A new classification for the valgus knee related to total knee arthroplasty and implant selection
Received: 05-Jun-2020 Accepted Date: Jul 17, 2020 ; Published: 27-Jul-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: We propose a novel classification for valgus knee deformity related to total knee arthroplasty, developed by evaluation of conventional and stress radiographs, clinical examination and a retrospective level 2 analysis of the implants selected for the treatment of valgus knees in a single institution.
Methods: This study includes the analysis of 335 total knee arthroplasties evaluated with AP standing and stress radiographs and clinical examination. The anatomical knee axis and the radiographs were measured by 2 different knee surgeons to determine the interobserver reliability.
Results: This new classification of valgus knees, focused on joint wear, stability and ligament sufficiency was developed in order to understand and define the knee types and relate them to the implant that should be utilized.
Conclusion: This new classification allows for better understanding of valgus knee deformities, defining ligament status and valgus types, and it seems to be a comprehensive tool for preoperative planning and the choice of prosthetic constraint. Constrained implants should be used in cases with coronal instability with attenuated medial collateral ligament. Rotating hinges must be reserved for medial collateral ligament incompetence, associated significant recurvatum, multidirectional instability and/or severe muscular deficiency.
Keywords
severe valgus knee, ligament incompetence, attenuated MCL
Introduction
Coronal alignment is a key factor in knee replacement surgery, both preoperatively to describe the deformity and postoperatively to asses correction [1]. The incidence of valgus deformity may range from 10 to 40% [1,2]. In a severe valgus knee (>20°), it is important to consider that they may present a coronal, sagittal or multidirectional instability with or without variable degrees of Medial Collateral Ligament (MCL) insufficiency [2-9].
Evaluation of collateral ligament competence in the physical and radiological preoperative examination [10,11] will allow to define the prosthetic type and to identify the patients that may require an implant with increased stability (superior to a posterior stabilized) in a primary TKA [11,12], since a standard implant may fail to achieve a stable knee in the short or medium term [3,7,13,14].
Constrained knee prosthesis presents a polyethylene liner with a higher and wider central post which fits more snugly in the intercondylar space, generating more sagittal and coronal stability [10,15]. Femoral and tibial components are not linked, allowing complete axial and 2º to 3º of rotational motion [10]. However, this central post is not designed to support complete varus/valgus strain load in the long term, so collateral ligaments must have some degree of sufficiency when this design is used [15,16].
Rotating hinges are mechanically stable in all directions since the tibial and femoral components are linked through an axis that restricts the rotation and translation in the coronal and sagittal planes. These implants do not need any type of ligament sufficiency [17-19].
Nevertheless, in the medium and long term, the use of constrained implants implies potential complications such as increased wear, breakage of stabilization mechanisms and risk of mechanical loosening due to higher stress transmission [15,16,19,20]. Therefore, it is important to understand the specific indication of these implants to ensure that they are only used when it is strictly necessary.
The Krackow classification [4-6], the most widely used, has 3 valgus knee types:
• Type 1: Minimum valgus deformity with lateral compartment bone defect, lateral retraction and medial indemnity of the soft tissues
• Type 2: Valgus knee with medial collateral ligament clearly attenuated
• Type 3: Severe valgus knee associated to a valgus tibial osteotomy sequel
This classification, focused on the valgus knee that needs an arthroplasty with some degree of complexity, was outlined at a time when the concepts for the treatment of the severe valgus knee were not yet clearly defined. It does not include the less severe valgus deformities and it does not really help surgeons foresee potential technical difficulties during surgery nor select the appropriate implant.
The purpose of this retrospective study on a wide variety of primary replaced valgus knees is to characterize the different degrees of valgus knee joint wear and ligament status, in order to propose a novel classification through a simple and reproducible method. This classification tries to help surgeons better understand the valgus knee pathology and its impact in implant selection.
Materials and Methods
Between January 2009 and January 2018, 1378 primary TKA were performed in our institution, 335 (24%) due to a valgus deformity. A Posterior Stabilized (PS) prosthesis was used in 301 knees (including 24 PFC Sigma PlusTM, DePuyTM, J and JTM, Warsaw, USA), a constrained implant was used in 17 knees and a rotating hinge in another 17. The minimum follow was of 2 years.
There were 214 females (64%) and 121 males (36%), with an average age of 70.1 years (40 to 87 years) and an average follow up of 6.3 years (2 to 12 years).
