A rare case of osteoblastoma body of talus treated with curettage, bone grafting and talo-navicular arthrodhesis
Received: 29-Apr-2021 Accepted Date: May 26, 2021 ; Published: 11-Jun-2021, DOI: 10.37532/1897-2276.2021.16(1).21
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Jaffe’s definition for benign osteoblastoma is a rare bone neoplasm characterized by vascular osteoid and a bone-forming matrix rich in osteoblast. It’s a rare benign locally aggressive osteoblastic lesion of the bone with a very low risk of becoming cancerous.
Case Report: In this case, a twenty-three-year-old man complained of difficulty in walking and pain that had been interfering with his everyday activities for a year. A palpable mass was present on inspection, and an X-ray revealed an enlarged lytic lesion in the talar body involving articular cartilage. Wide excision, bone grafting, and talo-navicular fusion with cannulated cancellous screw fixation were used to treat it. Osteoblastoma is verified by histopathology. Patient was on non-weight bearing with a below-knee cast for six weeks, followed by three months of partial weight-bearing. After six months, the patient had a satisfactory range of motion and was able to bear full weight. Symptoms were relieved, and there was no sign of recurrence after a year.
Conclusion: The better treatment option for osteoblastoma of the talus is surgical wide excision and talo-navicular fusion with cannulated cancellous screw fixation and bone grafting.
Keywords
Osteoblastoma, cartilage, osteoblast, bone grafting
Introduction
Jaffe coined the term benign osteoblastoma to describe a rare bone neoplasm characterised by vascular osteoid and a bone-forming matrix rich in osteoblasts [1,2]. In the Mayo Clinic sequence, this represents less than 1% of all bone tumors [1]. Osteoblastoma is a non-malignant bone tumor that most often affects the spine and long tubular bones. The talus is rarely involved, and when present it is located in the neck of the talus [3]. The second decade of life seems to have the highest occurrence [1,4]. The tumor progresses slowly, and symptoms can last for up to two years before a diagnosis is made. Aneurysmal bone cyst and osteoid-osteoma are two other possibilities [1]. Osteoblastoma is a lytic lesion with matrix ossification and moderate surrounding sclerosis that originates in the medulla of bones [5]. Osteoblastoma is diagnosed using a combination of histological, clinical, and radiological characteristics. Surgery is the only curative cure for osteoblastoma patients. Depending on the