A prospective study of clinico-radiological outcome assessment in intertrochanteric fracture treated with proximal femoral nail
Sir HN Reliance Foundation Hospital and Research Centre, Mumbai, India
Received: 28-Jan-2022, Manuscript No. 22-51971-M; Editor assigned: 02-Feb-2022, Pre QC No. 22-51971-P; Accepted Date: Feb 24, 2022 ; Reviewed: 08-Feb-2022 QC No. 22-51971-QC; Revised: 15-Feb-2022, Manuscript No. 22-51971-R; Published: 25-Feb-2022, DOI: 10.37532/1897-2276.2022.17(1).67
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Purpose: Intertrochanteric fractures of proximal femur are commonly encountered in elderly individuals due to porotic and weak bones. Surgical management such as dynamic hip screw, gamma nail, condylar plates are routinely used but the outcome is very poor. In this backdrop, the present study was carried out to evaluate the clinical and radiological outcome of Proximal Femoral Nail (PFN) in the treatment of intertrochanteric fractures.
Methods: A prospective study was carried on 45 patients with stable intertrochanteric fractures visiting our hospital for a period of two years. The patients were surgical treated PFN and subsequent follow was done upto a period of 3 months. The clinical and functional outcome was analyzed using Tip Apex Distance (TAD), Cleveland Index and Palmer and Parker score.
Results: The mean surgical time was 62.56 ± 8.02 minutes. Out of 45 patient 40 had fracture union and 1 patient had infection and non-union and 1 patient had delayed union. Screw cut out was observed in 5 patients and 1 patient had screw migration to joint. The mean Cleveland index was 6.04 ± 1.05 and TAD was 23.8 ± 2.16 mm at different post-operative periods. Further there was a significant improvement in Palmer and Parker score from 6 weeks to 3 months post-operative (p=0.000).
Conclusion: Proximal femoral is a safe and effective implant for the intertrochanteric fracture fixation in elderly population. Further, the intraoperative blood loss is very minimal with less complication, good union and lesser surgical time.
Keywords
Intertrochanteric fracture, PFN, tip apex distance, Cleveland index, Palmer and Parker score
Introduction
Intertrochanteric fracture is the most prevalent hip fracture documented in middle aged and elderly population [1]. With the rampant increase in the global aging population, the incidence of intertrochanteric fractures is increasing substantially [2]. The global incidence of hip fractures is estimated to rise to 2.6 million by 2025 and further reach 4.5 million by 2050 approximately [3]. Conservative management for intertrochanteric fractures encompasses bed rest for longer period and it may impose wide range of adverse complications such as pneumonia, urinary infections, deep venous thromboses, and pressure sores. In addition, the clinical outcome of conservative management is not satisfactory with a poor prognosis and the one year mortality rate is around 20-30% [4,5]. Surgical management such as Dynamic Hip Screw (DHS), gamma nail, condylar plates are routinely used but the outcome is moderate to poor in terms of surgical time and complications [6]. The treatment strategy for osteosynthesis encompasses open/closed reduction and surface implants fixation Intramedullary (IM) implants such as Proximal Femoral Nail (PFN) [7,8].During the period between 1999- 2010, mounting studies including Cochrane reviews recommended the use of DHS or the sliding Hip screw for stable intertrochanteric fracture and in the case of unstable fractures IM are highlighted [8,9]. However, recently majority of the studies and Cochrane reviews documented the use of PFN for stable as well as unstable intertrochanteric fracture [10,11]. Thus an ideal surgical technique must possess less surgical time, intra operative adverse events, blood loss and post-operative morbidity and mortality. Further, there should be minimal anaesthesia risk, length of hospital stay and healthcare cost. In addition the surgery must allow the patient out of bed at the earliest to minify various bed ridden adverse complications bed sores, pulmonary complications etc. In this backdrop, the present study was carried out to evaluate the clinical and functional outcome of intertrochanteric fractures treated with PFN.
Method
STUDY SETTING
This was a prospective study conducted on 45 patients diagnosed with intertrochanteric fractures and treated with Proximal Femur Nail (PFN) at the Department of Orthopaedics in our hospital for a period of two years.
INCLUSION CRITERIA
Patients with age ranging between 18-90 years, with intertrochanteric fractures and patients undergoing primary or index surgery were enrolled in the study.
EXCLUSION CRITERIA
Patients with fractures due to various pathological causes, previous surgical history in proximal femur, unstable intertrochanteric femur fracture treated with wide range of internal fixation methods and previous non-unions and malunions were excluded from the study.