Physical examination and X Rays were performed 6 weeks, 3 and 6 months after surgery, and then annually.
The Knee Society Score (KSS) [21,22] was used to evaluate outcomes at 1 year.
Revision surgery was considered as a treatment failure.
Patient and X Ray Evaluation
In the preoperatory examination we evaluate stability and wear of the knee joint, Range of Motion (ROM), ligament sufficiency and type and magnitude of knee deformity.
Collateral ligament sufficiency was examined with stress clinical maneuvers and standing AP and stress AP (with the knee in full extension as an easy and reproductible method) X Rays since physical evaluation can underestimate ligament insufficiency [12].
Two observers who measured the AP and stress radiographs performed the measurements for each patient.
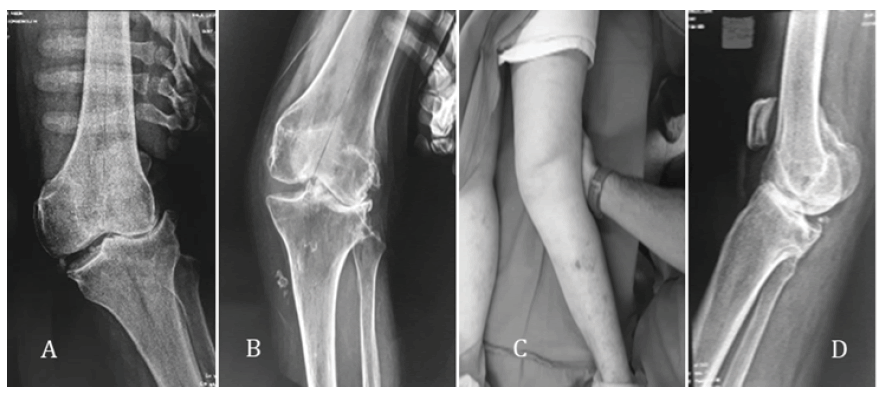
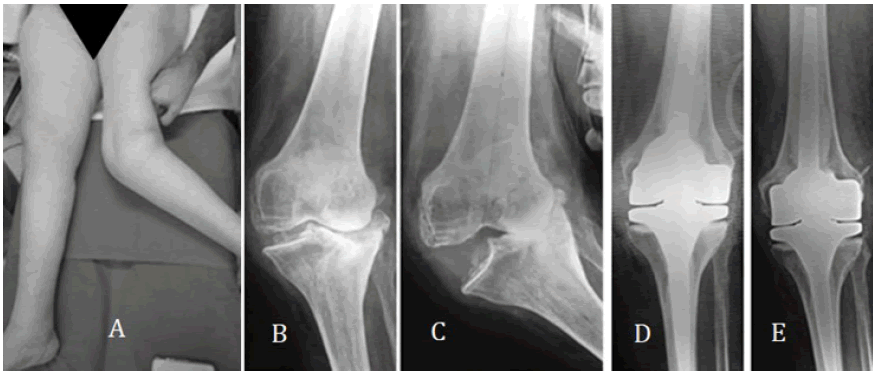
The MCL was considered sufficient when in the stress maneuver the joint deformity did not increase (Fig. 1A) while it was considered attenuated when the deformity increased but with a clear mechanical stop (Fig. 1B and 1C). Finally, the MCL was considered incompetent when the stress maneuver increased the deformity like a hinge, without a clear stop (Fig. 2).
Results
The interobserver accuracy was 2° as measured by 50 consecutive measurements at the start of the study. The interobserver reliability of the classification was measured using the Cronbach method and a Cronbach score of 0.90 was obtained.
Proposed Classification
The valgus knee was classified in 5 types considering joint wear, knee deformity, ligament sufficiency and joint stability.
• Type 1: Narrowing<50% of the lateral compartment.
• Type 2: Narrowing>50% of the lateral compartment, with a valgus knee of less than 20°
• Type 3: Valgus knee>20° with sufficient MCL
• Type 4: Valgus knee with attenuated MCL
• Type 5: Valgus knee of any angular deformity with incompetent MCL and/or recurvatum over 10° (Fig. 1C)
Any of these can be described with or without associated bone defects.
For the proposed classification, the radiological projections recommended to evaluate the knee should be: The AP, lateral and standing AP views are mandatory, using the stress AP view only when an attenuated or incompetent MCL is suspected at the physical examination.