clinical condition, position inside the bone, and suspicion of malignancy, the lesion may be removed with intra lesional curettage or wide resection. The surgical method affects recurrence rates, and wide resection is linked to lower recurrence rates [6]. The aim of this paper is to describe a rare case that was successfully treated with wide resection and bone grafting with talonavicular arthrodesis.
Case Report
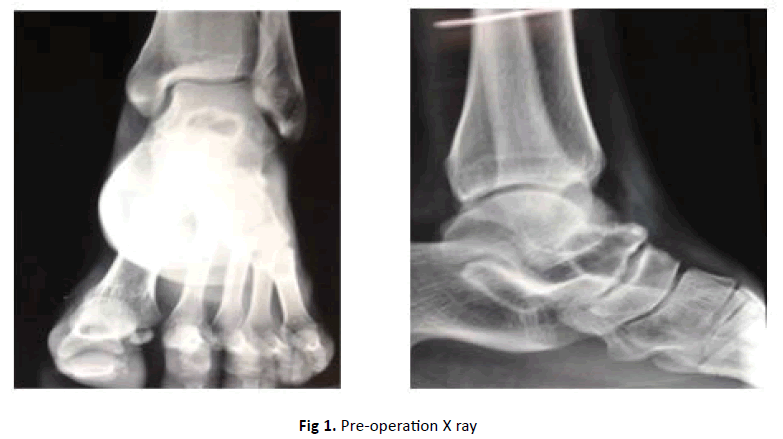
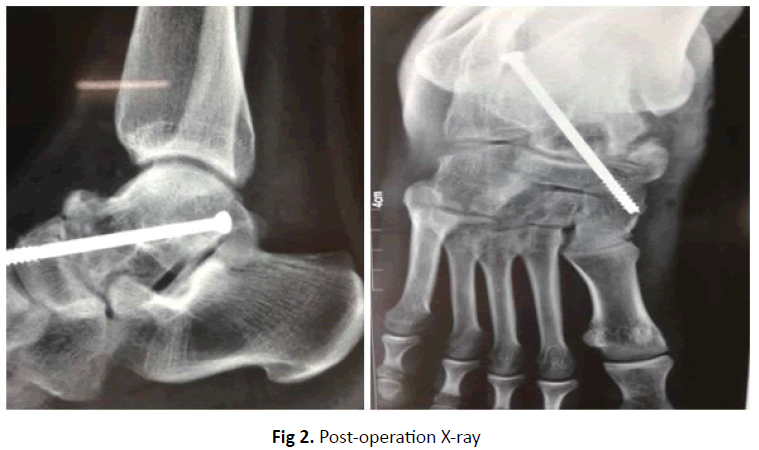
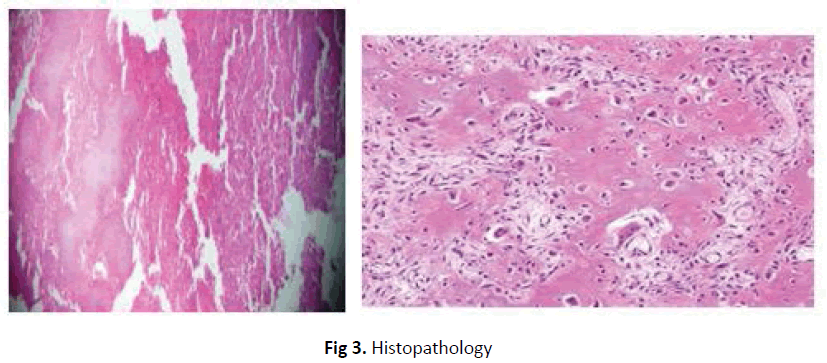
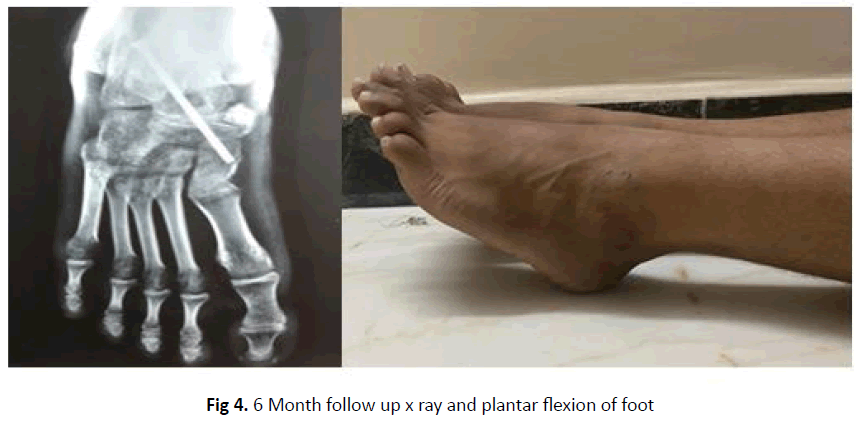
Since one year, a 23-year-old male patient has complained of pain in his right ankle and difficulty in walking. The pain was subtle, progressively worsening, sporadic, aggravated by walking and ankle movements, and relieved by rest and analgesics. It was interfering with his day-to-day routine. There hasn’t been any swelling in the past, and there aren’t any constitutional signs. Tenderness is present over the anterior part of the talus on examination. The subtalar and mid tarsal joints terminal movements are restricted and painful. The results of the laboratory studies were normal. An extended lytic lesion involving articular cartilage, thin shell of periosteal bone, clear zone of transition, and a sclerotic rim was seen on X-ray of the ankle joint, measuring about 3 × 3 cm in the talar neck body junction, involving articular cartilage, with thin shell of periosteal bone, clear zone of transition, and sclerotic rim (Figure 1). Broad excision biopsy, ipsilateral Ilium bone grafting, and talo-navicular fusion with cannulated cancellous screw fixation were all planned for the patient. Histopathology of the biopsy material revealed irregular spicules of mineralized bone and eosinophilic osteoid rimmed by osteoblasts. Pleomorphic spindle cells are found in the vascular stroma. Osteoblastoma talus is confirmed when tumor cells divide into osteoblasts, which produce varying quantities of osteoid and woven bone. For six weeks after surgery, a below knee cast was used with non-weight bearing mobilization. At the seventh post-operative week, the cast was removed. Partially weight-bearing mobilization was done over the course of seven to eighteen weeks after surgery (Figure 2). Active and passive movements of the ankle and subtalar joint were also performed. At the end of six months, the patient was able to bear full weight without discomfort and had adequate ankle and subtalar movements. With a one-year follow-up, there were no recurrences of illness (Figure 3 and 4).
