A rare case of sequential tendon rupture in a patient with alkaptonuria with ochronotic arthropathy of knee joint
Received: 11-Oct-2022, Manuscript No. jotsrr-22- 76946; ; Editor assigned: 12-Oct-2022, Pre QC No. jotsrr-22- 76946 (PQ);; Accepted Date: Nov 08, 2022 ; Reviewed: 26-Oct-2022 QC No. jotsrr-22- 76946 (QC);; Revised: 03-Nov-2022, Manuscript No. jotsrr-22- 76946 (R);; Published: 09-Nov-2022, DOI: 10.37532/1897- 2276.2022.17(10).72
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Sequential rupture of tendon is a rare condition. We describe a case of 46-year-old male with previous history of bilateral tendo-Achilles tear presents with right side quadriceps tendon rupture. Alkaptonuria is a rare autosomal recessive disorder characterized by the absence of homogentisic acid oxidase enzyme. excessive accumulation of homogentisic acid causes Arthropathy and tendinopathy in musculoskeletal system and also affect multiple organ system.
Keywords
Spondyloarthritis, non-radiographic, NSAID, DMARD, HLA-B27.Introduction
Alkaptonuria is a rare inherited genetic disease which is caused by deficiency of Homogentisic Acid Oxidase (HGA) enzyme. This enzyme causes metabolism of homogentisic acid, a metabolic product of aromatic amino acids phenylalanine and tyrosine [1]. The condition is rare, affecting only 1 in 100,000 to 250,000 individuals. The HGA is excreted abundantly in the urine of these patients. Even so, there are elevated circulating levels of HGA in the blood and body tissues [2].
Deficiency will lead to accumulation of homogentisic acid in blood and tissues which affects hyaline cartilages, skin, sclera, tendon, joints and intervertebral disc. It is also associated with decreased bone mineral density. The c ondition a lso a ffects re spiratory sy stems, ge nitourinary and cardiovascular systems. The polymer, named as Ochronotic pigment which is also called Ochronosis, affects the hyaline cartilage especially the weight bearing joints like knee [3]. Ochronotic arthritis often begins in the third decade. Ultimately joint replacement is needed, on average, this occurs at the age of 55 years [4]. Progressive Ochronotic arthritis always shows articular space narrowing, bone sclerosis, and effusion [5]. These ruptures tend to occur in older age groups typically more than 40 years of age. In older patients the rupture typically occurs at the osseo-tendinous junction while in younger patients, it is more often at the mid-tendinous area [6]. We report a case who had a Sequential tendo Achilles tendon rupture followed by right side quadriceps tendon rupture 10 years later. The hallmark of disorder is a Ochronotic pigmentation, degenerative arthritis and urine that turns black on alkalinisation. Spontaneous quadriceps rupture has been described in patient with chronic disease such as diabetes mellitus, obesity, gout, ontogenesis imperfecta, hyperparathyroidism, Alkaptonuria amyloidosis and SLE.
Case Report
A 46-year-old male presented to the Orthopaedic Department of our hospital with chief complaints of pain and swelling in the right knee with difficulty in walking since 1 week. He has a history of fall from bike 1 week back and was unable to climb stairs and unable to stand from sitting position. Patient had past history of right side tendo Achilles tear 11 years back followed by left side tendo Achilles tear 9 months after first event (Figure 1).
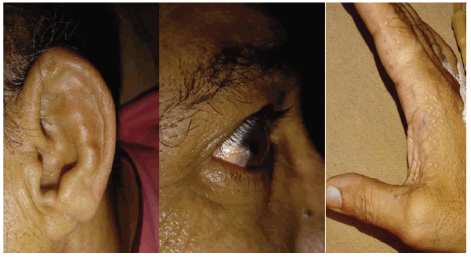
Where on evaluation we found that his father was operated for disc prolapse and there was a blackish discoloration of disc material and his grandmother has a Ochronotic pigmentation in sclera and pinna of ear (Figure 2).
A diagnosis of Alkaptonuria was suspected, history of darkening of urine on standing was present.