There were 38 type 1 knees, all treated with a PS prosthesis, with an average anatomical axis of 9° (6°-11°).
239 knees were classified as type 2, with an average anatomical axis of 11° (7°-18°), and all were treated with a PS prosthesis.
There were 23 type 3 knees, all treated with PFC Sigma PlusTM prosthesis (DePuyTM, J and JTM, Warsaw, USA), with an average anatomical axis of 23° (20°-28°).
There were 24 type 4 knees, with an average anatomical axis of 23.4° A new classification for the valgus knee related to total knee arthroplasty and implant selection (17°-37°). 17 were treated with a constrained prosthesis, 6 with a rotating hinge and 1 with a PFC Sigma PlusTM.
And 11 knees were classified as type 5, with an average anatomical axis of 27° (17°-55°), all treated with a rotational hinge prosthesis. Eight patients presented an incompetent MCL (two with rheumatoid arthritis) and three had a severe valgus knee associated to a recurvatum deformity of 10°, 15° and 26° and a neuromuscular disorder of the limb.
The average PO anatomical axis was of 4.3° of valgus (0° to 9°).
Prosthetic survival at the end of the average 6.3 year follow up was 99% (3 revisions due to acute infection).
Discussion
The term attenuated was first used by Krackow [5] in 1991 to describe MCL partial insufficiency but over the years this term became confusing. Understanding the knee joint ligament status previous to a TKA is the key for understanding the degree and type of joint injury, defining ligament sufficiency, attenuation or incompetence and thus, defining the type of knee and the recommended implant.
Krackow’s classification [4-6,22] does not contemplate the mild valgus deformities, as it focuses on those knees which required a TKR almost 30 years ago, and is clearly related to the technical challenges at that time. Krackow [4] includes in the Type 2 knees of his classification those with attenuated and incompetent MCL, using both terms as the same.
Ranawat [2], instead, makes a clear differentiation and classifies knees with incompetent MCL in Type 3, but despite being complementary, its contribution does not make a substantial difference.
Krackow’s classification is thus incomplete as it neither includes all types of valgus knees nor clearly defines the ligament status of each type. Moreover, it unnecessarily associates valgus osteotomy as a key factor, it does not include recurvatum as a critical issue and it fails to clearly differentiate between ligament attenuation and incompetence. There even are, in the existing publications, different descriptions of Krackow’s classification, as sometimes ligament incompetence is included in Type 2 [4,5,23,24], and others in Type 3 [2].
A complete classification must consider all the valgus knee characteristics that are relevant for the arthroplasty surgery, including the severity of joint wear, ligament sufficiency and joint stability. The evaluation of all these aspects is critical in the most severe valgus deformities [3], as they frequently present some degree of MCL insufficiency and therefore a standard PS prosthesis may not be able to achieve a stable knee, particularly in the medium or long term [3,7,14,15].
After analyzing a consecutive series of TKAs on valgus knees, a new classification for knee osteoarthritis with valgus deformity is proposed. This classification intends to help surgeons to properly select the knee implant and its degree of constraint. The classification as well, makes a distinction between a sufficient and an attenuated MCL, which is, to certain extent, subjective, as the palpable pain over the ligament and its apparent clinical and radiographic stretching may be the only aspects tilting the balance in favor of such diagnosis, and the suspicion of ligament attenuation is, precisely, what leads to enhance articular stability with a more constrained prosthesis.
In this series, all the Type 1, 2 and 3 knees (stable joints) were treated with a PS prosthesis (including the 23 type 3 treated with a PFC Sigma PlusTM). This means that all the joints with a sufficient MCL were treated in a similar way (PFC Sigma PlusTM is not considered a constrained implant), independently of the severity of its angular deformity.
Of the 24 knees classified as Type 4, 17 were treated with a constrained prosthesis, 6 with a rotating hinge and 1 with a PFC Sigma PlusTM. All 6 rotating hinges were used by the less experienced surgeon of the group and while it suggests that the surgeon’s experience is related with the type of prosthesis used, there were not enough patients to obtain a statistically significant conclusion.
Anderson et al. [11] reported a series of 55 TKA with a similar followup, using a constrained implant, in patients with a valgus knee>15°, coronal instability and attenuated MCL. Its clinical and functional results were promising and reported no revisions.
Lachiewicz et al. [13] published their experience in 54 patients with an average valgus anatomical axis of 20° and an attenuated MCL, using the TC3TM (DePuyTM, J&JTM, Warsaw, USA) prosthesis with a survival of 96% at 10 years.