SURGICAL PROCEDURE
The patient was positioned on the fracture table and hip was kept at slight adduction position for the nail insertion. A 5cm skin incision was done at 5cm cranial to the tip of greater trochanter. The fascia and muscles were passed and then 2.8 mm threaded K-wire was inserted at the greater trochanter tip under the C-arm control. Further, K-wire was moved to the femoral shaft so that it positioned at the shaft center in both the directions. The proximal portion of femoral shaft was reamed with 17 mm reamer, manually. The nail with a size of 240 mm with distal femoral canal diameter 10 mm, 11 mm, 12 mm options was mounted radiolucent insertion device and then inserted manually to the femoral shaft. With the help of aiming arm in the insertion device, the guide wire for the neck screw with self-tapping, 11.0 mm screw; length 80 mm-120 mm was initially placed into the femoral neck so that the screw was positioned at lower portion of the neck when viewed anteroposteriorly and at center when viewed laterally. Then, the guide wire for the anti-rotational hip pin was placed. Initially, the hip pin was introduced with 25 mm medial at the tip of fracture line and further the neck screws were placed. Next, based on the fracture type distal interlocking using 4.9 mm locking bolt with length of 26 mm-52 mm based on the choice of static and dynamic locking was done statically or dynamically in the same aiming arm. All the study participants received low molecular weight heparin for anti-thrombolytic prophylaxis followed by antibiotic. Anteroposterior and lateral x-rays were taken after 24-72 hours of postoperative period and evaluated for the reduction and implant position. The rehabilitation protocol was explained to the patients and they were allowed to mobilize on the 1st post-operative day. Partial, tolerated or restricted weight was instructed to the patients based on the condition on the immediate day of postoperative.
PRE-OPERATIVE ASSESSMENT
Radiograph of pelvis with both hip and full length femur of fracture side was taken for comparison with post-operative x-ray.
IMMEDIATE POST-OPERATIVE ASSESSMENT
Radiograph of pelvis with both hip and anteroposterior and lateral views of operated femur was taken immediate post-operative period and then the tip apex distance and Cleveland index were calculated.
POSTOPERATIVE FOLLOW UP
Singh’s index was used to assess osteoporosis. X-ray radiograph of pelvis with both hip and anteroposterior and lateral views of operated femur was taken after 6 weeks and 3 months-Tip Apex Distance, Cleveland Index were calculated and compared to immediate post-operative findings. Clinical assessment was evaluated with Palmer and Parker score at 6 weeks and 3 months.
DATA ANALYSIS
The data were analyzed using student’s t-test and Mann-Whitney test. A p-value <0.05 was considered as statistically significant. The analysis was done using SPSS, version 23.
Results
In this study, out of 45 patients, the mean age was 69.51 ± 14.74 years. Male and females were equally involved, occurrence of Boyd and Griffin type 1 fracture was observed in 55% of patients, right side was commonly involved in 68.9% of patients, 5(11.1%) patient displayed screw cut-out, 1(2.2%) has screw migration into the joint, 1(2.2%) had infection nonunion. In 97% of patient fracture reduction was achieved by closed reduction and the average surgical time was 62.5 ± 8.02 minutes (Table 1).
Table 1. Demographics and clinical variables of the study population (n=45)
| Variable | N (%) | |
|---|---|---|
| Age | Mean(SD) | 69.51(14.747) |
| Gender | Male | 22(48.9%) |
| Female | 23(51.1%) | |
| Type of fracture | I | 25(55%) |
| II | 18(40%) | |
| III | 2(4.4%) | |
| Side of fracture | Left | 14(31.1%) |
| Right | 31(68.9%) | |
| Local Complications | None | 38(84.4%) |
| Infection non-union | 1(2.2%) | |
| Screw cutout | 5(11.1%) | |
| Screw migration to joint | 1(2.2%) | |
| Type of reduction | Closed reduction | 44(97.8%) |
| Open reduction | 1(2.2%) | |
| Time procedure in mins | (SD) | 62.56(8.021) |
In our study, the median Singh’s index score was 3 and in 53.3% of the patients the score was <3 and in 46.7% the score was >3.
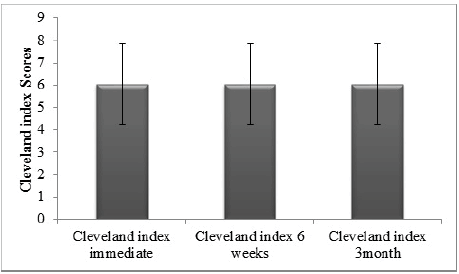
In this study, there was no significant difference in the Cleveland index between immediate, 6 weeks and 3 months post-operative and it was revealed that the screws were in same quadrant. The results were shown in figure 1.
