loss among those treated using cemented hemiarthroplasty than those using proximal femoral nail (950 vs. 550 mL, p=0.004).
All except three patients (91.4%) treated using the proximal femoral nail required blood transfusion. The total median number of blood bags used for transfusion was two bags, ranging from none to five bags. Although the median number of blood bags were comparable between the two procedures, a higher proportion of those treated using cemented hemiarthroplasty needed three to five blood bags for transfusion (23.5% vs. 0%, p =0.016). The total median duration of surgery was 120 minutes, ranging from 50 minutes to 340 minutes. The median duration between the two groups, however, was comparable (Table 2).
Table 2. Intraoperative parameters
| Parameter | All Patients | Proximal femoral nail | Cemented hemiarthroplasty | p-value |
|---|---|---|---|---|
| Blood loss, cc | 800 (500) | 550 (363) | 950 (325)‡ | 0.004 |
| Blood bags transfused | 2 (5) | 1 (2) | 2 (4) | 0.098 |
| 0 | 3 (8.6%) | 3 (16.7%) | - | 0.016 |
| 44563 | 28 (80.0%) | 15 (83.3%) | 13 (76.5%) | |
| 44625 | 4 (11.4%) | - | 4 (23.5%)† | |
| Operating time, min | 120 (45) | 120 (60) | 110 (45) | 0.815 |
| Data are median (range) on 35 elderly patients, 18 treated using proximal femoral nail and 17 using cemented hemiarthroplasty. ‡ P < .01 vs. proximal femoral nail † P < .05 vs. proximal femoral nail |
||||
Complication rate was 31.4% (95% CI: 16.8% to 49.3%). The rates of complication were 27.8% and 35.3% in the cemented hemiarthroplasty and proximal femoral unit groups, respectively. Comparisons between these two procedures showed comparable rates. Reported complications included intraoperative periprosthetic fractures that were reported in three cases (8.6%): two (11.8%) in the cemented hemiarthroplasty group and one in the proximal femoral nail group (5.6%). A total of three cases of varus malalignment (8.6%) were reported after one week from surgery and these patients were treated using the proximal femoral unit. Two cases of bedsore (11.8%) after cemented hemiarthroplasty and one case of pressured heel sore (5.6%) were also reported after surgery using a proximal femoral nail. There was, however, insufficient evidence of significant differences in the incidences of these complications between the two groups. Total mortality rate was 11.4% (95% CI: 3.2% to 26.7%). Three death cases (17.6%) were reported in the cemented hemiarthroplasty group and one in the proximal femoral unit group (5.6%). Death rates between the groups were also comparable. The known cause of death for one case was ascending cholangitis one month after surgery and another due to community-acquired pneumonia six months after surgery using cemented hemiarthroplasty. None of the patients requiring revision surgery had undergone the secondary procedure. The mean Harris hip score at one-year post-surgery was 72.1 points, ranging from 46.2 to 99.7 points. The majority had scores ranging from 71.2 to 79.5 suggesting a fair outcome. Comparison of scores between the two procedures showed insufficient evidence of significant differences. The median time to independent ambulation on level surfaces was 6 weeks, ranging from two weeks to six months. Comparisons also showed that time to independent ambulation was comparable between the two procedures (Table 3).