Following tests were performed:
1. Urine turns dark on standing in air for few hours.
2. Urine benedict’s test: urine turns black on adding benedict’s reagent and on heating slowly, a greenish yellow precipitate was formed which also turned black after few hours of standing. Therapeutically vitamin C as an antioxidant was started for degradation of homogentisic acid. Aim of the treatment is to prevent the destruction of cartilage, arthritis. Physical examination revealed grossly swollen knee joint and a palpable gap identified just above the patella and patient was not able perform active straight leg raising
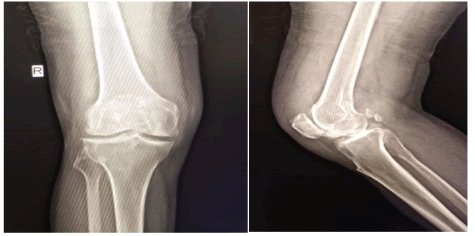
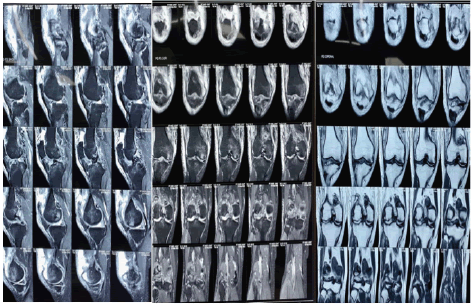
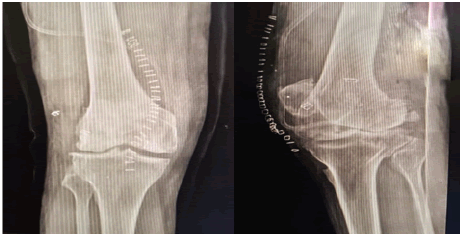
On X- Ray there is evidence of osteophytes with loose body formation, quadriceps tendon avulsion, osteoarthritis with narrowing of joint space and subchondral sclerosis (Figure 3). On Magnetic Resonance Imaging (MRI) of right knee showed quadriceps tendon rupture at osseo-tendinous junction and swollen diffuse degenerative changes of cartilage and both meniscus with osteophytes and multiple loose bodies (Figure 4).
ARTHROSCOPY
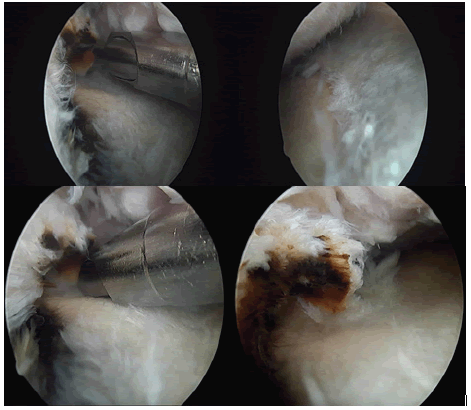
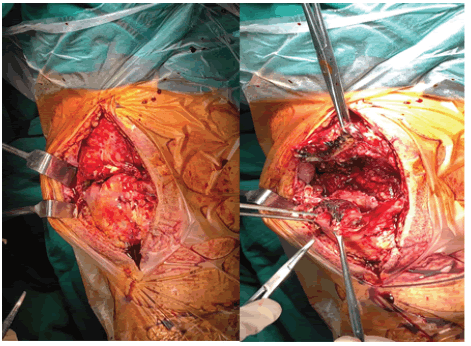
Diagnostic arthroscopy of right knee was performed on 7th post traumatic day with standard anteromedial and anterolateral portal. On examination there was a quadriceps tendon rupture and large loose body in intercondylar notch in front of Anterior cruciate ligament, measuring about 5×6 mm in size. There was a degenerative tear of both menisci with loss of elasticity with blackish discoloration of both menisci and also at the Attachment Sites of Ligaments (ACL, PCL). We arthroscopically removed loose bodies and performed a partial meniscectomy of both meniscus (Figure 5).
QUADRICEPS TENDON REPAIR
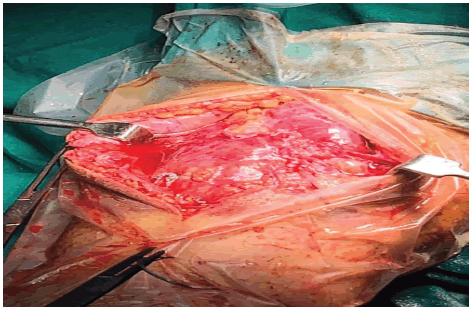
A lazy S shaped incision of 6 cm - 8 cm taken at the anteromedial aspect of knee joint. After subcutaneous dissection upto the tibial tuberosity, exposing the quadriceps tendon, retinaculum and patellar tendon. Quadriceps tendon rupture identified. On dissection there was a blackish discoloration at the both avulsed ends and there was thickening of distal quadriceps tendon closed to the patellar attachment site (Figure 6).