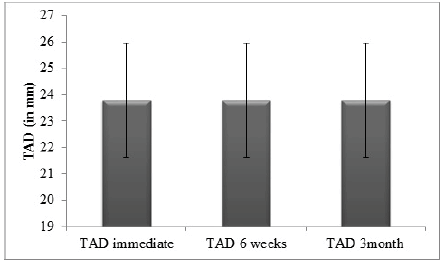
1. In this study, there was no significant difference in the Tip-Apex Distance (TAD) between immediate, 6 weeks and 3 months postoperative and it was revealed that the distance were the same. The results were shown in figure 2.
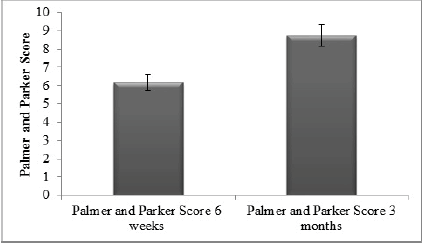
2. Further, there was a significant (p=0.000) improvement of palmer and parker score in 3months post-operative as compared to 3 weeks post-operative. The results were shown in figure 3.
Discussion
Intertrochanteric fracture in elderly imposes a significant challenge among the orthopaedic surgeons since there involved a various associated co-morbidities in these set of patients. An ideal surgical technique must possess the following merits such as less surgical time, blood loss, intra-operative complications and post-operative morbidity and mortality. Further, there should be minimal anesthesia risk, reduced length hospital stay and low healthcare cost. Further, it also important that there should be early mobilization of the patients to prevent the complications such as bed sores, pulmonary consequences and deep vein thrombosis [12]. Effective management of intertrochanteric fractures relies on surgeon independent variables such as quality of bone, pattern of fracture and fracture stability. In addition, surgeon dependent variables such as quality of fracture reduction and type and implant placement also have significant impact better treatment outcome [13].
Dynamic Hip Screw (DHS) is the hallmark gold standard methods for the management of stable intertrochanteric fracture fixation over a period of years [14]. However, due to implant related complications in the DHS, the PFN was considered since being an intramedullary implant it elicit minimal bending moment, gives an additional support to medial column and also serves as a buttress thus preventing in shaft medialization [15]. The main important merit of PFN is that the two proximal screws elicit lesser diameter and it provides good rotational control of proximal fracture fragment.
The mean age of the patients in the present study was found to be 69.51years. Our results are in corroboration with the previous study done by Sharma et al. [16] with a men age of 60.78 years. In our study the median surgery duration was 62.56 minutes. Post-operative infection was seen in 1 (2.2%) patients and needed change of antibiotics and debridement and dressings, while 5 (11.1%) patients has screw cut out, while 1 (2.2%) has screw migration in to the joint. Majority of patients were discharged by 5th post-operative day, only a few needed longer stay due to infection, any associated injuries or medical illness, which required further management or observation or both. A recent meta-analysis done by Kumar et al. [16] shows that PFN is a significant faster surgery methods and the intra operative blood loss has been very minimal. Further they also reported that it improves the patient wellbeing and mental health as evident by good Harris hip scores and lesser duration of hospital stay.
In our study, partial weight bearing is allowed within 3-6 weeks post operatively in patients with stable internal fixation without any comorbidity. Further, complete weight bearing is allowed within 12 weeks in most of the cases based on the stability of fixation, degree of comminution, amount of osteoporosis, age of the patient and radiological union. Load bearing capability of proximal femur is mainly mediated by calcar femoral and in the case of DHS in lever arm of laterally placed plate is elevated, which increases the chance of implant screw cut out. However in the case of PFN it decreases the bending force of the hip joint on implant by 25%-30%. Thus, in elderly patients treated with PFN has an advantage of early weight bearing mobilization [12].
Cleveland index and TAD has significant correlation with union of intertrochanteric fracture and significantly affecting the Palmer and Parker score .TAD of <25mm and Cleveland index of (5,6,8,9) quadrant has significant correlation in union of intertrochanteric fracture [18]. In our study both the Cleveland index and TAD are within the acceptable range but it was not significant when compared at different post-operative periods.