Table 3. Surgical outcome of elderly patients
| All Patients | Proximal femoral nail | Cemented hemiarthroplasty | p-value | |
|---|---|---|---|---|
| Complication | ||||
| Any complication | 11 (31.4%) | 5 (27.8%) | 6 (35.3%) | 0.632 |
| Intraoperative periprosthetic fracture | 3 (8.6%) | 1 (5.6%) | 2 (11.8%) | 0.603 |
| Varus malalignment | 3 (8.6%) | 3 (16.7%) | - | 0.229 |
| Bedsore/pressure heel sore | 3 (8.6%) | 1 (5.6%) | 2 (11.8%) | 0.603 |
| Death | 4 (11.4%) | 1 (5.6%) | 3 (17.6%) | 0.338 |
| Harris Hip Score | 72.1 ± 11.1 | 73.7 ± 9.8 | 70.1 ± 12.5 | 0.372 |
| Poor (<70) | 11 (35.5%) | 5 (29.4%) | 6 (42.9%) | 0.572 |
| Fair (70-79) | 16 (51.6%) | 10 (58.8%) | 6 (42.9%) | |
| Good (80-89) | 1 (3.2%) | - | 1 (7.1%) | |
| Excellent (90-100) | 3 (9.7%) | 2 (11.8%) | 1 (7.1%) | |
| Weeks to independent ambulation on level surfaces | 6 (5) | 4 (4) | 8 (8) | 0.715 |
| Data are count (%), mean ± SD or median (IQR) on 35 elderly patients, 18 treated using proximal femoral nail and 17 using cemented hemiarthroplasty. | ||||
Discussion
This study was able to show no difference in complication rate between patients treated with PFN and cemented hemiarthroplasty in the treatment of unstable intertrochanteric fractures. The majority of the complication from PFN was primary varus malalignment and intra-operative iatrogenic fracture. There was no incidence of loss of reduction, implant failure, infection, non-union or other complications requiring revision surgery. The varus malalignment can be attributed to the delay in the surgery of more than 3 weeks wherein abundant callus developed between the fracture fragments. In these cases, difficulty was encountered in achieving adequate reduction between fracture fragments. There was also a case of intra-operative iatrogenic fracture distal to the tip of the nail. This can be attributed to a posterior entry point, causing a fracture in the anterior cortex upon nail insertion. In this case, a long nail was used to bypass the iatrogenic fracture. Roberts noted that impingement and penetration of the anterior femoral cortex may occur during nail insertion in shorter patients, use of long hip nails, and inappropriate entrypoint [10].
There was 2 case of intraoperative iatrogenic fracture in the hemiarthroplasty group. According to Barlas, intraoperative fractures during hemiarthroplasty can be caused by intrinsic and extrinsic factors. Intrinsic factors include poor bone stock, advanced age, female gender, abnormal femoral geometry, biomechanical factors, patient compliance, and thinning of the femoral cortex with a smaller proximal canal/neck flare. Extrinsic factors include the use of a straight rather than bowed or so-called anatomic stem, stem diameter, the surgical approach, and under-reaming instead of line-to-line reaming for implantation of bowed stems [11]. For this study, their iatrogenic fracture occurred during broaching. The intra-operative fractures can be attributed to the abnormal femoral geometry brought about abundant callus between displaced fracture fragments. In one case, there was an anterior translation of the proximal fragment over the main distal fragment and in the other, the proximal fragment was displaced laterally to the main distal fragment. There was no incidence of dislocation, loosening or infection. There was no statistical difference in functional outcome between the two treatment groups as reflected from the Harris Hip Scores. The average duration of independent ambulation for the hemiarthroplasty group was 7.6 weeks while for the PFN group, 6.7 weeks. Theoretically, hemiarthroplasty has the advantage of allowing earlier weightbearing. However, a number of patients were not compliant with their rehabilitation protocol and refused weight-bearing. Three patients reported that there was a delay in weight-bearing due to the postoperative pain. There was 1 patient who developed bedsore from prolonged immobilization.
There were also 3 mortalities in the hemiarthroplasty group and 1 mortality in the proximal femoral nail. These patients did not expire during their admission to our hospital. The mortalities were discovered as we contacted the relatives by phone. The exact cause of death of these patients cannot be accurately retrieved as we do not have access to the medical records of other hospitals. The alleged cause of death was extracted from interviewed relatives. A study by Huang reported the use of hemiarthroplasty for intertrochanteric fracture led to more post-operative complications which were most pulmonary infections, cerebral infarction and heart failure [12]. Our study showed that mortalities in the hemiarthroplasty group were attributed to pulmonary infection and ascending cholangitis.