In the present study, all the 11 Type 5 knees were treated with a rotating hinge, due to the joint instability.
Bistolfi et al. [25] reported the result in 98 TKA using the rotating Endo ModellTM (Waldemar LinkTM, Hamburg, Germany) prosthesis, with a maximum follow up of 15 years and a prosthetic survival of 79.8% after 10 years. This is an interesting publication because it includes the complications of the use of this type of implants (prosthetic dislocation, breakage of the polyethylene capture mechanism, inadequate cementing of the stems and mechanical loosening).
Kowalczelski et al. [18] presented a series of 12 patients operated with a rotating Endo-ModellTM prosthesis, with an average follow up of 10 years. Although they do not describe the preoperative axis, they remark that the patients presented important deformities with an insufficient MCL.
A common aspect of all these publications is the lack of a clear and common classification of the knee affection. This issue complicates the comparison between prosthetic constraint selection and if it depends on the severity of the valgus deformity, the ligament status or another issue.
The polyethylene central post of the constrained implants is not strong enough to stabilize the knee if the MCL is incompetent, and it may fail in the short term in Type 5 knees [10,15,16,26].
Rotating hinges are mechanically stable in all directions, do not require ligament sufficiency and its use is mandatory to stabilize a knee with ligament incompetence or recurvatum [9,25,27-31].
During the preoperatory physical examination the condition of the collateral ligaments must be evaluated, establishing their status (sufficient, attenuated or incompetent), and documenting the evaluation with stress AP X Rays. Underestimating a ligament insufficiency and using a less constrained implant will lead to an early (if not immediate) failure [30,31].
The correct interpretation of ligament sufficiency will allow not to exceed the degree of constraint of the prosthesis, as in the medium and long terms, the unnecessary use of higher constrained implants exposes the patient to potential complications such as increased wear, breaking of stabilization elements and risk of mechanical loosening [15,16,19,20].
The differentiation between a sufficient, attenuated or an incompetent MCL is essential to comprehensively understand the severe valgus knee, and the correct use of the terminology to define the ligament status is a major issue.
Symptomatic severe valgus knee is a frequent cause of joint replacement. A proper understanding of this pathology will allow us to define the appropriate treatment for each patient.
The limitations of this paper are those corresponding to a retrospective study, with a low number of patients and a limited follow up. Its strengths are that the patients were evaluated and operated in the same institution, with the same preoperatory evaluation, surgical team and technique.
Conclusion
The classification proposed clearly defines the ligament status and valgus knee types, is a simple way of categorizing valgus knee osteoarthritis and it seems to be a comprehensive tool when deciding the knee prosthesis type for each patient and for performing prospective studies.
The design of this study does not allow to categorically define the indications for the use of augmented stability knee prosthesis, but it suggests that constrained prosthesis should be used in coronal instability and attenuated MCL, while rotating hinges should be applied in multidirectional instability with MCL incompetence and/or recurvatum>10° and/or neuromuscular disorders.
Compliance with Ethical Standards
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Funding
Not applicable.
Conflict of Interest
Author Santiago P. Vedoya declares that he has no conflict of interest. Author Hernan del Sel declares that he has no conflict of interest.
REFERENCES
- Thienpont E., Parvizi J.: A new classification for the varus knee. J Arthroplasty. 2016;31:2156-2160.
- Ranawat A.S., Ranawat C.S., Elkus M., et al.: Total knee arthroplasty for severe valgus deformity. JBJS Essent Surg Tech. 2005;87:271-284.
- Girard J., Amzallag M., Pasquier G., et al.; Total knee arthroplasty in valgus knees: Predictive preoperative parameters influencing a constrained design selection. Orthop Traumatol Surg Res. 2009;95:260-266.
- Krackow KA.: The technique of total knee arthroplasty. C.V. Mosby Co;1990.
- Krackow K.A., Jones M.M., Teeny S.M.: Hungerford DS. Primary total knee arthroplasty in patients with fixed valgus deformity. Clin Orthop Relat Res. 1991;9-18.
- Krackow K.A., Mihalko W.M.: Flexion-extension joint gap changes after lateral structure release for valgus deformity correction in total knee arthroplasty: a cadaveric study. J Arthroplasty. 1999;14:994-1004.