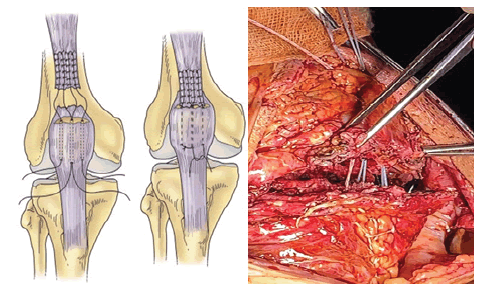
We used arthroscopic burr and battery operated saw to remove all the black deposit at the ruptured end and created bleeding surface for the better healing, there was a 2 cm-3 cm proximal retraction of ruptured stump but we could able to mobilize it till the superior pole of patella without tension. There was a small bony fragment attached at the distal end of Quadriceps tendon. We used size 2 fiber wire with needle (Anthrax, Naples, USA) of different colours (2 violates and 1 blackwhite) to put 3 columns of multiple locking running stitches in U shape fashion with separate entry and exit points from distal to proximal about 4 cm in the tendinous portion of the quadriceps. Then we flexed the knee joint and use patella holding clamp to control the patella while making 3 transosseous tunnel of 2.5 mm size in medial, central and lateral aspect of patella without damaging patellar tendon. (Figure 7) [7].
The proximal entry point of transosseous tunnels is 3 mm Anterior to the articular margin of patella and distal exit point is anterior surface of lower pole of patella near patellar tendon attachment. We used 18 no. spinal needle with a loop of 1-0 ethilon (Ethicon, J&J,USA) as a suture shuttle to pull the size 2 fiber wire through the patellar transosseous tunnels distally. Before tying knots we confirmed approximation of torn ends by pulling sutures distally. Knots tying done keeping a bone bridge by taking one fiber wire suture from medial and lateral tunnels. Finally sutures from central tunnel tied with fiber wire of medial and lateral tunnel. Simple half hitches knot (7 knots are tied for each suture) taken. At the end of procedure, we confirmed water tight repair by passing inflow cannula through the anterolateral portal (Figure 8)
On Histopathological examination of resected portion of tendon showed disposition of pigment within and outside the cells in the tissue. Post operatively knee was immobilized with the above knee brace in full extension. We started knee range of motion exercise (closed chain) and will achieve full knee flexion within 7-8 weeks. We advised patient to have non weight bearing ambulation immediately after surgery for six weeks (Figure 9).
Discussion
A deficiency of the hepatic enzyme Homogentisate 1,2-Dioxygenase (HGO) forces the accumulation of homogentisic acid, which is rapidly cleared in the kidney and excreted1.Production of large quantities of HGA daily in the urine, turns it dark on standing [8,9]. In urine, as in tissues, HGA oxidizes to benzoquinones, which in turn form melanin like polymers. Accumulation of HGA and its metabolites in tissues causes ochronosis, with darkening of cartilaginous tissues and bone, arthritis and joint destruction, and deterioration of cardiac valves [8].There is no effective therapy for this disorder, although nitisinone inhibits the enzyme that produces HGA [10]. Therapy could a lso b e a chieved with the use of antioxidants such as ascorbic acid since reducing HGA oxidation could increase urinary excretion of HGA [11]. Furthermore, ascorbic acid has been shown to inhibit HGA polyphenol oxidase, with a consequent decrease in Benzoquinone Acetic Acid (BQA) synthesis, a product of the oxidation of Homogentisic Acid (HGA) that causes tissue injury [12].
Alkaptonuria Arthropathy, the only disabling effect of the disease, is due to brittleness and fragmentation of the articular cartilage, which also causes a non-specific synovitis of the affected joints. The spine and major weight-bearing joints are most commonly affected and symptoms usually start by the fourth decade [13-15].
The numerous reports on Alkaptonuria are limited to degenerative manifestations in joints, but there are no reports of the effects of the deposition of homogentisic acid in tendons leading to spontaneous rupture. Homogentisic acid is widely deposited in connective tissue and such pigmentation must include tendons, which contain mainly Type-I collagen. The accumulation of homogentisic acid inhibits collagen crosslinking leading to reduction of the structural integrity of collagen [16]. Thus increasing the likelihood of spontaneous rupture. There is no specific treatment for Alkaptonuria
Arthropathy; it includes physiotherapy, analgesia, and rest. Reduction of tyrosine and phenylalanine in the diet has been reported to reduce the excretion of homogentisate. It is not known whether dietary restriction from early life would avoid or minimise later complications, but such an approach is reasonable. Vitamin C, up to 1 g/day, is recommended for older children and adults. The mild antioxidant nature of ascorbic acid helps to retard the conversion of homogentisate to the polymeric material which is deposited in the cartilaginous tissues. Genetic advances offer hope that corrective measures are forthcoming. Of note, in a murine model of Alkaptonuria, 2(2 nitro-4 trifluoromethylbenzoyl)1,3- cyclohexanedione (NTBC) was a potent inhibitor of hydroxyl phenyl pyruvate dioxygenase, which catalyses the formation of homogentisic acid. Development of the active compound may result in the first pharmacotherapeutic agent for this metabolic disease [17,18].