Discussion
Jaffe and Mayer published a detailed study on a metacarpal bone with osteoid and bone-forming tumor in 1932. In 1952, Lichtenstein coined the term osteogenic fibroma to describe a group of tumors with active osseous proliferation and osteoclastic resorption and remodeling in a highly vascular connective-tissue stroma. Golding and Sissons described two cases of osteogenic fibroma involving the vertebral column in 1954. In a systematic study published in 1956, Jaffe objected to the term osteogenic fibroma and called for the term benign osteoblastoma, which was later adopted [4]. Pain is the most common reporting symptom in clinical practise. The pain worsens over time and has a variable response to anti-inflammatory medications [7]. In their seven case series analysis of osteoblastoma of the talus, Rodolfo Capanna M.D. et al found that all of the patients had symptoms for at least a year, with pain in and around the talus not especially increasing at night [8]. We have a common medical history and test results. The lesion was lytic and measured 2 × 3 cm in diameter, with a sclerotic rim. Aneurysmal bone cyst and osteoid osteoma are two possible diagnoses [1]. Since osteoblastoma and osteoid-osteoma are both variants of the same pathologic procedure, radiological diagnosis of a diameter greater than 2 cm is called osteoblastoma [8]. Nicholas and Jack concluded that without histopathological studies of the material, it is practically impossible to diagnose benign osteoblastoma [4]. Extensive curettage or resection is used to treat the condition. It’s possible that the defect would need bone grafting [1]. According to Nicholas and Jack’s case study, curettement of small to moderate lesions accompanied by filling the defect with bone chips appears to be the preferred treatment. One of six patients who underwent marginal excision and two of eleven patients who underwent intra lesional curettage experienced recurrence. In their series, the average recurrence rate was 10%. They concluded that where anatomically necessary, wide resection should be included in the care of patients with osteoblastoma [6]. No malignant transformation or metastases of these lesions have been identified, according to Carol Det al. These tumors, on the other hand, are more likely to recur after incomplete or intra-lesional excision. Perform a total or marginal excision wherever possible. Up to 15% of patients experience recurrence after incomplete intralesional curettage [7]. In our case, wide excision of the tumour was performed, followed by the filling of the gap with bone graft and skeletal stabilisation with talonavicular arthrodesis with cannulated cancellous screw fixation. For confirmation of the diagnosis, the resected portion was sent for histopathological review. Despite the fact that the attachment screw is a little longer and violates the navicular-cuneiform joint, the patient reports no irritation or pain. Hardware was supposed to be taken out at a later time. The majority of authors advise against radiation therapy unless it is appropriate for symptomatic inoperable lesions such as those in the spine.
Conclusion
Osteoblastoma of the talus is a rare benign tumor that causes persistent pain in and around the talus. It tends to develop in the second decade of life. Radiology reveals a lytic lesion with a diameter of more than 2 cm. Broad resection with reconstruction should be performed if it is suspected and anatomically necessary for a good outcome, and the condition can only be verified by histopathological analysis of the material.
Conflict of Interest
No Conflict of Interest.
REFERENCES
- Robert K. Heck Jr. Benign: Aggressive Tumors of Bone. In: Canale&Beaty: Campbell’s Operative Orthopaedics, 11th ed. 2008, p. 892.
- Jafie H.L.: Benign osteoblastoma. Bull Hosp Joint Dis. 1956;18:141-151.
- Mir N.A., Baba A.N., Maajid S., et al.: Osteoblastoma of body of the talus-Report of a rare case with atypical radiological features. Foot Ankle Surg. 2010;16:e24-26.
- Giannestras N.J., Diamond J.R.: Benign osteoblastoma of the talus: a review of the literature and report of a case. J Bone Joint Surg. 1958;40:469-478.
- Kroon H.M., Schurmans J.: Osteoblastoma: clinical and radiologic findings in 98 new cases. Radiology. 1990;175:783-790.
- Saglik Y., Atalar H., Yildiz Y., et al.: Surgical treatment of osteoblastoma: a report of 20 cases. Acta Orthopaedica Belgica. 2007;73:747.
- Morris CD, Lee FY, Gebhardt MC.: Benign Bone Tumors. In: Chapman, Michael W: Chapman’s Orthopaedic Surgery. 3rd Edition. 2001, p. 3386-3389.
- Capanna R., Van Horn J.R., Ayala A., et al.: Osteoid osteoma and osteoblastoma of the talus. Skeletal radiology. 1986;15:360-364.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.