- Naudie, Naudie DD, Rorabeck C.H.: Parvici. Managing instability in total knee arthroplasty with constrained and linked implants. Instr Course Lect. 2004;53:207-215.
- Ranawat C.S., Rose H.A., Rich D.S.: Total condylar knee arthroplasty for valgus and combined valgus-flexion deformity of the knee. Instr Course Lect. 1984;33:412-416.
- Vedoya S.P., Garabano G., del Sel H.: Indication and results of the prosthesis with increased stability in primary knee arthroplasty. [Constrained prosthesis primary total knee arthroplasty]. Rev la Asoc Argentina Ortop Y Traumatol. 2018;83:94-100.
- Miyasaka K.C., Ranawat C.S., Mullaji A.: 10- to 20-year followup of total knee arthroplasty for valgus deformities. Clin Orthop Relat Res. 1997;345:29-37.
- Anderson J., Baldini A., MacDonald J., et al.: Constrained condylar knee without stem extensions for difficult primary total knee arthroplasty. J Knee Surg. 2010;20:195-198.
- Hartford J.M., Goodman S.B., Schurman D.J., et al.: Complex primary and revision total knee arthroplasty using the condylar constrained prosthesis: an average 5-year follow-up. J Arthroplasty. 1998;13:380-387.
- Lachiewicz P.F., Soileau E.S.: Ten-year survival and clinical results of constrained components in primary total knee arthroplasty. J Arthroplasty. 2006;21:803-808.
- Lombardi A.V., Berend K.R., Leith J.R, et al.: Posterior-stabilized constrained total knee arthroplasty for complex primary cases. J Bone Jt Surg. 2007;89:90.
- Lachiewicz P.F., Soileau E.S.: Results of a second-generation constrained condylar prosthesis in primary total knee arthroplasty. J Arthroplasty. 2011;26:1228-1231.
- Kim Y.H., Kim J.S.: Revision total knee arthroplasty with use of a constrained condylar knee prosthesis. J Bone Jt Surgery-American Vol. 2009;91:1440-1447.
- Gehrke T., Kendoff D., Haasper C.: The role of hinges in primary total knee replacement. Bone Joint J. 2014;96-B:93-95.
- Kowalczewski J., Marczak D., Synder M., et al.: Primary rotating-hinge total knee arthroplasty: good outcomes at mid-term follow-up. J Arthroplasty. 2014;29:1202-1206.
- Pour A.E., Parvizi J., Slenker N., et al.: Rotating hinged total knee replacement. J Bone Jt Surg. 2007;89:1735-1741.
- Puloski S.K., McCalden R.W., MacDonald S.J. et al.: Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. J Bone Joint Surg Am. 2001;83-A:390-397.
- Ewald F.C.: The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9-12.
- Insall J.N., Dorr L.D., Scott R.D., et al.: Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13-14.
- Favorito P.J., Mihalko W.M., Krackow K.A.: Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg. 10;1:16-24.
- Kim Y.H., Kim J.S., Surgeon O., et al.: Total knee arthroplasty in neuropathic arthropathy. J Bone Jt Surg Br. 2002;84:216-219.
- Bistolfi A., Lustig S., Rosso F.: Results with 98 endo-modell rotating hinge prostheses for primary knee arthroplasty. Orthopedics. 2013;36:e746-e752.
- Petrou G., Petrou H., Tilkeridis C., et al.: Medium-term results with a primary cemented rotating-hinge total knee replacement a 7-to 15-year follow-up. J Bone Jt Surg Br. 2004;86:813-830.
- Cottino U., Abdel M.P., Perry K.I., et al.: Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses. J Bone Jt Surg. 2017;99:324-330.
- Maynard L.M., Sauber T.J., Kostopoulos V.K., et al.: Survival of primary condylar-constrained total knee arthroplasty at a minimum of 7 years. J Arthroplasty. 2014;29:1197-1201.
- Del Sel H., Pablo Vedoya S., Garabano G., et al.: Reemplazo total de rodilla en gonartrosis asociada a deformidad extraarticular. Rev AAOT. 2013;77:178-184.
- Pasquier G., Ehlinger M., Mainard D.: The role of rotating hinge implants in revision total knee arthroplasty. EFORT Open Rev. 2019;4:269-278.
- Kouk S., Rathod P.A., Maheshwari A.V., et al.: Rotating hinge prosthesis for complex revision total knee arthroplasty: A review of the literature. J Clin Orthop Trauma. 2018;9:29-33.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.