Overall, there was a higher amount of blood loss in the arthroplasty group. There was also no significant difference in operative time. A meta-analysis by Chen comparing hemiarthroplasty with PFN also showed similar results where there was no significant difference in HHS, post-operative orthopaedic complications and postoperative medical complications. The same study also noted more blood loss in the hemiarthroplasty group [13].No patient in either treatment groupunderwent revision surgery. This study is limited to its smaller sample size. More statistical data could have been gathered from a bigger sample size. The hemiarthroplasty was performed by fellowship-trained arthroplasty surgeons. The level of skill required in performing arthroplasty in intertrochanteric fractures could be assessed in future studies. Mortalities could have been further investigated if access to patients’ medical records from other hospitals were granted.
Conclusion
When comparing the use of cemented hemiarthroplasty and proximal femoral nail in unstable intertrochanteric fractures, there was no statistical difference in complication rate, Harris Hip Score at 1-year post-op, operative duration and revision rate. There was more blood loss in the hemiarthroplasty group. There were also more mortalities in the hemiarthroplasty group. The use of cemented hemiarthroplasty is a viable option for the treatment of intertrochanteric fracture in elderly patients who have a higher amount of estimated allowable blood loss and for patients compliant with necessary rehabilitation protocols. Given the distorted anatomy, it is more challenging to perform arthroplasty in intertrochanteric fractures. The level of skill required for this procedure is yet to be determined.
REFERENCES
- Attum B, Pilson H.: Intertrochanteric Femur Fracture. StatPearls Treasure Island (FL): StatPearls Publishing; 2021
Google scholarCrossref - Moehring H.D., Nowinski G.P., Chapman M.W., et al.: Irreducible intertrochanteric fractures of the femur. Clin Orthop Relat Res. 1997; 339:197-9
Google scholarCrossref - Tronzo R.G.: Symposium on fractures of the hip. Special considerations in management. Orthop Clin North Am. 1974; 5:571-583
Google scholarCrossref - Kumar K., Sanjay M., Vijaya K.N., et al.: Bipolar Hemiarthropasty in Unstable Intertrochanteric Fractures In Elderly: A Prospective Study. J Clin Diagn Res. 2013; 7: 1669-1671
Google scholarCrossref - Khaldoun S., Mazen S., Julien G., et al.: The effectiveness of primary bipolar arthroplasty in the treatment of unstable intertrochanteric fractures in elderly patients. N AmJ Med Sci. 2010; 2: 561-568
Google scholarCrossref - Kim S.Y., Kim Y.G., Hwang J.K., et al.: Cementless calcar-replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures. A prospective randomized study. J Bone Joint Surgery Am. 2005; 87: 2186-2192
Google scholarCrossref - Nadir O., Okcu G., Aktuglu K.: Intertrochanteric femur fractures in the elderly treated with either proximal femur nailing or hemiarthroplasty: A prospective randomised clinical study. Injury. 2015; 2: S3-S8
Google scholarCrossref - Hayrettin K., Tahir O., Bilgili M.G., et al.: Treatment of intertrochanteric femur fractures in elderly patients: internal fixation or hemiarthroplasty. Acta Orthop Traumatol Turc. 2005; 39: 287-294
Google scholarCrossref - Nie B., Wu D., Yang Z., et al.: Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly. Medicine. 2017; 96
Google scholarCrossref - Roberts J.W., Libet L.A., Wolinsky P.R.: Who is in danger? Impingement and penetration of the anterior cortex of the distal femur during intramedullary nailing of proximal femur fractures: preoperatively measurable risk factors. J Trauma Acute Care Surg. 2012; 73: 249-254
Google scholarCrossref - Barlas K.J., Ajmi Q.S., Bagga T.K. et al.: Association of Intra-Operative Metaphyseal Fractures with Prosthesis Size during Hemiarthroplasty of the Hip. J Ortho Surg. 2008; 16: 30-4
Google scholarCrossref - Huang J., Shi Y., Pan W. et al.: Bipolar Hemiarthroplasty should not be selected as the primary option for intertrochanteric fractures in elderly patients. Sci Rep. 2020; 10: 4840
Google scholarCrossref - Chen J., Yue C., He P., et al.: Comparison of clinical outcomes with hip replacement versus PFNA in the treatment of intertrochanteric fractures in the elderly. Medicine. 2021; 100: e24166
Google scholarCrossref



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.