The Parker and Palmer score is a new method for evaluating the mobility in hip fracture patients. Mounting studies have shown that it is a reliable predictor for evaluating the in-hospital patient rehabilitation and various post-operative periods [19,20]. Further, the Parker and Palmer score is also useful to measure the patients mobility in indoors, outdoors and used to measure the outcome and also to predict the mortality [21]. In our study there was a significant improvement of Parker and Palmer score from 6 weeks to 3 months post-operative.
Conclusion
The proximal femoral nail is an effective implant for the internal fixation of stable intertrochanteric fractures by encouraging stable fixation, near-perfect reduction, early weight bearing and ambulation, decreased hospital stay and increased union rate with restoration of independent daily activities.
REFERENCES
- Cooper Tucker A., et al.: Is the best plate a nail? A review of 3230 unstable intertrochanteric fractures of the proximal femur. J Orthop Trauma. 2018;32:53-60.
- Lindskog D.M., Baumgaertner M.R.: Unstable intertrochanteric hip fractures in the elderly. J Am Acad Orthop Surg. 2004;12:179-190.
- Yang Q.H., et al.: Geographic variations in intertrochanteric femoral fractures in China. Biomed Res Int. 2019;2019:8396723.
[CrossRef ] [Google Scholar]
- Yoo J.I., et al.: Early rehabilitation in elderly after arthroplasty versus internal fixation for unstable intertrochanteric fractures of femur: systematic review and meta-analysis. J Korean Med Sci. 2017;32:858-867.
- Dyer S.M., et al.: A critical review of the long-term disability outcomes following hip fracture. Innov Aging. 2017;1:736.
- Ceynowa M., et al.: The early failure of the gamma nail and the dynamic hip screw in femurs with a wide medullary canal: A biomechanical study of intertrochanteric fractures. Clin Biomech. 2020;71:201-207.
- Lenich A., et al.: Clinical comparison of the second and third generation of intramedullary devices for trochanteric fractures of the hip-blade vs screw. Injury. 2010;41:1292-1296.
- Sadowski C., et al.: Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am. 2002;84:372-381. [CrossRef]
- Anglen J.O., Weinstein J.N.: Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice: A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008;90:700-707.
- Sanders D., et al.: A Multicentre randomized control trial comparing a novel intramedullary device (InterTAN) versus conventional treatment (sliding hip screw) of geriatric hip fractures. J Orthop Trauma. 2017;31:1-8.
- Unsay J.C., Chua T.H.I., KwekBengKee E.: Early experience with the trochanteric fixation nail-advanced (TFN-A): A descriptive review of thirty-four cases from a single center. Indian J Orthop. 2020;54:246-253.
- Özkayın N., Okçu G., Aktuğlu K.: Intertrochanteric femur fractures in the elderly treated with either proximal femur nailing or hemiarthroplasty: A prospective randomised clinical study. Injury. 2015;46:S3-S8.
- Sheehan S.E., et al.: Proximal femoral fractures: What the orthopedic surgeon wants to know. Radiographics. 2015;35:1563-1584.
- Jensen J.S., Sonne-Holm S., Tøndevold E.: Unstable trochanteric fractures: A comparative analysis of four methods of internal fixation. Acta Orthop Scand. 1980;51:949-962.
- Kulkarni G.S., et al.: Intertrochanteric fractures. Indian J Orthop. 2006;40:16-23.
- Sharma A., Mahajan A., John B.: A Comparison of the clinico-radiological outcomes with Proximal Femoral Nail (PFN) and Proximal Femoral Nail Antirotation (PFNA) in fixation of unstable intertrochanteric fractures. J Clin Diagn Res. 2017;11:RC05-RC09.
- Kumar P., et al.: Proximal femoral nailing is superior to hemiarthroplasty in AO/OTA A2 and A3 intertrochanteric femur fractures in the elderly: a systematic literature review and meta-analysis. Int Orthop. 2020;44:623-633.
- John B., et al.: Tip-apex distance and other predictors of outcome in cephalomedullary nailing of unstable trochanteric fractures. J Clin Orthop Trauma. 2019;10:S88-S94.
- Parker M.J., Palmer C.R.: A new mobility scores for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993;75:797-798.[CrossRef] [Google Scholar]
- Kristensen M.T., et al.: High inter-tester reliability of the new mobility score in patients with hip fracture. J Rehabil Med. 2008;40:589-591.
- Kristensen M.T., et al.: Prefracture functional level evaluated by the new mobility score predicts in-hospital outcome after hip fracture surgery. Acta Orthop. 2010;81:296-302.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.