Conclusion
Ochronosis is a rare metabolic disease leading to orthopaedic complications like tendon rupture, osteoarthritis and back pain. Prophylactic therapy may reduce the complications by a combination of protein restricting diet, ascorbic acid. We decided to report this case because he presented with Sequential rupture of both tendo Achilles and right sided quadriceps tendons. Ultimate goal of treatment may be using genetic engineering to replace the missing homogentisic acid oxidase enzyme. Its always better to keep these patients informed about possible consequences of disease and regular follow up required for early detection and treatment of any musculoskeletal problems.
References
- Jarrod AE, Oxon MD. The incidence of Alkaptonuria: a study in chemical individuality. The Lancet 1902:161-20. [Google Scholar][CrossRef]
- Hallowell TR, Gallagher JA, Ranganath L. Alkaptonuria: a review of surgical and autopsy pathology. Histopathology 2008;53:503-12. [Google Scholar][CrossRef]
- Taylor AM, Boyde A, Wilson PJ, et al. The role of calcified cartilage and subchondral bone in the initiation and progression of Ochronotic Arthropathy in Alkaptonuria. Arthritis Rheum 2011;63:3887-96. [GoogleScholar][CrossRef]
- Gil JA, Wawrzynski J, Waryasz GR. Orthopedic manifestations of ochronosis: pathophysiology, presentation, diagnosis, and management. Am J Med 2016;129:536.e1-6. [Google Scholar] [CrossRef]
- Mannoni A, Selvi E, Lorenzini S, et al. Alkaptonuria, ochronosis, and ochronotic arthropathy. Semin Arthritis Rheum 2004;33:239-48. [Google Scholar] [CrossRef]
- Rasul Jr AT, Fischer DA. Primary repair of quadriceps tendon ruptures. Results of treatment. Clin Orthop Relat Res Apr 1993(289):205-7. [Google Scholar][CrossRef]
- McNeilan RJ, Flanigan DC. Quadriceps Tendon Ruptures. In Hamstring Quadriceps Inj Athl. 2014, 103-19. [Google Scholar][CrossRef]
- La Du BN, Zannoni VG, Laster L et al. The nature of the defect in tyrosine metabolism in alkaptonuria. J Biol Chem 1958; 230: 251-60. [Google Scholar] [CrossRef]
- O'Brien WM, La Du BN, Bunim JJ. Biochemical, pathologic and clinical aspects of alkaptonuria, ochronosis and ochronotic arthropathy: review of world literature (1584-1962). Am J Med 1963;34:813-38. [GoogleScholar][CrossRef]
- Phornphutkul C, Introne WJ, Perry MB, et al. Natural history of alkaptonuria. N Engl J Med 2002; 347: 2111-21. [Google Scholar][CrossRef]
- Zannoni VG, Lomtevas N, Goldfinger S. Oxidation of homogentisic acid to ochronotic pigment in connective tissue. Biochim Biophys Acta 1969;177: 94-105 [Google Scholar][CrossRef]
- Lorenzini S, Mannoni A, Selvi E et al. Alkaptonuria. N Engl J Med. 2003; 348(14):1408. [Google Scholar][CrossRef]
- Aydogdu S, Cullu E, Ozsoy MG, et al. Cementless total knee arthroplasty in ochronotic arthropathy: a case report with four-year follow-up. J Arthroplasty 2000;15:539-43. [Google Scholar][CrossRef]
- Carrier DA, Harris CM. Bilateral hip and bilateral knee arthroplasties in a patient with ochronotic arthropathy. Orthop Rev 1990;19:1005-9. [Google Scholar][CrossRef]
- Dom K, Pittevils T. Ochronotic arthropathy, the black hip: case report and review of the literature. Acta Orthop Belg 1997;63:122-5. [Google Scholar][CrossRef]
- Emel E, Karagoz F, Aydin IH, et al. Alkaptonuria with lumbar disc herniation: a report of two cases. Spine 2000;25:2141-4. [Google Scholar][CrossRef]
- Suzuki Y, Oda K, Yoshikawa Y et al. A novel therapeutic trial of homogentisic aciduria in a murine model of alkaptonuria. J Hum Genet 1999;44:74-9. [Google Scholar][CrossRef]
- La Du Jr BN. Are we ready to try to cure alkaptonuria? Am J Hum Genet Apr 1998;62(4):765-7 [GoogleScholar][CrossRef]




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.